Triglycerides (TG)
Other names: Blood lipids, neutral fats, TG, Triglycerides, Trig, TG.
Service code 1072
general information
Triglycerides (TG) are complex fats that enter the body with fatty plant and animal foods and can also be synthesized in the liver. The level of triglycerides in the blood is constantly changing: the highest amount is observed after eating, then it gradually decreases and returns to normal when all the triglycerides are distributed throughout the cells of the body.
TG are deposited in the cells of subcutaneous fat “in reserve”, where they perform a thermal protective function, retaining the heat generated in the body, and also protect internal organs from possible mechanical damage. Triglycerides are the most important source of energy for muscles, since 1 g of fat, when broken down, provides twice as much energy as the same amount of protein or carbohydrate.
When triglyceride metabolism is disrupted, excess fat deposition most often occurs in the subcutaneous tissue and around internal organs—obesity. Increasing triglyceride levels in the body increases the risk of developing cardiovascular diseases and acute pancreatitis.
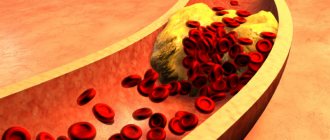
A blood test for triglycerides in combination with cholesterol is used to assess the risk of developing atherosclerosis and cardiovascular diseases, as well as to diagnose hereditary disorders of lipid metabolism.
Important! Triglyceride levels can be significantly elevated (5-10 times) even several hours after eating. Blood values taken on an empty stomach at different times may also be different. Some people experience a 40% change in triglyceride levels within a month. This phenomenon is called biological variation and reflects normal fluctuations in cholesterol metabolism in the body. Thus, a single test does not always reflect “usual” triglyceride levels, so sometimes a retest is required.
A triglyceride test should be taken outside the acute phase of the disease, and after a heart attack or surgery - at least 6 weeks later.
Indications for the purpose of analysis:
- scheduled preventive examination;
- assessing the risk of developing atherosclerosis, heart and vascular problems;
- monitoring the effectiveness of a diet with a reduced amount of animal fats and monitoring blood lipid levels after prescribing drugs that reduce triglycerides and cholesterol;
- diabetes;
- myocardial infarction;
- pancreatitis;
- hereditary disorders of lipid metabolism;
- gout;
- the presence of one or more risk factors for the development of cardiovascular diseases: smoking;
- age (men over 45 years old, women over 55 years old);
- high blood pressure (140/90 mmHg and above);
- coronary heart disease, heart attack or stroke;
- excess body weight;
- alcohol abuse;
- eating large amounts of food containing animal fats;
- low physical activity;
- high cholesterol or cardiovascular disease in other family members (heart attack or stroke in an immediate male relative under 55 years of age or a female relative under 65 years of age).
Research method: homogeneous enzymatic colorimetric method
Analyzer : Cobas 6000
Units: mmol/l
Material for research: venous blood serum
Recommendations for preparing for analysis:
- take on an empty stomach, after sleep;
- stop eating 8-12 hours before the test;
- You can only drink clean, still water;
- do not smoke for 2 hours before the test;
- do not consume spicy, fatty, fried foods and alcohol for 2 days;
- exclude physical and emotional stress 1 day before the analysis;
- do not take the test after radiography, physiotherapeutic procedures and instrumental studies.
Interpretation of analysis results:
The result of laboratory tests is not a sufficient basis for making a diagnosis. Interpretation of the results and diagnosis is carried out only by the attending physician.
Reference values: up to 2.26
Conversion factor : mmol/l x 88.5 = mg/dl
Possible causes of increased TG levels (hypertriglyceridemia)
Primary hyperlipidemias:
- familial hypertriglyceridemia (phenotype IV);
- complex familial hyperlipidemia (phenotype II b;
- simple hypertriglyceridemia (phenotype IV);
- familial dysbetalipoproteinemia (phenotype III);
- chylomicronemia syndrome (phenotype I or V);
- LCAT (lecithin-cholesterol acyltransferase) deficiency;
- Gierke's syndrome.
Secondary hyperlipidemias:
- coronary heart disease, myocardial infarction, atherosclerosis;
- hypertonic disease;
- obesity;
- viral hepatitis and liver cirrhosis (alcoholic, biliary), obstruction of the biliary tract;
- diabetes;
- hypothyroidism;
- nephrotic syndrome;
- acute and chronic pancreatitis;
- taking oral contraceptives, beta blockers, thiazide diuretics;
- pregnancy;
- glycogenosis;
- Thalassemia.
Possible causes of decreased TG levels (hypotriglyceridemia):
- abetalipoproteinemia;
- COPD (chronic obstructive pulmonary disease);
- physical activity (transient decrease);
- malnutrition;
- loss (permanent decrease) of weight;
- hypolipoproteinemia;
- hyperthyroidism;
- hyperparathyroidism;
- malabsorption syndrome;
- intestinal lymphangiectasia.
Substances and drugs that affect the increase in TG levels: beta blockers, catecholamines, corticosteroids, cyclosporine, diazepam, diuretics, estrogens, ethanol, interferon, retinol, miconazole.
Substances and drugs that affect the reduction of TG levels: ascorbic acid, aminosalicylic acid, asparaginase, clofibrate, heparin, fish oil, prazosin.
Where to get tested for triglycerides (TG)
You can take a triglyceride (TG) test at any Synevo point in Minsk, Gomel, Brest, Grodno, Vitebsk, Mogilev, Bobruisk, Baranovichi, Soligorsk, Slutsk, Polotsk, Novopolotsk, Orsha, Zhlobin, Svetlogorsk, Molodechno, Mozyr, Pinsk, Borisov, Rechitsa, Smorgon.
Yulia Mikhailovna Nikitina, cardiologist, functional diagnostics doctor at MEDSI-Premium, talks about what triglycerides are, what they are used for and who is prescribed a test for TG levels in the blood, what to do if their level increases.
Triglycerides (synonyms: blood lipids, neutral fats, TG, TG, Trig, Triglycerides) are one of the main sources of energy in the body. They come with food, are formed in the intestines, liver and adipose tissue, transported in the blood and deposited in adipose tissue. Between meals, they enter the bloodstream and are burned, releasing energy for the body.
Triglycerides are insoluble in water, so they circulate in the blood in the form of macromolecular complexes with proteins called lipoproteins. Most TG in the body is carried by very low-density lipoproteins (VLDL) and chylomicrons.
Blood TG levels fluctuate significantly throughout the day. After a meal, the TG content in the blood serum increases within 15–30 minutes and returns to the initial level only after 9–12 hours, so TG determination is usually recommended to be carried out strictly on an empty stomach, after an overnight period of fasting of at least 12 hours.
However, the transient accumulation of residual lipoproteins rich in TG in the blood during the postprandial period also serves as a significant factor in atherosclerosis. Circulating in the bloodstream, TG can be absorbed by macrophages, which are localized in developing atherosclerotic plaques, which is a key stage in the development of atherosclerosis.
An increase in TG levels is associated with an increase in cardiac risk and indicates the need for a comprehensive analysis of other risk factors.
Also, an increase in their level increases the risk of developing acute pancreatitis - inflammation of the pancreas (a level of >10 mmol/l is considered critical).
What is the research used for?
- Assessing the risk of developing atherosclerosis and cardiovascular diseases
- Monitoring the effectiveness of a diet with a reduced amount of animal fats
- Monitoring blood lipid levels after prescribing medications that lower triglyceride levels
When is the study scheduled?
- Together with a total cholesterol test or as part of a lipid profile. It is recommended that all adults over 20 years old have a lipid profile at least once every 5 years.
- During routine preventive examinations, if a person is prescribed a diet with limited intake of animal fats and/or he is taking medications that reduce triglycerides and cholesterol. In these cases, it is checked whether target lipid levels are achieved and, accordingly, whether the risk of cardiovascular diseases is reduced
- It is especially important to check TG in diabetes and prediabetes, since fluctuations in sugar levels contribute to increased triglyceride levels
- If the patient has one or more risk factors for developing cardiovascular diseases: smoking, age (men over 45 years old, women over 55 years old), high blood pressure (130/80 mm Hg or higher), high cholesterol or cardiovascular diseases in other family members (heart attack or stroke in a close male relative under 55 years of age or a female relative under 65 years of age), coronary heart disease, myocardial infarction or stroke, diabetes mellitus, excess body weight, alcohol abuse, drinking large quantities foods containing animal fats, low physical activity
- If the child is overweight or there have been cases of high cholesterol or heart disease in the family at a young age (it is recommended to take a lipid spectrum test for the first time between the ages of 2 and 10 years)
Causes of increased triglyceride levels (hypertriglyceridemia)
Often, an increase in TG levels is a consequence of diet.
Secondary hypertriglyceridemia can occur with:
- obesity
- alcohol abuse
- type 2 diabetes mellitus and impaired glucose tolerance
- chronic kidney disease, nephrotic syndrome
- liver pathology, cirrhosis
- decreased thyroid function (hypothyroidism)
- pancreatitis
- gout
- smoking
- sedentary lifestyle
- pregnancy
- taking oral contraceptives, estrogens, furosemide, veroshpiron, thiazide diuretics, cordarone, corticosteroids, retinoic acid derivatives, beta-blockers, protease inhibitors, bile acid sequestrants, antipsychotic drugs, cyclosporine and tacrolimus, L-asparaginase, interferon alpha-2b, cyclophosphamide
In rare cases, an increase in TG levels may be a consequence of hereditary disorders of lipid metabolism (in such situations, the indicators significantly exceed the upper limit of reference values): familial combined hyperlipidemia, familial dysbetalipoproteinemia, familial hypertriglyceridemia, familial lipoprotein lipase deficiency.
Reduced triglyceride levels are not significant in diagnosis. It is most often found in intestinal pathologies associated with malabsorption of nutrients, during a period of strict diet, fasting, hyperthyroidism, in patients suffering from chronic obstructive pulmonary disease, with cerebral infarction, hereditary hypolipoproteinemia, and intense physical activity. Taking a number of medications can reduce TG levels: statins, cholestyramine, clofibrate, colestipol, fenofibrate, fish oil, gemfibrozil, nicotinic acid.
How to properly prepare for research?
- Do not eat for 12 hours before the test
- Avoid physical and emotional stress and do not smoke 30 minutes before the test
- Avoid drinking alcohol 24 hours before the test
If the level of blood triglycerides increases and after assessing the cardiovascular risk, the attending physician will definitely recommend non-drug treatment methods and lifestyle modifications:
- reduce the number of calories in the diet, lose weight (losing weight by 5-10 percent helps reduce triglyceride levels by 20%)
- choose the “right” fats (unsaturated fats, especially polyunsaturated fats, lean meats, poultry, low-fat dairy products and some seafood), avoid trans fats and saturated fats
- limit the amount of carbohydrates and give preference to fresh vegetables, berries, whole grains
- reduce your intake of sugar and sweetened drinks
- reduce alcohol consumption
- Walk for 30 minutes every day (at a minimum), and ideally recommend 150 minutes of moderate aerobic activity, 75 minutes of vigorous aerobic activity, or a combination of both each week
If these measures are insufficiently effective, the attending physician will select a drug that normalizes triglyceride metabolism.