How to do an ECG correctly, classification of various techniques, diagnostic stages
An ECG procedure is prescribed by a cardiologist if heart and vascular diseases are suspected.
Some categories of citizens regularly undergo this examination due to chronic diseases or due to the nature of their professional activities. Patients who were first prescribed this diagnostic method are wondering why they need to do an ECG? The heartbeat is accompanied by electrical impulses, which are recorded by a special device - a cardiograph. The device has several sensors that collect information from various points of the human body, which are located in the chest area, on the upper and lower extremities. A cardiogram represents waves on a graph corresponding to each phase of the heart rhythm.
How is an ECG done? The procedure for patients of different ages is carried out according to the same scheme. The purpose of the manipulation is to record the contractions and relaxations of the heart muscle. The diagnostic procedure is carried out in stages: first, sensors are fixed on the human body, and then electrodes transmit information about the work of the heart to the device.
The cardiograph produces a schedule according to which the specialist determines whether the patient has a particular pathology and draws up a suitable treatment regimen. The procedure is carried out quickly and has no absolute contraindications.
Using an ECG, cardiovascular diseases such as heart defects, myocardial infarction, inflammatory diseases, etc. are diagnosed. Not only the correct conduct of an ECG is important, but also preparation for it and a competent interpretation of the result. Only these measures taken together will make it possible to promptly identify and eliminate dangerous pathologies of the circulatory system.
How many times a year can the examination be done? An ECG is recommended to be performed once a year for persons over 40 years of age and patients with heart problems. How often a patient needs to be examined is determined by the doctor depending on his state of health.
Pressure 220 (200) per 100 (110,120,130): what to do, causes and consequences
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
High blood pressure may indicate hypertension and other ailments. A decrease in pressure can only occur after the cause of the condition has been eliminated; for this you should seek medical help.
High blood pressure is the most commonly reported cardiovascular disease. Pressure is the force with which blood pushes against the walls of the arteries as it moves through the body. Blood can fill the arteries only to a certain extent.
High blood pressure from 180/90 mmHg. Art. and more can lead to serious diseases, for example, which are dangerous to the full health and life of a person. Hypertension is also a leading cause of heart attacks.
How to take measurements
A person’s blood pressure consists of two indicators. The first, higher one, shows systolic pressure - the pressure inside the arteries when the heart fills them with blood. The second number expresses diastolic pressure, that is, the pressure inside the arteries when the heart breathes between beats.
Normally, blood pressure gradually increases from 90/60 mmHg. Art. at birth and up to 120/80 in a healthy adult. If a person jogs or drinks alcohol, the blood pressure will rise noticeably, but this is not a cause for concern.
A person’s blood pressure rises and falls under the influence of emotional state and physical activity. For one person, a reading of 130/90 mmHg is considered normal, while another person feels unsatisfactory in such cases.
If you have persistently high blood pressure, you should visit your doctor. With this pathology, the heart works at its limit. In addition to blood vessels, deformations occur:
- brain,
- eye,
- kidney
If the pressure is 140/90 mmHg. Art. and higher with measurements of more than two, then we can talk about hypertension. When the pressure is 200/120 or higher, urgent medical attention is needed. If you have diabetes and high blood pressure, treatment should begin at 130/80 mmHg. Art.
Scientists include people whose blood pressure is more than 120/80 mmHg. Art, in a category that has a chance of developing hypertension. This condition is called prehypertension. Prehypertension increases the likelihood of system and organ defects, so it is important to begin timely treatment.
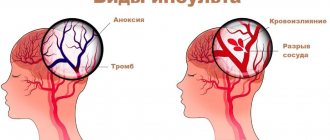
Because hypertension often has no symptoms, it is called the “silent killer.” It is typical that symptoms may not appear even with serious complications. The disease is severe when the pressure is 220/110 mmHg. Art and above provokes:
- vision problems,
- heart attack,
- stroke,
- kidney failure.
Hypertension leads to heart failure, a common but very dangerous disease that causes breathing problems. It is generally accepted that people with high blood pressure have malignant hypertension with a diastolic pressure of more than 130 and a systolic pressure of more than 200 mmHg. Art. This type of hypertension is a very serious disorder, since various organ damage occurs very quickly.
High blood pressure can be controlled and corrected. To do this, you must first of all systematically measure your blood pressure.
Risk group
on
There are several categories of people who are most likely to develop hypertension. People most often affected by high blood pressure are:
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
- with a genetic predisposition,
- African Americans,
- aged over 55 years,
- overweight
- leading a passive lifestyle,
- smokers and alcohol abusers,
- consuming unhealthy and highly salty foods.
Hypertension may also affect patients who use certain medications, such as nonsteroidal anti-inflammatory drugs, decongestants, and drugs such as cocaine.
Norms and classifications of arterial hypertension
There are three degrees of the disease.
- With stage 1 hypertension, the pressure is from 140/90 to 160/99 mmHg. Art. The pressure rises and falls abruptly. If hypertension at this stage is not treated, it transforms into more serious stages,
- Stage 2 hypertension is called moderate. Here the pressure changes to 179/109 mmHg. Art. In this case, a protracted increase in pressure is observed. The indicator rarely drops to normal,
- Stage 3 hypertension is the most severe. Pressure starts from 180/110 mm Hg. and stays stable.
Normal blood pressure varies from person to person. Medicine suggests taking 120/80 mmHg as a normal indicator. These indicators are observed in people aged 20 to 40 years.
Normal blood pressure for ages 16 to 20 is usually slightly low. This applies to both systolic and diastolic pressure. The physiological norm is blood pressure at rest at 100/70 mm Hg.
In general, blood pressure is considered normal in the range of 90 - 139/61 - 89 mm Hg. Doctors consider 120/80 mmHg to be the absolute norm. Slightly elevated blood pressure – 130/85 mmHg, elevated normal blood pressure – 139/89 mmHg. An increase in the indicator to an increase of 140/90 mmHg and above indicates an existing pathology.
Over time, irreversible processes begin in the human body, causing an increase in blood pressure throughout life. Over the years, any person's blood pressure increases.
There are blood pressure standards based on a person’s age and gender.
- At 20 years old, blood pressure in men is 123/76, in women 116/72 mm Hg,
- At 30 years old, men have 126/79, women 120/75 mmHg. st,
- At 30–40 years old, men have 129/81, women 127/80 mm. rt. st,
- At 40–50 years old, men have 135/83, women 137/84 mmHg. st,
- At 50–60 years old, men have 142/85, women 144/85 mmHg. st,
- After 70 years, men have 142/80, women 159/85 mm Hg. Art.
As the data shows, changes due to age affect both the upper and lower blood pressure levels. It is important to remember that these are averages and do not reflect individual patterns.
Not only high blood pressure, but also a decrease in its indicators is a characteristic sign of deterioration in the functioning of body systems. Therefore, the ability to take measurements with a tonometer can be attributed to the prevention of almost all ailments.
To identify the dynamics of changes in blood pressure, you should keep a diary.
Constantly high blood pressure
The third stage of hypertension is the most severe. In this case, the constant pressure exceeds 180/100 mmHg. Art. Gradually a person gets used to this condition, but the heart works under high load and wears out a lot. Patients often experience:
- cardiac ischemia,
- heart rhythm disturbance,
- angina pectoris
- the formation of heart failure.
Thus, at any age of a person, a blood pressure of 120/80 mm Hg is considered normal. Art. with slight deviations in both directions. If blood pressure systematically increases to 160/100 mm Hg. Art. or remains at this level for a long time - this indicates the initial stage of hypertension.
Regardless of what age a person is, he should immediately consult a doctor for a thorough examination. The doctor sets the task of clarifying the diagnosis by conducting diagnostics. After identifying concomitant diseases, specific treatment is prescribed.
The examination includes:
- examination by a therapist,
- study of medical history (heredity, work, bad habits, general lifestyle),
- general clinical analysis of urine and blood,
- blood for cholesterol and sugar levels, ECG,
- consultation with an ophthalmologist, fundus examination,
- examination by a neurologist.
If the need arises, an endocrinologist or cardiologist should be involved in the diagnosis. The following may also be prescribed:
- Ultrasound of the heart,
- MRI,
- 24-hour blood pressure monitoring.
After the examination and study of the medical history, the doctor reviews the results and forms a treatment plan. In severe stages of hypertension, the person should be hospitalized for more intensive treatment.
It is important to visit a doctor in any case, at least to find out what exactly to do if your blood pressure increases.
The doctor should measure the patient's blood pressure and consider lifestyle changes. In particular you need:
- weight loss,
- proper diet with a reduction in fat and salt,
- moderate physical activity,
- giving up alcohol, smoking and coffee,
- walks in the air.
It is necessary to consume vegetables and fruits rich in potassium and magnesium in your diet, including:
- greenery,
- carrot,
- legumes,
- sea kale.
You should buy a tonometer and take measurements twice daily - in the morning after getting up and in the evening before going to bed.
It is necessary to take medications only as prescribed by your doctor. All medications for high blood pressure are prescribed for a certain time to achieve a lasting result.
Diuretics are used, for example:
- Furosemide,
- Indapamide,
- Arifon,
- Indap.
These products reduce swelling by removing excess fluid. Therapy begins with diuretics, if there are no such diseases:
- diabetes,
- renal failure,
- lactation and pregnancy,
- gout,
- allergy.
Beta blockers are also used:
- bisoprolol,
- metoprolol,
- Celiprolol.
These drugs reduce blood pressure by dilating blood vessels and reducing the load on the heart muscle. The medicines should not be taken if you have allergies, bradycardia or pregnancy.
ACE inhibitors:
- Enalapril,
- Perindopril,
- Ramipril.
These drugs dilate blood vessels and are contraindicated in cases of renal impairment and pregnancy.
Calcium antagonists include:
- Verapamil,
- Amlodipine,
- Diltiazem.
These drugs show effectiveness in hypertension, accompanied by increased heart rate and heart rhythm disturbances. The drugs should not be used during pregnancy or bradycardia.
Quite often, combinations of funds from different groups are used. May be assigned:
- sedatives,
- phytotherapy,
- medicines to strengthen the heart muscle,
- statins and other drugs.
During pregnancy, high blood pressure is common, especially after the 20th week. There is a physiological reason for this - the volume of circulating blood increases due to the fetus, so the heart works harder, the pulse quickens and blood pressure rises. As a rule, the figure does not exceed 140/90 mmHg.
If a woman complains of unsatisfactory health in the first half of pregnancy due to high blood pressure, most often this indicates the appearance of hypertension.
Increase in pressure to 160/100 mmHg. Art. and more at any stage is a reason for hospitalization, since the fetus suffers with this pressure. If you have high blood pressure in the second half of pregnancy with a pathological urine test, you should consult a doctor, since there is a high risk of eclampsia, a serious complication.
Every morning a person with hypertension should begin with measuring their blood pressure. Treatment should only be carried out under the supervision of a physician. The video in this article will help you figure out what to do with high blood pressure and what to do.
on
Standard research design
The doctor does an ECG as follows:
- Before installing the sensors, make sure that there are no metal jewelry on the patient’s body. The patient's body is freed from excess clothing, the upper torso, wrists and shins are exposed.
- The electrode attachment points are treated with special compounds to better attach the sensors to the skin surface.
- The person takes a horizontal position, lying on his back. Before doing an ECG, the doctor writes down all the information about the patient.
- The sensors are fixed on the body using special clamps. The devices are placed in the lower part of the forearms, the outer and inner areas of the legs.
- The chest leads are attached to the skin of the chest in 6 zones using adhesive tape.
- The sensors are connected to the device according to a certain scheme: the red wire is attached to the right hand; yellow – to the left upper limb; green - to the lower left, white - to the chest.
- Leads are registered. According to the standard scheme, sensors are registered through alternate connections: 1 lead - the sensor from the left upper limb is connected to the electrode of the right hand; Lead 2 – the sensor from the right upper limb is combined with the electrode of the left leg; Lead 3 – combines the sensors of the limbs located on the left side.
Standard ECG scheme
Important! During the procedure, the person must not move and remain in a calm psycho-emotional state.
To register an electrocardiogram, the patient is recommended to follow some rules:
- during the diagnostic procedure, breathe evenly and avoid emotional overload;
- do not eat 2-3 hours before the procedure;
- patients with severe shortness of breath are recommended to perform the procedure in a sitting position;
- Women should remove their bra.
Patients who have never had an ECG often ask: how long does the study take? Answer: about 3-5 minutes. Another question that interests women is whether it is necessary to take off their bra before an ECG? Answer: when recording an ECG, suction cups are placed on the surface of the skin of the chest, and any materials, including a bra, create interference.
To examine heart rhythms that occur only during physical activity, non-standard ECG schemes are used, for example, a stress test. Heart rate measurements are taken after exercise on a treadmill or bicycle. If the patient has contraindications to physical activity, then to conduct a stress test, he is injected intramuscularly with drugs that stimulate the heart.
Stress tests are prescribed to diagnose a patient with coronary heart disease in the early stages of development, which does not manifest itself with characteristic symptoms.
Several hours before the procedure, alcoholic and caffeine-containing drinks are excluded from the diet.
Performing a stress test
You should know! An ECG of the heart according to the standard scheme is performed in a supine position. But if it is necessary to confirm disturbances in heart rhythm or conduction of the cardiac arteries, the procedure is performed in a standing position. Before the ECG, women will only need to remove their bra, and men should preferably shave their chest hair so that the ECG recording goes as smoothly as possible.
If stress tests record abnormal values, then the diagnosis is carried out with hyperventilation. What is this technique used for? Nonspecific changes in the cardiogram can appear for two reasons - due to increased physical activity or as a result of diseases of the cardiovascular system.
To understand the cause of the anomaly, the doctor asks the patient to breathe evenly and deeply. During this time, adaptive changes occur in the body, and the line on the ECG takes on a normal physiological appearance. If after hyperventilation the heart rate increases two or more times relative to the control result, then the test is considered positive. This indicates that the patient has neurocircular dystonia.
A stress test with hyperventilation is not performed on children and patients suffering from problems with cerebral circulation, since the test may provoke vasospasm.
If the patient has a predisposition to an irregular rhythm, then he is prescribed Holter monitoring. In this case, using a standard scheme it will not be possible to detect the deviation in a few minutes. The device for Holter monitoring has 2, 3 or 12 valves. It is worn for 24-48 hours.
Is it possible to do a CT scan on your own initiative without a doctor’s referral?
Children will not be given a CT scan without a doctor's order. There are no rules for adults that would prohibit them from signing up for examinations and taking tests on their own. However, there is a risk of examining the wrong thing or not. For example, a woman, unknowingly, can undergo a pelvic ultrasound herself on any day and only then go to the gynecologist. The doctor may be alarmed by some points in the ultrasound results, and he will ask you to repeat the examination during the 5-10th day of the cycle, when, according to the standards, this diagnosis is carried out. As a result, the patient will simply pay for the same procedure twice, but without harm to health.
With a self-ordered CT scan, the risk isn't just double payment. As we wrote earlier, due to X-ray radiation, this examination must be done correctly the first time and with good equipment. Only an experienced doctor will determine which organ needs to be examined and to what extent. Plus, like any medical procedure, there are contraindications that the patient may not be aware of, even if he has read several articles on the Internet. Therefore, in this case, self-medication is doubly dangerous.
Functional diagnostics doctor Inna Petrovna Aleshova:
We invite you to the Filatov Clinic to undergo a safe examination using our new SOMATOM go.Up computed tomograph.
The device is an advanced model with low radiation exposure. IVR technology allows you to obtain 64 high-quality image slices per revolution of the ring, which guarantees more accurate diagnosis of the lungs and other organs. You can sign up for the study by phone. or online registration.
Operating principle of an electrocardiograph
The main components of any cardiograph are a galvanometer, a lead switch, an amplification system and a recording device. Weak electrical impulses arising in the heart of the subject are perceived by electrodes, amplified and then detected by a galvanometer. Data on changes in the electromagnetic field enters the recording device, and the recorders leave graphs of the work of various parts of the heart on a uniformly moving paper tape. There are teeth of different sizes, depending on the strength of the signals this department sends.
But it is important not only how an ECG is done, but also the correct interpretation of the recordings. The norms for the duration and height of each tooth were established experimentally, and any deviation from these norms indicates a certain problem. Knowing how an ECG of the heart is done, being able to decipher it, as well as the ECG norm in adults, a specialist is able to make an accurate diagnosis.
To the question of what to do before an ECG, the answer is quite simple: you don’t need to do anything special. You just need to calm down before recording it, especially since this is a non-invasive method. Before doing an ECG of the heart, no punctures are needed.
During the examination, the patient experiences absolutely no discomfort from the procedure itself.
True, while women are undergoing ECG, they are not recommended to use greasy creams on their chests, since they reduce skin conductivity and distort the measurement results. Since all electrodes should be attached only to the naked body, when going for this procedure, it is better to wear the most easily removable clothing. For example, a woman who is doing an ECG will still have to take off her tights, since electrodes are also attached to her ankles.
Any doctor can give a referral for this procedure, however, most often this is the domain of cardiologists. But when you are referred for an ECG, which doctor performs this procedure, each hospital may answer you differently. This is mainly done by functional diagnostic doctors, but often this procedure is also performed by nurses.
So, the sequence of actions when performing an electrocardiogram:
1. The subject lies down on the couch. 2. The electrode attachment points are degreased with ethanol. 3. Then a conductive gel is applied to them (it is sometimes replaced with wet gauze wipes). 4. Electrodes are attached to his chest, hands and ankles, fixed with a suction cup. 5. Wires from the electrodes extend to the device itself, which receives and processes cardiac impulses. 6. Afterwards, the doctor turns on the device, which begins to record an ECG graph. 7. The output is a tape with graphs, after decoding which the specialist can prescribe and adjust further treatment.
If there are serious deviations in the diagram, the attending cardiologist should immediately get involved in assessing the results.
In order for the ECG procedure to be successful, it is important to follow some rules:
- During the procedure, the patient should breathe evenly and not worry. For this purpose, it is desirable that the subject lie on the couch for at least five minutes.
- The last meal before the procedure should be no later than two hours.
- The room where the electrocardiographic examination is performed must be sufficiently warm. Otherwise, physiological tremors caused by cold can distort the pattern of cardiac activity, which will be reflected in incorrect cardiogram data.
- Patients with severe shortness of breath during an ECG are recommended not to lie down, as usual, but to sit, since it is in this position that all cardiac arrhythmias are most clearly recorded.
In addition to how this procedure is done, many people have a question: how long does an ECG take? Let's answer: no more than a couple of minutes.
Despite the fact that this procedure does not bring any discomfort, it is still worth knowing one more thing about the ECG: how often can this examination be done?
People over 40 years old are recommended to have an ECG once a year.
How often to do an ECG for older people is decided by their attending physician, but it is recommended once a quarter.
When should a CT scan be done instead of an X-ray?
X-ray is a well-known and more affordable diagnostic procedure. The price of CT scans is usually higher. A logical question arises: why pay more if you can get an x-ray?
A regular X-ray produces a two-dimensional picture, so images of organs overlap each other, which reduces the accuracy of diagnosis. The result will depend on the doctor's experience and ability to read radiographs. X-ray is more suitable for primary diagnosis, since it does not allow a full assessment of the situation, the condition of tissues, inflammation, formations, etc. Therefore, often with “suspicious” results and other related indications, the doctor refers the patient to the most accurate and unambiguous diagnosis - computed tomography.
The CT machine provides a three-dimensional volumetric image of the examined organ. It can be studied in small details from different angles. A computed tomogram clearly shows the consequences of injuries, benign and malignant neoplasms, stones, cysts, developmental defects, etc. A high-quality three-dimensional image helps to identify pathologies even at the earliest stages of development.
What is safer - a CT scan of the lungs or an X-ray?
During a routine X-ray of the lungs, a person receives a radiation dose of 1.2 mSv. While a modern computed tomograph allows you to do a low-dose CT scan of the lungs, in which the radiation dose will be from 0.3 to 0.7 mSv, depending on the patient’s build. Plus, the radiologist will be able to evaluate the lung tissue in 3 projections at once, which is impossible with X-rays. Therefore, examining the lungs with a modern tomograph is several times safer and more informative than taking an X-ray.
What does electrocardiography show?
Not only patients with complaints, but also healthy people are prescribed an ECG. Why is this procedure done and what can it show? Using this research method you can determine:
- Regularity and heart rate.
- Chronic and acute myocardial damage.
- Disturbances in the metabolism of potassium, magnesium and calcium.
- The cause of pain in the heart area is whether it is caused by the work of the heart or, for example, by a pinched nerve.
- General condition and thickness of the myocardial walls (which may be normal or increased).
- The condition of an electrical pacemaker implanted in the heart.
How to make an ECG: the process of performing a cardiogram
The principle of performing an ECG is based on the ability of the device to capture electrical impulses arising in the heart and, after processing, record them in the form of a graph. Next, the results obtained are interpreted by a specialist in functional diagnostics, and the attending physician can use the data to make a diagnosis.
An electrocardiogram is performed using a special device - an electrocardiograph. Its main components are:
- galvanometer;
- lead switch;
- system for amplification of captured signals;
- recording device.
During the procedure for taking an ECG, electrodes installed at certain points capture electrical impulses arising in the heart and transmit them through a galvanometer to a recording device. Next, the recorders display the received information on paper moving at a certain speed in the form of graphs showing the functioning of different parts of the heart. ECG graphs are recorded on graph paper in the form of lines of teeth of different sizes. These sizes depend on the strength of the signal sent by one or another part of the heart. Video: Recording an electrocardiogram
The results of the study are described by a specialist who compares these standards with the results obtained. In the interpretation, the doctor of functional diagnostics indicates the identified deviations, according to which the patient’s attending physician makes a diagnosis.
How is a CT scan done?
“Is it scary to climb inside the apparatus, what if I have claustrophobia?” There is a stereotype that you will be “stuffed into a narrow pipe, where it will be scary and dark.” This is wrong. During the procedure, the patient lies down on a special table that fits into a portal - inside a large ring. It doesn't look like a pipe, but rather like a donut. The portals of modern tomographs have a wide open area to provide greater physical and psychological comfort. You are not lying in a closed space - not the whole body is inside the ring, but only the part being examined. At this moment, medical workers are monitoring the process from the next room and communicating with you through a speakerphone.
The computed tomography procedure on previous generations of computed tomographs lasts 5-40 minutes, depending on the area being examined. With a new generation of tomographs, such as the SOMATOM go.Up from Siemens, a CT scan of, for example, the sinuses is scanned in just 10 seconds. The only unpleasant thing can be the need to lie still all this time, and during a CT scan of the lungs, also at the doctor’s command, to hold your breath. Therefore, for people with increased excitability or claustrophobia, the doctor may prescribe a sedative before the examination. The time it takes to prepare results with transcripts depends on the density of the examination schedule, but not more than a few hours.
When is electrocardiography necessary?
Indications for prescribing an electrocardiogram are the following patient complaints or symptoms:
- dyspnea;
- discomfort and pain in the chest area;
- frequent stress;
- tachycardia or bradycardia;
- signs of arrhythmias;
- overweight;
- suspicions of hypertension and other manifestations of cardiovascular diseases;
- preparation for surgery or certain types of diagnostic tests.
For preventive purposes, an ECG should be performed on all persons over 40 years of age once a year. At a more mature age, the study should be performed once a quarter. For people suffering from pathologies of the heart and blood vessels, an electrocardiogram is performed as often as necessary, that is, within the time frame determined for them by the doctor, guided by data on the existing disease.
How is a cardiogram read and what does an ECG determine?
The ECG conclusion is made by a functional diagnostics doctor and a cardiologist. The description of the study includes several stages:
- assessment of the patient’s age and gender – the interpretation of the results according to age norms depends on these data;
- determination of the amplitude, duration of waves and intervals of the cardiogram - analysis of the P wave and the duration of the P - Q interval, ventricular QRS complex, ST segment, T wave, Q - T interval;
- rhythm characteristics - with arrhythmias, an abnormal rhythm is detected, an increase in the heart rate of more than 100 beats per minute, a violation of the conduction of an electrical impulse through the conduction system, or a non-sinus rhythm;
- the presence of focal changes in the heart muscle - when identifying zones of myocardial infarction, the localization of the focus of necrosis and its prevalence is determined;
- manifestations of hypertrophy of certain parts of the heart - an increase in the size of the heart muscle is manifested on the ECG by increased electrical activity of the enlarged chamber, ischemic or dystrophic processes in the myocardium, or slow propagation of the electrical impulse in the wall of the hypertrophied cardiac chamber.
In addition to the changes in the heart described above, an electrocardiogram can help evaluate the position of the organ, signs of myocarditis, pericarditis, the condition of the implanted pacemaker, disturbances in electrolyte metabolism and other abnormalities. After analyzing all the data obtained, a conclusion is formed. If possible, the ECG performed is compared with previously recorded cardiogram graphs, that is, the results are monitored over time. Normal ECG readings are:
- the rhythm is correct and regular, with a source in the sinus node;
- heart rate - determined by measuring the distance between adjacent R waves (R - R interval), the indicator is estimated depending on age (for adults and healthy people under 50 years old - 60 - 90 beats per minute);
- electrical axis of the heart – normally the alpha angle is 40 – 70 °.
Video: ECG norm. All intervals and waves: p, QRS, T, PR, ST
Measuring blood pressure - step-by-step technique
We present to your attention a step-by-step technique for measuring blood pressure at home. You will see that measuring your blood pressure at home with a tonometer is easy and convenient. You don’t need to go to the doctor every time for this. We recommend that everyone have a modern electronic blood pressure monitor at home. This device is not too expensive at the pharmacy, and can bring you great benefits - protect you from heart attack, stroke and other complications of hypertension. Useful article “Which tonometer to buy for home” - an independent review of home tonometers, objective information, no advertising.
Don't panic and don't grab the pills if your blood pressure is high according to the first measurement. Repeat the procedure at least twice more. On our website you will learn how to cure hypertension on your own, as well as what medications your doctor can prescribe. Good news: we will teach you for free how to maintain normal blood pressure without “chemical” pills, “starvation” diets and grueling exercise.
Remember that blood pressure is above 180/120 mmHg. requires immediate medical attention.
If the patient complains of frequent dizziness, then it is necessary to separately measure blood pressure in a standing position. If in this case the systolic pressure decreases by 20 mmHg. Art. or more, and diastolic - by 10 mm Hg. Art. or more than in a sitting position, a diagnosis of orthostatic hypotension is established - a disorder of the autonomic nervous system, characterized by a sharp decrease in blood pressure when the body position changes (from sitting or horizontal to vertical).
- The best way to recover from hypertension (quickly, easily, healthy, without “chemical” drugs and dietary supplements)
- Hypertension is a popular way to cure it at stages 1 and 2
- Causes of hypertension and how to eliminate them. Tests for hypertension
- Effective treatment of hypertension without drugs
- Cardiac ischemia
- Myocardial infarction
- Heart failure
- Diabetes
Which tonometer is better to use?
To measure blood pressure at home, we recommend using a semi-automatic blood pressure monitor with an upper arm cuff. This is the best option in terms of price and quality. You can buy a semi-automatic blood pressure monitor at the pharmacy - accurate and durable - for no more than $60. For such modest money you will get a modern device from Switzerland, the USA, Germany or Japan.
Automatic blood pressure monitors are less accurate. We believe that when measuring pressure, pumping air with a bulb is not such a big deal, and there is no point in overpaying for a fully automatic tonometer. Wrist or finger blood pressure monitors are not accurate enough. Their use is not recommended. Especially those on the finger.
Before purchasing, make sure the blood pressure cuff fits you. As a rule, medium-sized cuffs are suitable for most people, and blood pressure monitors come with them. Please do not use older blood pressure monitors where you need to listen to heart sounds with a stethoscope.
Step-by-step technique for measuring blood pressure
We further assume that you are using a semi-automatic electronic blood pressure monitor and do not need to listen to heart sounds with a stethoscope. Read the article “How to Prepare for Blood Pressure Measurement.” It is important to properly attach the blood pressure monitor cuff to your shoulder. It should be 2-3 cm above the elbow joint, and in height - at the same level as the heart. This is clearly shown in the picture.
- Wrap the cuff around your arm and secure it in position with Velcro.
- Hold the tonometer's bulb-shaped pump in your hand.
- By squeezing and unclenching the bulbar pump, inflate the air in the cuff until the tonometer shows a pressure of approximately 40 mmHg. Art. higher than what you expect.
- Begin deflating the cuff. To obtain reliable results, measuring blood pressure should be done slowly, at a speed of about 2 mmHg. Art. per second. The pressure in the cuff will decrease and blood flow through the artery will resume.
- Write down the resulting systolic and, through a fraction, diastolic pressure, without relying on memory.
- Take not one, but several blood pressure measurements at once. Because the results of the first measurement are often very overestimated. Measure 3-8 times in a row on the same hand, with an interval of several minutes. Until the results begin to more or less coincide, with a minimal difference. Before each new measurement, bend and straighten your arm to restore blood circulation. Calculate the average value of “similar” results and consider it reliable. Do not take into account measurement results that deviate greatly from all others.
- Record the measurement result in your diary. Please also indicate the date and time (morning, afternoon or evening). Also mark the hand on which the measurement was taken (right or left).
Why is it necessary to measure blood pressure several times in a row and average the result?
In most cases, the results of the first blood pressure measurement are overestimated. Because due to the squeezing of the arm by the tonometer cuff, the tone of the blood vessels greatly increases. This is an automatic, involuntary reaction of the body that needs to be taken into account and adapted to. If an experienced doctor measures your blood pressure, he will not be satisfied with one measurement, but will take it 2-3 times.
We recommend that you measure your blood pressure with a semi-automatic tonometer on one arm at least 3 times in a row. If the results of the second and third measurements are repeated, with a slight difference, then this is the patient’s real blood pressure value. If there is no coincidence, then do 4-8 “approaches” until you see stable repeatability. After this, calculate the average, write it down in your diary and analyze it.
Let's illustrate this technique for measuring blood pressure with specific examples.
Patient #1
| 1 | 154/94 |
| 2 | 137/84 |
| 3 | 136/86 |
In this case, blood pressure is the average of measurements Nos. 2 and 3.
Patient #2
| 1 | 156/96 |
| 2 | 138/89 |
| 3 | 134/82 |
| 4 | 132/78 |
| 5 | 129/78 |
In the second case, you can use the arithmetic average of measurements Nos. 3, 4 and 5 (it turns out 132/79) or only measurements Nos. 4 and 5 (it turns out 131/78). If we had limited ourselves to just one measurement, both patients would have been left upset and overtreated.
Analyzing the results
Now is the time to analyze the results of the blood pressure measurement you just took. Notes will help you with this:
- Blood pressure measurement: interpretation of results;
- Stages of hypertension
If your blood pressure is high, repeat the measurement after 60 seconds on the same arm, and then after another minute on the other arm. If the pressure on one arm is higher than on the other, future measurements should be taken on that arm. The diagnosis of hypertension can be made only if measurements for several days in a row show that the patient has consistently high blood pressure.
Many people worry that their blood pressure monitor is not accurate. In fact, the main problem is errors in the process of measuring blood pressure, not the quality of the devices. Watch the video “Is your tonometer lying?”, prepared by famous specialist Elena Malysheva. It does not discuss the comparative characteristics of different tonometers, but the technique of measuring blood pressure. It clearly shows the mistakes people make most often and how much these mistakes inflate results.
A single measurement is not enough to prescribe medications for hypertension to a patient. If you suspect that you have hypertension, do not make hasty conclusions. First, measure your blood pressure for a week. Do this every day at the same time, preferably in the afternoon or evening. Of course, all this is provided that you are feeling normal. If anything worries you, consult a doctor as soon as possible.
Benefits of home blood pressure monitoring
Doctors should more actively encourage their patients to measure their blood pressure at home. Because patients who use home blood pressure monitors receive significant benefits:
- The measurement results are more reliable because there is no white coat effect.
- When the patient clearly sees the results of treatment on the tonometer (blood pressure decreases), he willingly continues to take medications and follow the recommendations for a healthy lifestyle.
- It is easier for the patient to assess whether a particular medicine is suitable for him or not. However, remember that you need to give each medicine a minimum of 3 weeks before deciding whether it works well for you.
- How to avoid mistakes when measuring blood pressure
- Isolated systolic hypertension - important for elderly patients over 60 years of age
- Hypertension in pregnant women
Features of undergoing cardiography for children
ECG can be prescribed to children of any age. When assessing the results, the doctor must be guided by age characteristics and, if necessary, supplement the study with other techniques (for example, Echo-CG, cardiac CT, etc.). ECG in children has its own specific feature in each age period, since the heart is influenced by many factors depending on age and growth: changes in the number of heart contractions, the influence of the autonomic and endocrine systems, the anatomical position of the heart in the chest, changes in the speed of propagation of impulses and etc. The following clinical cases may be the reason for prescribing an ECG for a child:
- heart murmurs;
- heart rhythm disturbances;
- the presence of even slight shortness of breath;
- pathologies of other organs;
- a history of severe infectious diseases;
- identification of relatives with severe heart pathologies in the patient’s medical history;
- the need for surgical treatment;
- preventive examination during sports activities.
Features of taking an ECG by women during pregnancy
Carrying out an ECG is an absolutely safe procedure and is not dangerous for pregnant women. That is why women should not refuse to perform such a study, which allows timely identification of various abnormalities in the functioning of the heart, which experiences increased stress during gestation. During pregnancy, the ECG procedure is prescribed 2 times; in addition, an electrocardiogram is performed not only on the woman, but also on the fetus - this study is called CTG (cardiotocography). When interpreting the results, the doctor must take into account the features that occur in a woman’s body during pregnancy (especially in its later stages) and that affect the nature of the cardiogram graph:
- displacement of the electrical axis to the left;
- increase in the number of heart contractions;
- negative T wave in the third and fourth leads;
- shortened PR interval;
- pathological wave in Q in the third lead and aVF (right arm lead).