Heart formation
So, a new life was born. Whether you wanted it or not, whether the fruit of your love is desired or not - it doesn’t matter anymore. The egg formed in the ovary passed through the tubes, settled in the uterine mucosa, received and merged with the sperm. This is already a fertilized egg that will grow and eventually become your child.
This life, while still only one cell, carries all the information contained in your genes, i.e. the smallest protein molecules, and in your partner's genes. We will return to this later. But now, the cells have merged, and in the first two weeks after conception, the processes of formation of cellular systems begin, which will then turn into tissues and organs.
As the amazing poet Dmitry Kedrin once wrote:
“There is still no trace of nausea or spots. And your belt is just as narrow, just look in the mirror. But you, by elusive, secret feminine signs, frightenedly guessed what was inside you ... "
At first, new life has the shape of a disk. Sometimes such a small protein disc can be seen in the yolk of a broken chicken egg. It is called an embryo and in the first days it is just a collection of wise cells that know exactly what they need to do. With each subsequent hour there are more and more cells. They connect and fold into certain shapes, first forming two tubes, then merging into one. This tube folds and descends from the primary disk to form a loop called the “primary cardiac loop.” The loop quickly lengthens, significantly outstripping the growth and increase in the number of cells surrounding it, and lies to the right, in the form of such a ring as the ring of a mooring rope, which is thrown onto the bollard when mooring a boat or vessel. This loop normally lies only on the right, otherwise the future heart will lie not on the left, but on the right of the sternum. And on the 22nd day after conception, the first contraction occurs in the thickened lower part of the loop. The heart began to beat. You can try to remember what happened to the future mother then. What condition was she in? What was happening to her? And, if you, like the vast majority of married and non-family couples, did not pay attention to this, I can guarantee that you will not remember. You will say: “So what?” - and you will be right. As a rule, nothing. But still, think about it. The first days may not solve anything. But the next ones will decide a lot.
The cardiovascular system of the fetus is formed first of all its systems, because the fetus needs its own blood circulation for the full development of its other organs. The development and formation of the cardiovascular system begins in the third week and mainly ends by the eighth week of the embryo’s life, i.e. occurs within five weeks.
We will briefly describe these stages, but now let’s ask ourselves the question: “What is 4–5 weeks of pregnancy today?” The woman is not yet sure whether she is pregnant, especially if she is not looking forward to this event too much. She does not change her lifestyle, habits, sometimes harmful ones. She can work in hard and hazardous work or do hard physical work at home. She can carry a viral infection in the form of influenza on her feet. Usually a couple doesn’t think yet, tries not to think about the future, but it – this future – not only lives, but also beats, contracts, grows. But wait to punish yourself - there may be other reasons. More about them later. In the meantime, let us remember: today in the world they believe that a child’s life begins not from the moment of his birth, but from the moment of conception.
So, on the 22nd day, the future heart begins to pulsate, and on the 26th day, independent blood circulation begins in the body of the fetus, whose length is 3 millimeters. Thus, by the end of the fourth week the fetus has a contracting heart and circulation. So far it is one stream, one curved tube, in the bend of which lies the “motor” - the heart. But every minute processes take place in it that lead to final formation. It is very important to understand that these processes flow simultaneously in three-dimensional space and in order for “everything to come together correctly and accurately,” they need to be completely synchronized. Moreover, if this did not happen, i.e. at some point something did not connect where it was needed, the growth and development of the heart does not stop. Everything is going as usual. After all, when some musician in the orchestra suddenly plays a false note, the orchestra will still finish the symphony. But the false sound will fly away and be forgotten, and few will pay attention to it, and the developing heart will remember it. And now the growing septum has nowhere to attach, or the valve has nothing to hold onto. This is how birth defects are formed. In order for the heart to become four-chambered and not two-chambered (as in the third week), it is necessary for its partitions to grow (interatrial and interventricular), so that the common arterial trunk is divided into the aorta and pulmonary artery, so that inside the common ventricle it is divided into right and left so that the aorta connects to the left ventricle so that the heart valves are fully formed. All this happens between the 4th and 8th weeks of pregnancy (at this time the length of the fetus reaches only 3.5–4 cm). By the end of the second month of pregnancy, the “inch” (3.5 cm) embryo is already fully formed. Obviously, the earlier in this process a disruption of normal development occurred, the more the heart is deformed, i.e. the more severe his congenital defect. The later this happened, the smaller the structural change will be and the easier it will be to correct the defect in the future.
Quoted from the book by G. E. Falkovsky, S. M. Krupyanko. The heart of a child. A book for parents about congenital heart defects
How to get treatment at the Scientific Center named after. A.N. Bakuleva?
Online consultations
Coronary heart disease (CHD)
Stroke
Diabetes
4193 08 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Coronary heart disease (CHD): causes, symptoms, diagnosis and treatment methods.
Definition _
Coronary heart disease (CHD) is an acute (transient) or chronic (stable) damage to the heart muscle (myocardium) caused by a decrease or cessation of blood flow through the coronary arteries.
Causes of coronary heart disease
Myocardial ischemia occurs when the myocardial demand for oxygen exceeds the ability to deliver it through the bloodstream through the coronary arteries. Normally, the coronary arteries have a reserve for expansion, providing a fivefold increase in coronary blood flow, and, as a result, oxygen delivery to the heart muscle. A discrepancy between oxygen delivery and muscle demand can occur under the influence of various factors.
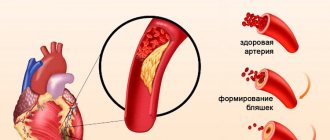
In 95% of cases, the cause of coronary heart disease is a decrease in its blood supply (insufficient oxygen supply) through the coronary arteries due to atherosclerotic narrowing of the lumen of the vessel.
The course of the disease is determined by the presence and further growth of an atherosclerotic plaque, which can block the vessel completely or partially. When blood pressure increases, the sclerotic endothelium of the vessel is easily damaged, blood penetrates into the plaque, the blood clotting process is activated and a blood clot is formed, which can partially or completely block the vessel.
A significant role in the development of IHD is played by disturbances in the movement of blood through the vessels and changes in the rheological properties of blood (the ability of blood to flow).
The formation of a blood clot, especially against the background of vessel spasm, can lead to complete or partial blockage.
In 5% of cases, the cause of IHD is congenital anomalies of the origin of the coronary arteries, Marfan and Ehlers-Danlos syndromes with aortic root dissection, coronary vasculitis in systemic connective tissue diseases, Kawasaki disease and Hurler syndrome, infective endocarditis, overdose of vasoconstrictor drugs and certain narcotic drugs, syphilitic mesaortitis and other conditions.
There are factors that provoke the development of coronary heart disease that can be influenced: dyslipoproteinemia (violation of the normal ratio of blood lipids); arterial hypertension; diabetes; smoking; low physical activity; obesity; stress. And also those risk factors for the development of coronary artery disease that cannot be changed: male gender, age, family history of cardiovascular diseases (myocardial infarction or ischemic stroke in close relatives: in women - up to 65 years, in men - up to 55 years).
Classification of IHD
I. Acute myocardial infarction (MI).
- According to the stage of the disease:
- developing – from 0 to 6 hours;
- acute – from 6 hours to 7 days;
- healing (scarring) – from 7 to 28 days;
- healed - starting from the 29th day.
- According to the depth of the lesion:
- transmural MI (necrosis of the entire thickness of the heart muscle);
- Q-wave (Q wave appears on the ECG);
- not Q-generating.
- By localization:
- front;
- lower;
- myocardial infarction of other specified locations;
- myocardial infarction of unspecified localization.
- Based on the presence or absence of persistent ST segment elevation on the ECG:
- myocardial infarction with ST segment elevation on ECG;
- myocardial infarction without ST segment elevation on ECG.
II. Unstable angina (a period of ischemic heart disease that threatens the development of myocardial infarction).
- New-onset angina.
- Progressive angina.
- Variant angina (Prinzmetal's angina).
III. Chronic ischemic heart disease.
- Angina pectoris I-IV FC (functional class).
- Previous myocardial infarction.
Symptoms of coronary heart disease
Coronary heart disease can have a relatively benign course over many years. The progression of atherosclerosis of the coronary vessels leads to the development of the disease.
The most common form of coronary artery disease is angina pectoris, in which the most common complaint of patients is squeezing or pressing pain in the chest. The pain can radiate to the left arm, back or neck, lower jaw, less often to the area under the xiphoid process, and last from 2 to 5 or even 20 minutes. It occurs during physical exertion or severe psycho-emotional stress. After stopping physical activity or 1-3 minutes after taking nitroglycerin, the pain quickly disappears.
As the disease progresses, there comes a time when even minimal exertion is enough for an angina attack, and finally, attacks begin to occur at rest. Some patients may experience pain while lying down due to increased blood flow to the heart.
It is necessary to take into account that pain that occurs with other diseases (neuralgia, gastralgia, cholecystitis, etc.) can provoke and intensify existing angina.
When the blood circulation of the heart muscle is disrupted with the development of a focus of necrosis (tissue death), myocardial infarction occurs. A heart attack (from the Latin infarcire - to stuff, stuff) is the necrosis of organ tissue due to an acute lack of blood supply.
The pain of myocardial infarction is significantly greater in intensity and duration than a normal angina attack.
The pain is not relieved by nitroglycerin and its duration can vary - from 1 hour to several days. Sometimes myocardial infarction is accompanied by weakness, dizziness, headache, vomiting, fainting, and loss of consciousness. The patient looks pale, his lips are blue, and he is sweating.
Diagnosis of coronary heart disease
The diagnosis of “coronary heart disease” is established by a combination of complaints, information about the course of the disease, data from laboratory and instrumental examination methods.
For all patients with suspected ischemic heart disease, the following questions are asked:
- current or past smoking;
- the presence of cardiovascular diseases and/or deaths from cardiovascular diseases in the patient’s immediate relatives (father, mother, siblings);
- previous cases of seeking medical help and the presence of previously registered electrocardiograms, studies and conclusions;
- comorbidities to assess additional risks;
- medications taken.
The following studies are recommended for all patients with coronary artery disease or suspected coronary artery disease at initial consultation:
- clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes);