Anemia - what is it and how dangerous is it?
This disease is also called anemia. This is a clinical-hematological syndrome that can occur as a consequence of one or another pathology. Hemoglobin protein is synthesized in the bone marrow with the participation of iron and is a component of erythrocytes - red blood cells. It delivers oxygen to the tissues and also helps to utilize carbon dioxide, delivering it to the lungs.
Such an important function easily explains the dangerous consequences of anemia. Firstly, even in conditions of a lack of iron in the diet, the body will fight anemia with all its might: first there will not be enough iron in the tissues and organs, and only lastly in the blood. This means that anemia often accompanies serious bone marrow diseases, tumors, and severe hematological diseases. It is important to pay attention to anemia as early as possible for this reason.
Secondly, a decrease in hemoglobin levels can lead to the following consequences:
- weakening of protective forces and increased susceptibility to aggressive environmental factors;
- decreased physical endurance and tolerance to intellectual stress;
- high risks of developing heart disease;
- high risks of developing purulent-septic processes.
Pregnant women deserve special attention. Anemia during pregnancy can lead to a high probability of spontaneous abortion, fetal malnutrition and intrauterine growth retardation, the appearance of hypoxia, and discoordination of labor. Physiological blood loss during childbirth or during a cesarean section will not cause complications in a healthy woman, but in an expectant mother with anemia it can also cause serious consequences.
Functions of iron in the body
The main studied processes occurring with the participation of iron include:
- blood cell formation;
- synthesis of hemoglobin and myoglobin;
- supplying body tissues with oxygen and evacuating carbon dioxide;
- synthesis of ATP (energy carrier molecules) from blood glucose;
- synthesis of cytochromes (P450) and enzymes (catalases) - natural antioxidants involved in the processing of drugs, xenobiotics and the removal of hydrogen peroxide;
- DNA synthesis;
- participation in the regeneration of cells and tissues;
- synthesis of hormones and neurotransmitters;
- regulation of thyroid function;
- regulation of immune system function;
- participation in the processes of physical and psychomotor development.
Symptoms of anemia
Symptoms of anemia and treatment options may vary in patients of different age groups, gender, and general health. The most characteristic signs are the following:
- pallor of the skin (from white to yellowish) and mucous membranes;
- hair loss (not patchy baldness, but uniform hair loss);
- brittle nails, changes in the structure of the nail plate, suddenly appearing white spots on the nails;
- change in taste sensations, burning sensation on the tongue;
- cracks in the corners of the mouth;
- menstrual cycle disorders in women;
- decreased physical activity, resistance to physical activity;
- muscle weakness;
- increased drowsiness;
- rapid mood changes, irritability;
- dizziness, periodic headaches, less often fainting;
- ringing in the ears, darkening or spots in the eyes;
- unusual gastronomic preferences, for example, the desire to taste paints, soil, chalk, etc.;
- pain behind the sternum, usually in the heart area.
In each specific case, not all of the listed symptoms may be observed. Sometimes anemia is discovered by chance, during the diagnosis of general health, when the patient came to the doctor for another reason. Thus, frequent respiratory diseases are a common consequence of anemia, and consulting a doctor allows you to identify the true causes of constant ailments.
Anemic syndrome
This syndrome is manifested by nonspecific signs characteristic of all anemias:
- shortness of breath that appears with minimal physical activity;
- interruptions in heart function;
- dizziness when changing body position;
- tinnitus.
The severity of the above symptoms depends on the rate of decrease in hemoglobin. Iron deficiency anemia has a chronic course, so patients are able to adapt to its manifestations.
In some cases, the first complaints with iron deficiency anemia may be:
- fainting conditions;
- angina attacks;
- decompensation of vascular lesions of the brain.
Differences between anemia in adults and children
According to WHO, about 2 billion people in the world suffer from anemia. The majority are children of different ages. Almost half of them are preschoolers, and a little more than a quarter are young school-age patients. And in adults, the disease occurs quite often. This syndrome is dangerous for both children and adults, and in adults the treatment period is somewhat longer.
Anemia in children may be associated with a specific cause: periods of rapid growth. The mechanisms of hematopoiesis are still imperfect, and the growth spurt requires an increased amount of nutrients. This may be associated with a temporary decrease in hemoglobin levels in the blood. However, this is still not a variant of the norm, but a syndrome that deserves close attention from a doctor. Anemia can lead to decreased defenses, poor weight gain, loss of appetite, weakness, and tearfulness. Timely methods of diagnosing and treating anemia will allow you to correct the condition and prevent complications.
The most dangerous complication of iron deficiency anemia (IDA) in adults is hypoxic coma. With high blood loss, it can cause death. Therefore, it is important to consult a doctor in time.
Causes
A necessary condition for the development of deficiency is the excess of iron consumption by tissues over its intake. Iron deficiency is caused by the following conditions (listed by degree of prevalence):
Blood loss
chronic (daily blood loss 5-10 ml)
- frequent nosebleeds;
- stomach and intestinal bleeding;
- heavy menstruation;
- kidney pathology with characteristic hematuria.
Acute (massive blood loss)
- injuries, extensive burns;
- uncontrolled donation;
- pathological bleeding (for example, uterine bleeding in oncopathology, etc.).
Insufficient iron intake
- exhausting diets and starvation;
- unbalanced diet;
- vegetarianism.
Decreased levels of absorbed iron
- gastrointestinal diseases, helminthic infestation;
- old age and infancy.
Increasing the level of essential iron
- active growth (1-2 years and adolescence);
- pregnancy, lactation (the need for iron doubles to 30 mg/day);
- formation of the menstrual cycle;
- physical activity, sports;
- frequent inflammations (ARVI, etc.).
Congenital anemia in children
- premature pregnancy
- anemia in a pregnant woman.
Why does anemia occur?
Anemia can be caused by many factors. There is often a combination of causes that quickly lead to blood disorders. The most common factors for the development of anemia:
- diet features. This is the most insidious reason. The lack of food rich in iron and B vitamins may not be taken seriously by a person. This is observed with a meager diet in women trying to lose extra pounds, the need to follow a certain table for gastrointestinal diseases, etc.;
- dysfunction of the digestive system. Even a complete diet does not guarantee the absence of anemia if iron cannot be absorbed in full due to gastrointestinal diseases. Iron absorption occurs in the stomach and upper small intestine. Diseases of these organs can lead to disruption of the process and the development of IDA;
- diseases leading to disruption of red blood cell production in the bone marrow. Such diseases include pathologies of the kidneys and endocrine system, protein depletion, chronic infections, cancerous tumors;
- hemolysis. This is a condition in which red blood cells are destroyed prematurely. Normally, physiological hemolysis occurs no earlier than after 120 days—that’s how long the red blood cell “lives.” In pathological conditions, the lifespan of red blood cells decreases, causing anemia. This may be due to long-term drug therapy, infectious diseases, rheumatism, systemic diseases (scleroderma, etc.), kidney diseases, etc.;
- chronic blood loss. Blood loss is a common cause of anemia. These include heavy menstruation in women or a short (21 days or less) menstrual cycle, frequent nosebleeds or bleeding gums, gastrointestinal bleeding, non-healing wounds in people with diabetes, previous surgeries, childbirth, etc.
Anemia is always the result of an underlying disorder, so it is important to get accurate information about the causes. It is not recommended to engage in self-diagnosis and self-medication. Taking iron supplements can correct the condition, but will not get rid of the underlying disease, so it will not be fully effective and there is a high probability of relapse.
The approach to treating anemia depends on what causes the disease. Thus, secondary causes of the development of the syndrome include:
- refusal of protein foods, fasting due to life circumstances or beliefs. If a person is forced or prefers to give up food of animal origin and does not find a replacement for it in terms of iron content, deficiency and associated anemia develop;
- pregnancy. Hormonal changes, an increased need for vitamins and microelements can cause deficiency, including iron; anemia in pregnant women develops quite often. It is important to regularly visit an obstetrician-gynecologist and get tested on time so as not to miss possible violations;
- blood donation. Although blood donation is carried out taking into account safe blood loss, the risks of developing anemia increase. You should consult your doctor if you are acting as a donor;
- professional sports or increased physical activity. This is due to the fact that muscles require increased amounts of iron. The peculiarity of this cause is that anemia occurs in an erased form, because usually an athlete leads an active and healthy lifestyle. It is important to pay attention to fatigue, intolerance to previously habitual stress, and shortness of breath.
Other mechanisms affecting iron levels
It is important not only to receive the mineral from food (the body does not produce iron), but also to the correct process of its absorption and transfer.
A special protein (transferrin) is responsible for the absorption of iron molecules from the duodenum. It delivers Fe to the bone marrow, where red blood cells are synthesized. The body forms a “warehouse” in the liver cells for rapid replenishment in case of acute deficiency. The reserves are stored in the form of hemosiderin.
If you decompose all the iron-containing forms into parts, you get the following:
- 2/3 is hemoglobin;
- for reserves in the liver, spleen and bone marrow in the form of hemosiderin - 1 g;
- for the transport form (serum iron) - 30.4 mmol/l;
- for the respiratory enzyme cytochrome oxidase - 0.3 g.
Accumulation begins in the prenatal period. The fetus takes some of the iron from the mother's body. Maternal anemia is dangerous for the formation and development of internal organs in the child. And after birth, the baby should receive it only with food.
Excess mineral is eliminated through urine, feces, and sweat glands. Women from adolescence to menopause still have a path of menstrual bleeding.
- About 2 g of iron is excreted per day, which means that no less amount should be taken from food.
Maintaining the necessary balance to ensure tissue respiration depends on the correct functioning of this mechanism.
Classification of anemia
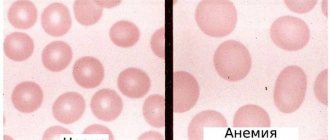
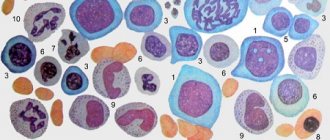
Anemia is classified according to the color index, which shows the level of saturation of the red blood cell with hemoglobin. The following types of syndrome are distinguished:
- hypochromic (iron deficiency, thalassemia, anemia associated with a lack of vitamin B6, etc.);
- normochromic (hemolytic, posthemorrhagic, i.e. resulting from blood loss/surgery, aplastic, etc.);
- hyperchromic (vitamin B12 deficiency, folate deficiency, etc.).
We see that anemia is not always synonymous with iron deficiency. Deficiency of B vitamins can also cause the development of the syndrome, and quite often it is associated with diet or absorption of nutrients in the intestines. And in this regard, independent diagnosis is impossible: only a doctor can determine the type of anemia, identify the causes and correctly correct the condition.
Treatment also depends on the severity of the anemia. It is determined by the severity of the decrease in hemoglobin levels. There are three degrees of severity:
- light. Hemoglobin level from 90 g/l;
- average. Hemoglobin level 70–90 g/l;
- heavy. Hemoglobin level is less than 70 g/l.
How long should you take iron supplements?
- If the treatment is effective, then on days 10-12 the number of young red blood cells – reticulocytes – increases sharply in the blood.
- After 3-4 weeks, hemoglobin increases.
- After 1.5-2 months, complaints disappear.
- Iron deficiency in tissues can be eliminated only after 3 months of continuous use of iron supplements - this is how long the course of treatment should continue.
Thus, iron deficiency anemia is a common and well-studied, but not harmless disease. Low hemoglobin levels are just the tip of the iceberg, which hides serious tissue changes associated with iron deficiency. Fortunately, modern drugs can eliminate these problems - provided that the treatment is completed and the causes, if possible, are eliminated.
Features and diagnostic methods
Diagnosis of anemia includes not only determining the fact of a decrease in hemoglobin levels. The doctor must understand the causes, assess the general state of health, and exclude severe pathologies that occur in a latent form, if they were not detected earlier. For this purpose, laboratory tests may be involved: a detailed clinical blood test is required. It will help assess the size, structural and other characteristics of blood cells.
The content of hemoglobin, erythrocytes, platelets, leukocytes, and several calculated erythrocyte indices are assessed. These indicators allow you to obtain data on the size, hemoglobin saturation, and uniformity of red blood cells. Determination of reticulocytes (young red blood cells) helps to understand the nature of anemia, as well as assess the reactivity of the hematopoietic system to the pathological condition. This is also important for monitoring treatment - the doctor can evaluate the response to the course of therapy.
Determination of erythrocyte parameters includes assessment of the following indicators:
- red blood cell count;
- hemoglobin concentration;
- average erythrocyte volume;
- hematocrit;
- width of distribution of red blood cells by volume;
- normoblasts.
The average volume and diameter of red blood cells are also assessed. An increase in these parameters may indicate a vitamin B12 deficiency. A decrease indicates a lack of iron.
Reticulocytosis or quantitative indicators of immature red blood cells may indicate certain features of bone marrow activity. In aplastic anemia associated with bone marrow suppression, the indicator may drop to zero. Reticulocytosis increases with blood loss and hemolytic anemia.
The doctor will also pay attention to those blood parameters that are not directly related to red blood cells. For example, an increase in platelet levels may be a consequence of IDA due to chronic blood loss. If leukocytes and platelets are reduced, we can talk about aplastic anemia. Detection of blast cells requires special attention; there is a high probability of acute leukemia.
Although laboratory diagnosis is critical, it is important to resort to other research methods. An examination is mandatory - the doctor evaluates the color of the skin and mucous membranes. Palpation helps to suspect possible disorders of internal organs and tumors. A thorough survey allows you to identify lifestyle features, probable causes, and the duration of symptoms.
If you have symptoms of anemia, it is important to consult a general practitioner or hematologist. He will order the necessary tests and make suggestions as to the reasons. To clarify them, it is sometimes necessary to resort to additional diagnostic tools:
- fibrogastroduodenoscopy. Assessing the condition of the mucous membranes of the esophagus and stomach will help in identifying gastric bleeding;
- Ultrasound of the liver and kidneys;
- examination of the pelvic organs in women;
- CT or MRI if indicated;
- colonoscopy;
- X-ray of the lungs, etc.
A complete list of diagnostic methods is not required: a specialist will find out the possible causes and refer you to certain studies according to indications. If necessary, he can refer you to another doctor. So, if the cause of anemia is heavy and prolonged menstruation or a short cycle, an examination by a gynecologist will be required. Detection of gum problems (bleeding) and symptoms of periodontal disease will require a visit to a periodontist. Frequent nosebleeds are a reason to consult an otolaryngologist, assess blood pressure parameters, etc.
Hyposiderosis
Symptoms of hyposiderosis are associated with a lack of iron in tissues. This is accompanied by:
- deterioration of the hair structure with splitting of the ends;
- signs of asthenia;
- excessive dry skin, which can be minimally corrected with moisturizing cosmetics;
- pathological changes in the nails, transverse striations of the nail plate, changes in its shape;
- violation of the body’s protective properties with frequent viral diseases;
- the appearance of angular stomatitis, manifested by cracks with areas of inflammation in the corners of the mouth;
- signs of inflammatory lesions of the tongue;
- change in skin color to a pale greenish tint;
- unusual eating habits (desire to eat chalk, ashes and other substances);
- addiction to unusual smells;
- blue sclera due to dystrophic changes in the cornea of the eye against the background of iron deficiency.
According to recent studies conducted by pediatricians and hematologists, children with tissue iron deficiency experience mental retardation. This is due to a disruption in the processes of myelination of nerve fibers with a decrease in the electrical activity of the brain. Also, in young patients there is a high risk of developing heart failure, however, clear mechanisms of myocardial damage in hyposiderosis have not been identified.
Treatment of anemia
Clinical recommendations for the treatment of anemia depend on many factors: gender, age and condition of the patient, type and severity of the syndrome. There are several general principles that apply in medical practice. These include the following:
- Mandatory diet correction for B12 deficiency and iron deficiency anemia. This complements the main course of treatment - taking medications that will compensate for the lack of substances;
- timely correction of deficiency of vitamins and microelements in pregnant women;
- mandatory consultation with a specialist when identifying specific causes: chronic bleeding, features of the functioning of the reproductive system in women, etc.;
- examination by a specialist in cases where anemia has caused complications in organs and systems. For example, consultation with a cardiologist for angina pectoris, low blood pressure, etc.
An integrated approach allows you to cope with the cause of the syndrome, rather than mask the symptom, and also eliminate or correct the consequences of the disease.
Diet
The International Association of Hematologists states that by normalizing the eating behavior of a patient with signs of mild iron deficiency anemia, it is possible to significantly normalize blood counts and not resort to the use of iron supplements to eliminate the iron deficiency state. For patients with severe anemia, the use of a specialized diet is indicated as an addition to the main treatment.
The fundamental principles of therapeutic nutrition for iron deficiency anemia are a sharp limitation in the consumption of fats of both plant and animal origin, as well as enrichment with foods containing large amounts of protein. It has been proven that carbohydrates do not affect the body's absorption of iron in any way, so their consumption should not be limited.
In order to replenish the level of iron necessary for normal hematopoiesis, it is necessary to include in the patient’s diet a large amount of foods containing iron (liver, beef tongue, lean turkey meat, red types of sea fish, buckwheat and millet cereals, blueberries and peaches). A large percentage of iron is also found in all types of greens, beef and eggs. Among fruits, preference should be given to persimmons, quinces and apples, raw or baked.
It is recommended that patients with iron deficiency anemia completely exclude dairy products and black tea from their diet, as they contain substances that interfere with the absorption of iron. And, on the contrary, synergistic products that should be consumed in large quantities together with iron-containing products are those that contain a high percentage of vitamin C (sorrel, currants, sauerkraut, freshly squeezed fruit and citrus juices with pulp).
The main objectives of the treatment of anemia:
- eliminating the cause. Identification and elimination of the source of chronic blood loss, normalization of iron absorption in the intestines, reduction of blood loss during menstruation, etc.;
- replenishing the lack of important substances;
- prevention of the development of dystrophic changes in internal organs, restoration of their normal function.
It is important to remember that it is impossible to eliminate anemia with diet alone. This is explained by the fact that the absorption of iron from food is no more than 2.5 mg/day. From drugs, it is absorbed 20 times more. However, following a diet is very important as an addition to a course of drug therapy. Patients are recommended foods containing large amounts of digestible protein and iron.
Meat contains heme iron, which is absorbed by 30%. Also, liver, eggs and fish contain iron, which is absorbed by 10–15%. The microelement is also found in products of plant origin; absorption of Fe from legumes, spinach, soybeans, dill, and bread is up to 3–5%. It is advisable to include apples, pomegranates and pomegranate juice, beets, and buckwheat in your diet. But in terms of their overall benefits, the absorption of iron ions from them is limited, as demonstrated by numerous studies. That is why it is important to understand that eating apples will not help cure anemia; this is nothing more than a myth.
People who eat meat get more iron than those who are vegetarian. Strict vegetarianism can cause anemia because vegetables and grains contain substances that interfere with the absorption of iron. If you follow a normal, balanced diet, they do not entail serious consequences.
It is important to understand that a balanced diet helps cover the daily requirement, but will not eliminate iron deficiency. The basis of correction is drug therapy.
Blood transfusions (transfusions) are performed according to vital indications. They are usually carried out when hemoglobin drops below 50−40 g/l.
If the situation is not so severe, the doctor prescribes medication. IDA is corrected with oral medications; the course of treatment in adults is quite long. Interim monitoring is mandatory - detailed blood tests are performed. The principles of treatment in this case are as follows:
- prescribing iron supplements with a dose of divalent or trivalent iron sufficient for a person;
- supplementing the course of treatment with substances that enhance absorption. Succinic and ascorbic acid are used;
- refusal of antacids, oxalates and other drugs that reduce iron absorption whenever possible or recommendations for taking them at different times;
- therapy for at least 6–8 weeks until normalization and for at least another 4 weeks after improvement.
Let’s take a closer look at the recommendations about avoiding medications and foods that interfere with the absorption of iron. This can be prevented by phosphoric acid, calcium, tannin, phytin, and salts. Therefore, you should not drink tea, coffee, or Coca-Cola at the same time as taking iron.
For women suffering from long and heavy menstruation, not associated with diseases of the endocrine and reproductive systems, it is important to maintain monthly short courses of treatment: take average therapeutic doses of Fe for 3-5 days.
Clinical guidelines for the treatment of anemia dictate regular monitoring. The criterion for the effectiveness of therapy is an increase in reticulocytes at least three times 7-10 days after the start of treatment.
All iron preparations are classified into two groups: ionic (salt or polysaccharide compounds of ferrous iron) and non-ionic, consisting of a ferric iron complex.
Ferrous sulfate is included in mono- and polycomponent products and is well absorbed, and also has a relatively smaller list of side effects. Chloride compounds are absorbed less well and can also cause undesirable consequences: metallic taste in the mouth, dyspepsia, darkening of tooth enamel, etc. Modern treatment standards call for the use of ferrous or trivalent iron preparations.
Sometimes iron supplements are indicated to be administered parenterally. This is relevant for cases where there is a malabsorption in the intestine and other features. The main indications for drip infusion are the following:
- impaired intestinal absorption - malabsorption, previous surgery, etc.;
- intolerance to oral medications;
- the need for quick saturation. For example, in case of emergency surgery;
- treatment with erythropoietin: with it, the need for iron sharply increases, since it is actively consumed by red blood cells.
Important: parenteral administration requires no more than 100 mg/day. Otherwise, there is a risk of complications.
Treatment regimens for anemia associated with vitamin deficiency include additional intake of vitamin B12, folic acid and certain microelements.
Treatment of anemia associated with diseases of the hematopoietic organs and bone marrow tumors is developed individually and requires special attention to the cause.
Popular iron supplements
Currently, doctors and patients are offered a wide selection of medications that increase the iron content in the body.
The most effective medications for increasing iron concentrations include:
- Ferrum Lek;
- Maltofer;
- Ferroplex;
- Hemofer;
- Ferroceron; (colors urine pink);
- Tardiferon;
- Ferrogrademet;
- Heferol;
- Ferograd;
- Sorbifer-durules.
Preparations for parenteral administration are prescribed for malabsorption of iron in the gastrointestinal tract (gastric resection, peptic ulcer of the stomach and duodenum in the acute phase, resection of large areas of the small intestine).
When prescribing medications for intravenous and intramuscular administration, first of all you need to remember about allergic reactions (feelings of heat, palpitations, pain behind the sternum, in the lower back and calf muscles, metallic taste in the mouth) and the possible development of anaphylactic shock.
The list of ferrum-containing drugs is not a guide to action; prescribing and calculating the dose is the responsibility of the attending physician. Therapeutic doses are prescribed until hemoglobin levels normalize, then the patient is transferred to prophylactic doses.
Features of prevention
Prevention of anemia should be carried out in case of hidden signs of iron deficiency or the presence of risk factors for the development of the syndrome. Thus, if there are grounds for the rapid development of anemia, it is important to examine the level of hemoglobin and serum iron annually. The following patients are at risk:
- blood donors, especially females;
- pregnant women, especially those with frequent pregnancies;
- women with long (more than 5 days), heavy menstrual bleeding, short cycle (21–25 days);
- children from multiple pregnancies, premature babies;
- children during growth spurts;
- people with dietary restrictions;
- people suffering from chronic bleeding. For example, with hemorrhoids, etc.;
- patients taking non-steroidal anti-inflammatory drugs;
- professional athletes and people engaged in active physical labor.
Side effects
The most common side effects observed during treatment with iron supplements are a metallic taste in the mouth, darkening of tooth enamel, allergic skin rashes, digestive disorders as a result of irritation to the mucous membrane of the digestive tract, especially the intestines (loose stools, nausea, vomiting). Therefore, the initial doses of drugs should be 1/3–1/2 of the therapeutic dose, followed by increasing them to the full dose over several days in order to avoid the occurrence of severe side effects.
Intramuscular administration of iron supplements is carried out only under strict indications due to the development of pronounced local and systemic side effects. Indications for intramuscular administration of iron preparations are as follows: diseases of the digestive tract (poor intestinal absorption syndrome, ulcerative colitis, chronic enterocolitis, gastrointestinal bleeding) and intolerance to iron-containing preparations when taken orally.
Contraindications to the prescription of iron supplements are anemia not caused by iron deficiency (hemolytic, aplastic), hemosiderosis, hemochromatosis.
Prevalence of IDA
Iron deficiency anemia in women is a common pathological condition. Thus, according to WHO (2015), severe iron deficiency is observed in every third woman of reproductive age and in every second pregnant woman, being an important cause of chronic fatigue and poor health, and the third most common cause of temporary disability in women aged 15– 44 years old [12, 19]. In the Russian Federation, despite active preventive and therapeutic measures, the prevalence of IDA remains very high. For example, in Moscow, anemia occurs in almost 38% of gynecological patients [20, 21] and is the most common concomitant pathological process and the first manifestation of the underlying disease, determining the severity of its course and treatment tactics. The main reasons for the development of IDA in women are heavy menstrual bleeding, pregnancy, childbirth (especially repeated ones) and lactation. Anemia often accompanies uterine fibroids, adenomyosis, hyperplastic processes in the endometrium, and ovarian dysfunction. During normal menstruation, 30–40 ml of blood is lost (which is equivalent to 15–20 mg of iron). The critical level corresponds to a blood loss of 40–60 ml, and with a blood loss of more than 60 ml, iron deficiency develops. In women suffering from abnormal uterine bleeding of various origins, the amount of blood lost during one menstruation can reach 200 ml (100 mg of iron) or more. In such situations, the loss of iron exceeds its intake and IDA gradually forms [20].
The most important medical and social problem is anemia in pregnant women, which, according to WHO, is detected in 24–30% of women in economically developed countries and in more than 50% of women in countries with low economic levels [3, 22].
A survey of pregnant women conducted as part of clinical studies in the 2000s showed a high incidence of anemia even among residents of prosperous European countries. Thus, in Belgium (n=1311), Switzerland (n=381) and Germany (n=378) iron deficiency was diagnosed in 6% and 23% (serum ferritin (SF) <15 μg/l) in the first and third trimesters, respectively, of Belgian women; in 19% (SF<12 µg/l) - in Switzerland and Germany. The prevalence of IDA (Hb <110 g/L, SF <15 μg/L) was 16% in Belgium and 3% in Switzerland, although 65–66% of Belgian and Swiss women received dietary iron supplementation during pregnancy. In Germany, IDA was diagnosed in 12% of women [23].
In Russia, according to the Ministry of Health, the incidence of anemia in pregnant women varies from 39% to 44%, in postpartum women - from 24% to 27% [24]. A 2021 systematic review and meta-analysis found that in low- and middle-income countries, pregnancy anemia increases the likelihood of preterm birth by 63%, low birth weight by 31%, perinatal mortality by 51%, and neonatal loss by 2 ,7 times [25].
During pregnancy, there is a significant physiological increase in the need for iron for the normal functioning of the placenta and fetal growth. The total amount of iron required for a normal pregnancy is 1000–1200 mg. To complete a normal pregnancy without developing iron deficiency, a woman must have iron stores in the body at conception of ≥500 mg, which corresponds to an SF concentration of 70–80 μg/L [20, 23].