Causes and symptoms of diseases
Both pathologies have a similar course at the initial stage, but arise for different reasons and require special therapy. With hemorrhoids, inflammation of the blood vessels occurs, which is why the hemorrhoids increase in size until they come out during defecation, and in the later stages - even when walking calmly. This condition is accompanied by severe pain, bleeding and a high risk of additional trauma to the rectal area. Based on the current location of the nodes, internal and external hemorrhoids are diagnosed. Stagnation of blood in these vascular formations, leading to their enlargement, occurs due to:
- poor nutrition (drinking alcohol, too spicy, spicy and fatty foods, lack of certain dietary fibers, etc.);
- sedentary work;
- excessive strain during bowel movements;
- physiological changes that occur during pregnancy and childbirth;
- hereditary predisposition;
- too intense physical activity;
- frequent constipation.
Anal fissures are vertical defects in the mucous membrane of the rectum, usually forming at the border with the skin. Their length is usually 1.5-2 cm, depth – 2-3 mm, width – 2-5 mm. The disease occurs both independently and as a complication of hemorrhoids. Swelling appears at the site of the rupture and an inflammatory process begins, which progresses with each subsequent bowel movement. Pathogenic microorganisms constantly enter the wound with feces, therefore, in the absence of adequate therapy, there is a high risk of suppuration and the development of other complications. In case of circulatory disorders, as in cases with chronic hemorrhoids, the healing of the anal fissure is even more difficult and its ruptures recur.
The main causes of the disease:
- mechanical injury to the rectum due to high density of feces or during anal sexual intercourse;
- ruptures during difficult childbirth;
- haemorrhoids;
- passive lifestyle;
- the presence of condylomas in the anal area;
- frequent constipation;
- proctitis, anoproctitis;
- itching in the rectal area;
- dysentery;
- colitis.
Rectal fistulas
According to statistics, approximately 95% of patients with rectal fistulas associate the onset of the disease with a history of purulent inflammation (acute paraproctitis). It is not advisable to postpone radical surgical treatment for a long time, since exacerbation of paraproctitis can recur and the inflammatory process can lead to deformation of the surrounding tissues, including the development of anal muscle insufficiency. For most rectal fistulas, excision of the fistula is performed (with or without suturing the wound). Surgical treatment of simple fistulas leads to a permanent cure in approximately 95% of cases and is not accompanied by any serious complications. Complex fistulas (so-called deep trans- and extrasphincteric) can also be cured without functional impairment.
Epithelial coccygeal tract
In proctological practice, every 10 patients (in men, on average, three times more often) are found to have fistulas in the coccyx area. This is a congenital anomaly - the epithelial coccygeal duct. Patients are often unaware of their illness, or their complaints are limited to a small constant discharge above the anus, wetness of the skin between the buttocks, and itching. In other cases, often after an injury, suppuration suddenly occurs in the coccyx area, after opening which a non-healing fistula remains. Prolonged course of the epithelial coccygeal tract without proper treatment or self-medication leads to the formation of secondary fistulas; the entire sacrococcygeal region is affected by the inflammatory process. The prognosis for radical treatment of the epithelial coccygeal tract at any stage of the disease is favorable, complete recovery occurs.
Perianal genital warts
Pointed perianal condylomas are gray-pink papillary formations between which unaffected skin is visible, sometimes in the form of papillae that merge and form whole conglomerates that can cover the anus. Sometimes there are giant condylomas up to 20 cm or more in diameter. It has now been established that condylomas are caused by human papillomavirus (HPV) types 6 and 11. The disease is usually sexually transmitted. They must be distinguished from flat condylomas, characteristic of syphilis and lesions in patients with AIDS. Surgical treatment is most often undertaken in the presence of large nodes and damage to the anal canal. Excision is performed with a scalpel, or an electric knife, or a laser. Sometimes, in the presence of large condylomas, surgical removal is not performed at once, since the resulting extensive wounds can lead to deformation in the area of the anus.
Patient consultations in our department are free and are held daily on weekdays. You can pre-agreed the time of your visit by phone. Read more on the website: https://www.surgery-future.ru/proktologiya
Modern methods of treatment
Proctologists use local medications (ointments, suppositories), general medications, therapeutic diets, minimally invasive and classical surgical interventions to treat hemorrhoids and anal fissures. In the initial stages, as a rule, drug treatment and physical procedures are used, which are effective, atraumatic and painless.
In medicine, they give preference to gentle methods of therapy, which provide a pronounced result and do not require long-term rehabilitation. How to treat fissures in hemorrhoids in a particular case, doctors decide based on the medical history, the neglect of the pathological process and the patient’s well-being. It can be:
- Sclerotherapy is the “gluing” of vessels supplying enlarged hemorrhoids with a special preparation. Effective for stage 2-3 hemorrhoids with rectal bleeding. Not used for severe inflammation with prolapse of nodes.
- Ligation with latex rings - complete blocking of blood flow to hemorrhoids. The method is used for advanced forms of hemorrhoids. In the absence of nutrition, tissues die and spontaneously separate from healthy ones after 7-10 days.
- Laser coagulation is layer-by-layer burning of hemorrhoids with a laser beam. The technology involves minimal trauma to the mucous membranes, the integrity of which is completely restored over the next few weeks.
- Desarterization HAL-RAR - treatment using the HAL-Doppler device. It is equipped with a special sensor that detects the hemorrhoidal artery and ligates it using self-absorbing threads. The method provides a precise effect of blocking the blood supply to inflamed vascular structures. The procedure is carried out using a rectoscope, which guarantees precise visual control of the process. Ligation of the arteries occurs without violating the integrity of the rectum, which allows the use of disarterization technology for internal hemorrhoids, as well as at stages 3 and 4. The technique is gentle, therefore it does not require hospitalization and does not impose restrictions on the usual lifestyle and physical activity.
- Radio wave therapy with the Surgitron apparatus is the destruction of pathologically altered cells by high-frequency radio waves. The impact is carried out pointwise through a very thin electrode that does not directly contact the skin or mucous membrane. Destruction occurs due to the evaporation of intracellular fluid, which is absolutely safe for healthy tissues and allows them to be preserved in full. Radio wave radiation does not leave an open wound field, and the treated area heals quickly and without discomfort.
Chronic fissure and aloe treatment - how effective and safe is it?
The most popular traditional medicine recipes are based on the use of aloe. As you know, aloe has anti-inflammatory and healing properties and can alleviate the suffering of the patient and relieve the acute state of the disease. Rectal suppositories are made from it, pieces of the plant are applied to the sore spot, and a variety of local preparations are made based on the juice. Treatment of hemorrhoids in the initial stages of the disease in this way is quite possible and is periodically used as the first conservative stage in the treatment process. However, before treating anal fissures with traditional methods, you should remember that self-medication is fraught with extensive negative consequences.
What is important to know about therapy?
The use of minimally invasive techniques is the main standard of modern proctology, since in most cases they allow you to get rid of hemorrhoids and anal fissure in one visit. A full examination and laboratory tests must be carried out first. To ensure maximum comfort during a proctological examination and obtain reliable medical information, special preparation is recommended. To do this, you need to cleanse the intestines with an enema or special laxatives prescribed by your doctor. After this, he will determine how to treat hemorrhoids and anal fissures, taking into account the existing indications.
What is easier to cure – hemorrhoids or anal fissure?
The method of treating anal fissure, like the treatment of hemorrhoids, is determined in each specific case and depends on the severity of the pathology. Very often, an anal fissure occurs as a result of the development of hemorrhoids and then treatment must be comprehensive. Treatment of anal fissure is very different from the treatment of hemorrhoids: as a rule, to treat fissures at an early stage of development, non-surgical correction of the disease that has arisen is used, and only if therapy does not give the desired result, radical methods are used - surgical excision of the anal fissure. The most modern and painless method of excision today is radio wave surgery, thanks to which the pathology is eliminated.
How do they occur and in whom are they more common?
Anal fissure is not only a medical, but also a social problem, as it causes discomfort to the patient. Fissure occurs equally often in both men and women.
Despite the long study of this disease, the exact etiology of anal fissure remains unknown.
The occurrence of anal canal fissures can be caused by defecation disorders (chronic constipation, diarrhea), mechanical injuries of the anal canal (anal sex, sex toys, etc.).
The onset of the disease is most likely caused by mechanical damage, which injures the mucous membrane of the anal canal.
There is a theory that the occurrence of a posterior anal fissure is associated with the peculiarity of the blood supply to the anal canal.
Against the background of the development of pain, the tone of the anal sphincter increases, which leads to a subsequent increase in muscle pressure of the anal sphincter.
Severe pain can be caused by excessive persistent contraction of the internal anal sphincter, leading to blockage of the vessels, which does not allow the fissure to heal on its own.
Pain is followed by spasm, spasm is followed by pain, and this is how a “vicious” circle develops with an anal fissure.
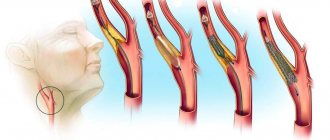
Rice. 7.
How is the initial consultation with a coloproctologist?
When applying for an appointment, no complex special preparation is required, which can take you out of your normal daily routine.
The doctor will listen to you, ask you about your complaints, how long the disease has been, and then conduct an examination.
The examination in our consultation room is carried out in the supine position with the legs raised on supports (lithotomy position).
On the eve of the consultation, it is necessary to make a microenema and perform hygiene of the perineal area.
After the examination, a specialist doctor will tell you about your disease, prescribe additional examinations if necessary and suggest the most optimal treatment method.
Is it possible to heal an anal fissure on its own?
Answer: Many patients are interested in whether an anal fissure can disappear without treatment. Yes maybe. But! - only if it is fresh and no more than one week old.
Safe scarring of the fissure, without the subsequent formation of gross fibrous changes - such as a sentinel polyp - is possible only with strict adherence to comprehensive measures. This is the normalization of stool, dietary nutrition, the use of softening and regenerating rectal agents. Well, if time has already been lost, and the crack has become chronic, the best solution would be gentle surgical treatment with a Surgitron radiofrequency scalpel. In addition to bloodless excision of the fissure and painless intervention, radiofrequency treatment provides rapid postoperative recovery and excellent cosmetic results.
How does cauterization of an anal fissure occur?
Cauterization of an anal fissure is called electrocoagulation, and is performed with an infrared laser. Laser coagulation of cracks is modern and widely used, but it is quite painful and is not indicated in all cases. It is not suitable in the fight against chronic fissures, and is effective only for fresh ruptures of the rectum (for a period of 3, maximum 4 weeks).
It is much more painless and effective to undergo radiofrequency treatment , which, like laser treatment, is called cauterization.
The essence of cauterization is laser or radio wave excision of scar perianal tissue along with a crack. Occurs under local anesthesia.
What is required for differential diagnosis of this disease?
A fissure can occur with inflammatory diseases of the colon, such as Crohn's disease or ulcerative colitis. Infectious diseases (syphilis, HIV, herpetic infection, etc.) can also contribute to the development of anal fissure. Tumor diseases such as cancer, melanoma, leukemia can manifest themselves in the same way as an anal fissure. The patient will experience pain in the anus and bleeding from the anus.
Rice. 8. Cancer of the anal canal with transition to the perianal skin