Calcium and potassium preparations are a group of medicines that contain salts of macroelements - calcium and potassium, respectively.
Macro- and microelements are a collective (generalized) name for mineral substances - food components that, together with vitamins, are involved in maintaining normal human life.
If minerals are needed by the body in relatively large quantities, they are called macroelements. Macroelements include magnesium, calcium, potassium, sodium, phosphorus, chlorine and sulfur.
The human body requires minerals called microelements in much smaller quantities. Microelements include zinc, iodine, selenium, iron, manganese, copper, etc.
The most important macroelements that regulate the normal functioning of the human body include calcium and potassium.
Calcium and potassium are active participants in many biochemical processes in the body, significantly influencing metabolism.
By depositing (accumulating) in the bones, calcium gives them strength and elasticity and prevents the occurrence of fractures. In addition, the importance of calcium is in the implementation of muscle contractions. Calcium is involved in the conduction of nerve impulses and the regulation of excitation processes in the brain. In addition, calcium ions play a key role in blood clotting and the formation of blood clots (thrombi), which is a key factor in stopping bleeding.
Potassium maintains osmotic pressure in cells and also regulates the acid-base balance of the body. Potassium is also involved in the conduction of excitation along nerve fibers, as well as in the transmission of impulses through the conduction system of the heart, and affects neuromuscular transmission.
With a balanced diet, the human body receives sufficient amounts of calcium and potassium from food. However, under certain conditions (for example, poor nutrition, significant physical activity, various pathological conditions, taking certain medications), there is a deficiency of these macroelements. In this case, drugs containing calcium or potassium are used.
General information
The human body is designed in such a way that as we age, all organs gradually wear out.
And in order for each organ to serve “without breakdowns” for as long as possible, it is important to ensure high-quality disease prevention. If we are talking about the most important organ - the heart, then prevention methods consist of giving up alcohol consumption and smoking, losing body weight, and normalizing lipid metabolism. However, in addition to the points described, the use of potassium and magnesium supplements will help prevent cardiovascular diseases and their complications. Why such medications are needed for the body, in what cases potassium and magnesium preparations are used, and why you need to consume foods containing magnesium and potassium will be discussed in the article below.
What are the benefits of magnesium and potassium?
Potassium
Taking potassium supplements is very important for the prevention of heart and vascular diseases. After all, potassium in the body promotes the functioning of the conduction system of the heart and ensures the regulation of blood pressure . It is important to take medications containing potassium not only for the heart. This mineral determines the transmission of excitation from nerve cells to muscles and is responsible for maintaining water and electrolyte balance. By activating enzymes , potassium participates in the regulation of protein and carbohydrate metabolism. It also takes part in the synthesis of proteins and the conversion of glucose into glycogen .
Potassium preparations in tablets help to activate urine flow.
Potassium is contained in tablets, the price of which is relatively low. However, some complex drugs have a higher cost.
You can replenish your reserves of this microelement by consuming foods high in it. A large amount of potassium is found in dried fruits (raisins and dried apricots), leafy greens, legumes, watermelons, melons, kiwi, etc. Slightly less of this trace element is found in potatoes, milk, and beef.
The adult body needs from 2 to 5 g of potassium per day from food (this depends on physical activity). However, it is important to know that approximately 90% of potassium is absorbed from food. This is provided that the absorption process occurs normally and there is no diarrhea or vomiting.
Magnesium
Magnesium in the body promotes the breakdown of glucose. It is involved in various enzymatic reactions that help increase cell stability and renewal. Due to the synthesis of B vitamins, magnesium improves the process of neuromuscular transmission. Therefore, magnesium preparations are indicated for various diseases. In particular, preparations with magnesium are effective for leg cramps.
If you take medications containing potassium, magnesium and calcium, vascular tone improves. Also, magnesium, when interacting with potassium, takes part in muscle contraction.
The use of magnesium is also advisable from the point of view that it activates the absorption of potassium and regulates the content of this trace element in the blood. The optimal ratio of potassium and magnesium in food is 2 to 1. This allows you to maintain the density of bone tissue and protect teeth from destruction.
Preparations containing magnesium are also taken “for the heart,” since this microelement stabilizes cell membranes, allowing potassium and chlorine ions to penetrate through them. This allows you to lower blood pressure and stabilize the heart rhythm.
The price of such drugs may vary. But it is not always necessary to take magnesium-containing medications. After all, a large amount of this microelement is found in food products - legumes, cereals, cabbage, seafood, fish, nuts, etc.
Magnesium is easily absorbed from consumed dairy products, although they contain relatively little of it. A person should receive 400 mg of this microelement per day.
What is hyperkalemia?
Hyperkalemia is a condition in which serum potassium levels exceed 5 mmol/L. Hyperkalemia occurs in 1-10% of patients admitted to hospitals.
Hyperkalemia is a condition in which serum potassium levels exceed 5 mmol/L.
Hyperkalemia occurs in 1-10% of patients admitted to hospitals. The number of patients with hyperkalemia has increased in recent years due to an increase in the number of patients taking medications that affect the renin-angiotensin-aldosterone system (RAAS). Potassium inside the human body
Potassium is the most important electrolyte in the human body.
It plays a key role in the conduction of nerve impulses and muscle contraction. 98% of potassium is concentrated in the intracellular fluid; the potassium concentration here reaches 140 mmol/l. Only 2% of potassium is found outside the cells, the concentration here is 3.8-5.0 mmol/l. The role of potassium in the body
Potassium is the main intracellular cation (a positively charged ion), in contrast to sodium, the main extracellular cation.
Functionally, potassium and sodium are related to each other:
- The creation of membrane potential, important for muscle contraction (skeletal and cardiac muscle), is ensured by maintaining a high concentration of sodium outside the cell and potassium inside the cell (sodium-potassium pump, see Fig. 1).
- Maintaining acid-base balance, osmotic balance, water balance
- Activation of many enzymes
Mechanisms of regulation of potassium metabolism
To maintain normal potassium balance (transport between intra- and extracellular fluid), a coordinated interaction of all regulatory mechanisms is required. The main mechanism for regulating potassium levels is its excretion by the kidneys . This mechanism is controlled by the adrenal hormone aldosterone . The presence of this mechanism ensures that, despite the high potassium content in food (from 40 mmol to 200 mmol), its level in the blood serum will be maintained at a constant level. Dysregulation of potassium levels, and, as a result, an increase in potassium levels in the blood, can alter the excitability of membranes. This means that the function of nerves, muscles, and heart will be impaired.
Fig. 1 Scheme of regulation of transmembrane potassium transport Potassium concentration inside cells is maintained by active transport of potassium using Na-K-ATPase and passively due to a concentration gradient. The rate of passive movement depends on the permeability of potassium channels in the cell membrane. Insulin and beta-2 adrenergic agonists, through cAMP, promote the uptake of potassium into cells by stimulating Na-K-ATPase. With insulin deficiency and the action of beta-2 blockers, the release of potassium from the cells increases, which leads to hyperkalemia. Acidosis, hyperosmolarity, and cell lysis also cause potassium leakage and an increase in potassium levels in the blood. In the diagram: ECF=extracelluar fluid (intracellular fluid); ICF=intracellular fluid Aldosterone is a mineralocorticoid hormone synthesized in the adrenal cortex from cholesterol.
Under the influence of aldosterone in the kidneys, tubular reabsorption (that is, reverse absorption from primary urine) of sodium ions increases: aldosterone stimulates the transition of sodium into the cells, and potassium - outward (into the intercellular space, that is, potassium then passes into the urine, released from the body) - see .fig.2. Aldosterone also increases the secretion of potassium and hydrogen ions by the kidneys. Thus, the body's sodium and extracellular fluid levels (the body retains water) increase. Aldosterone levels depend on sodium (Na+) and potassium (K+) levels. At high potassium concentrations and low sodium concentrations, the synthesis and secretion of aldosterone is enhanced. The most important influence on aldosterone levels is the renin-angiotensin system (see RAAS). Other factors also influence aldosterone levels. Many factors are involved in the development of hyperkalemia, which develops as a result of a decrease in potassium excretion or an increase in the release of potassium from cells.
Hyperkalemia may be false (pseudohyperkalemia), this should be excluded first (except in cases where emergency assistance is required).
Pseudohyperkalemia
Pseudohyperkalemia is a condition when the calcium level determined in the laboratory does not reflect the level of potassium in the body.
This is because intracellular potassium levels are very high and in certain situations it is released from the cells after blood is drawn. In such cases, to confirm true hyperkalemia, blood sampling should be repeated and plasma and serum potassium levels should be measured simultaneously. The concentration in the serum is 0.2–0.4 mmol/l higher than the concentration in plasma, which is associated with the formation of a clot and the release of potassium from cells into the serum. Table 1: Causes of pseudohyperkalemia
- Untimely analysis
- Taking blood from a vein into which potassium was injected
- Using too much pressure when applying a tourniquet or using a fist to fill the veins
- Hemolysis due to blood flow through a thin needle or traumatic venipuncture
- Long-term blood storage
- High leukocytosis or thrombocytosis (significantly increased white blood cell or platelet count)
- Unusual genetic disorders (familial hyperkalemia)
Hyperkalemia with increased potassium intake
Excessive dietary potassium intake may contribute to hyperkalemia if urinary potassium excretion is simultaneously reduced. With normal kidney function, all potassium should be excreted.
Table 2: Foods High in Potassium
- Salt substitutes
- Figs
- Syrup
- Bran, cereals, wheat germ
- Vegetables (spinach, tomatoes, carrots, potatoes, broccoli, lima beans, cauliflower) and mushrooms
- Dried fruits, nuts, seeds
- Fruits (bananas, kiwi, oranges, mango, melon)
Hyperkalemia may be associated with blood transfusion - intravenous administration of blood cells, from which potassium is released into the extracellular space, with too rapid administration of calcium preparations to treat hypokalemia, with high potassium content during parenteral nutrition.
Hyperkalemia associated with the release of potassium from cells
Some exogenous and endogenous factors can disrupt the exchange of potassium between intercellular and intracellular fluids and increase the concentration of potassium in the serum. However, this mechanism rarely causes severe hyperkalemia unless the factor is, for example, tissue damage, necrosis (local tissue death as a result of injury), rhabdomyolysis, tumor breakdown, severe burns.
Table 3: reasons for potassium redistribution Redistribution of potassium between extracellular and intracellular fluids
- Muscle necrosis, myolysis (rhabdomyolysis - damage to skeletal muscles), tumor breakdown, severe burns
- Insulin deficiency (normally, this hormone accelerates the movement of potassium into cells)
- Metabolic acidosis
- Hyperosmolarity (hyperglycemia - increased blood glucose levels, administration of mannitol)
- Medicines (eg, succinylcholine (aka dithiline, listenone), beta blockers, digoxin)
- Hyperkalemic periodic paralysis (attacks most often develop 30-40 minutes after exercise)
Decreased potassium excretion
- Kidney damage (glomerular filtration <20 ml/min)
- Decreased mineralcorticoid activity
- Hyporeninemic form of hypoaldosteronism (chronic kidney disease, diabetic nephropathy, NSAIDs)
- Adrenal insufficiency (Addison's disease, congenital enzyme defect)
- Aldosterone blockers (see table 4)
- Immunity to aldosterone (sickle cell anemia, systemic lupus erythematosus, amyloidosis, obstructive nephropathy)
Decreased rate of urine filtration and sodium delivery to the distal nephron
- Hypovolemia
- Some genetic disorders, such as Gordon's syndrome
Hyperkalemia caused by impaired potassium excretion
Most potassium is excreted by the kidneys, so kidney damage is the main cause of hyperkalemia. Kidney damage accounts for up to 75% of cases of this condition.
In patients with chronic kidney disease, the ability to excrete potassium is maintained until renal failure develops (when filtration is reduced to less than 15-20 ml/ml) or when the patient consumes large amounts of potassium or takes drugs that increase potassium levels .
Damage to the juxtaglomerular apparatus leads to a deficiency in renin production (see RAAS), which causes hyponatremia and hypoaldosteronism, which can also cause hyperkalemia even in the absence of severe kidney damage. Hyporeninemic hypoaldosteronism is also known as type 4 tubular acidosis type 4, as it is often associated with mild to moderate metabolic acidosis, with a normal anion gap (the difference between cations and anions; Anion gap = (Na + K) - (Cl + [HCO3- ]) (units – mol/l)). Most often, this condition develops with diabetic nephropathy.
Hypoaldosteronism may also be a consequence of primary diseases of the adrenal glands (Addison's disease, congenital disorders of steroid synthesis, 21-hydroxylase deficiency) or a decrease in mineralcorticoid activity. The latter problem is often associated with sickle cell anemia, systemic lupus erythematosus, amyloidosis, obstructive nephropathy, and the use of potassium-sparing diuretics. In rare cases, a mutation of the mineralcorticoid receptor gene is detected.
In general, disturbances in mineralcorticoid metabolism do not cause hyperkalemia if normal amounts of sodium enter the distal nephron. Thus, patients with Addison's disease do not always develop hyperkalemia if they have adequate salt intake. Impaired urinary excretion or sodium delivery to the distal nephron plays an important role in the development of hyperkalemia. These disorders can be caused by internal factors or (more often) by certain medications (see tables 3, 4).
Drugs that cause hyperkalemia
Drugs can disrupt potassium homeostasis through several mechanisms: activation of transmembrane potassium transport, reduction in renal excretion (changes in the action of aldosterone, sodium delivery to the distal nephron, changes in the function of the collecting ducts). The risk increases when such drugs are taken by patients with kidney failure. Elderly patients and patients with diabetes are especially susceptible to developing hyperkalemia. In these groups, such drugs should be used with caution, starting with small doses and monitoring potassium levels whenever the dose is changed. There are no recommendations regarding the number of studies; the frequency of determining potassium levels depends on the level of renal failure, the presence of diabetes, medications taken, and concomitant diseases.
In particular, it is necessary to approach the management of patients with impaired electrical conductivity of the heart muscle very carefully, since even a slight increase in potassium levels can lead to arrhythmia.
The full list of medications is in the table.
Drugs that interfere with potassium transmembrane transport
- Beta blockers
- Digoxin
- Hyperosmolar solutions (mannitol, glucose)
- Suxamethonium (Listenon)
- Intravenous administration of positively charged amino acids
Substances containing potassium
- Potassium supplements
- Salt substitutes
- Herbal preparations (alfalfa, dandelion, horsetail, spurge, nettle)
- Red blood cells (when they break down, potassium is released)
Medicines that reduce aldosterone secretion
- ACE inhibitors
- Angiotensin II receptor blockers
- NSAIDs (NSAIDs)
- Heparin preparations
- Antifungal drugs (ketoconazole, fluconazole, intraconazole)
- Cyclosporins
- Prograph
Drugs that block the binding of aldosterone and mineralcorticoid receptors
- Spironolactone
- Inspra (Eplerenonum)
- Drospirenone
Drugs that inhibit potassium channel activity in epithelial cells
- Potassium-sparing diuretics (amiloride, triamterene)
- Trimethoprim (an antimicrobial drug)
- Pentamidine (antimicrobial)
Let's look at some of them:
Angiotensin converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are widely used to protect the kidneys and reduce mortality from heart disease, especially in diabetics. They are also included in standard treatment regimens for patients with chronic heart disease.
These drugs predispose to the development of hyperkalemia because they impair aldosterone secretion and reduce renal reperfusion (and glomerular filtration rate). Both drugs reduce urinary potassium excretion.
They do not cause hyperkalemia in patients with normal renal function; The degree of suppression of aldosterone secretion is not sufficient to significantly impair potassium excretion unless there is previous hypoaldosteronism (due to some disease or other medications). Unfortunately, people taking these drugs are at high risk of developing hyperkalemia. About 10% of outpatients develop hyperkalemia within a year of starting treatment with AFP inhibitors or angiotensin II receptor blockers.
Moreover, these drugs contribute to the development of hyperkalemia in 10-38% of patients admitted to hospitals. The risk is especially increased if the patient is taking high doses of drugs or in combination with other drugs that cause hyperkalemia.
Aldosterone (mineralocorticoid) receptor antagonists are also frequently used in the treatment of patients with congestive cardiac failure since the Randomized Aldactone Evaluation Study showed that the addition of spironolactone to treatment reduced morbidity and mortality. This study indicated that severe hyperkalemia developed in only 2% of patients when the creatinine concentration was 106 mmol/L and the spironolactone dose did not exceed 25 mg per day. In contrast, population based time-series analyzes demonstrate a significant increase in hospitalization and mortality from hyperkalemia. This is likely because the study included patients with severe renal impairment who were taking high doses of spironolactone. These patients were more likely than others in the study to take potassium supplements or other drugs that interfere with potassium excretion. The risk increases when spironolactone is combined with AFP inhibitors and ARBs, especially in elderly patients with impaired renal function.
Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit renin secretion (leading to hypoaldosteronism and decreased renal potassium excretion) and may impair renal function.
These drugs may be given judiciously in patients with diabetes or renal failure, especially if patients are taking other drugs (ACE inhibitors and ARBs). How is hyperkalemia diagnosed?
Hyperkalemia often occurs without symptoms and is detected during laboratory testing. When symptoms exist, they are not specific and are predominantly associated with disturbances in muscle function (paresthesia, muscle weakness, fatigue) or cardiac function (palpitations).
ECG: high “peaked” T wave, flattening or absence of P wave, widening of the QRS complex, sine waves.
However, ECG is not a sensitive method for diagnosing hyperkalemia. In a study by Acer et al, nearly half of patients with potassium levels above 6.5 mmol/L had no ECG changes. In addition, some patients experience a gradual change in cardiac function, while others experience a rapid progression from benign changes to fatal ventricular arrhythmias.
Evaluation of patients with hyperkalemia should include:
- Careful review of medical history to identify potential risk factors such as renal impairment, diabetes, adrenal insufficiency, use of medications that may cause hyperkalemia.
- Laboratory tests should be aimed at confirming the medical history and physical examination, and should include urea, creatinine, electrolytes, osmolarity (an acute increase in osmolarity can cause potassium to leak out of cells), and urine potassium concentration.
- In some patients, additional specific tests are performed, such as fractional sodium excretion or a transtubular potassium gradient may be used to distinguish between renal and nonrenal causes of hyperkalemia.
What to do with severe hyperkalemia?
Guidelines for the management of hyperkalemia are based on expert opinion due to a lack of clinical research. Treatment should be aimed at restoring electrolyte metabolism, preventing serious complications and treating the underlying disease. Figure In the management of mild to moderate hyperkalemia, loop diuretics are used to increase potassium excretion. Potassium intake from food should be limited. The dose of medications that increase potassium levels in the blood should be reduced or discontinued as much as possible. If the patient has impaired renal function, diuretics may not be effective. Then other measures are required, in particular dialysis.
Severe hyperkalemia is a life-threatening condition as it can cause serious disturbances of the heart and neuromuscular system, including cardiac arrest and paralysis of the respiratory muscles. Therefore, urgent and aggressive therapy is required. Many authors provide the following criteria for severe hyperkalemia: more than 6.0 mmol/l + changes on the ECG, or more than 6.5 mmol/l regardless of the presence of changes on the ECG.
If there are signs of hyperkalemia on the ECG or in the event of cardiac arrest in patients on dialysis, for example, therapy is started without laboratory data. Other factors that require proactive treatment: rapid rise in potassium levels, signs of acidosis, rapid deterioration of kidney function.
Most guidelines and experts advise that severe hyperkalemia should be treated in a hospital setting, which allows for continuous cardiac monitoring, since even patients without symptoms or ECG changes can develop life-threatening arrhythmias.
Although emergency dialysis removes potassium from the body, it is urgent to begin treatment of the underlying disease, as the 2005 Cochrane systematic review of emergency interventions for hyperkalaemia recommends doing three things :
- The first step is to stabilize myocardial activity and reduce the likelihood of arrhythmia. Intravenous calcium is used as a direct antagonist of potassium in influencing the membrane, stabilizing cardiac conduction. Calcium gluconate in a volume of 10 ml of a 10% solution is administered over 3-5 minutes under the control of the heart on a cardiac monitor. Calcium infusion has no effect on serum potassium levels, but does affect cardiac function: changes on the ECG are visible within 1-3 minutes after calcium administration, the effect lasts for 30-60 minutes. The infusion may be repeated if there is no effect within 5-10 minutes. Calcium should be used very carefully in patients taking digoxin, as calcium increases the toxic effects of digoxin.
- The second step is the transfer of potassium from extracellular fluid to intracellular fluid. This reduces serum potassium levels. This is achieved by administering insulin or beta-2 agonists, which stimulate the sodium-potassium pump. Insulin is administered intravenously as a bolus with sufficient glucose (to prevent hypoglycemia). The effect of insulin administration occurs after 20 minutes, reaches a maximum after 30-60 minutes, and lasts up to 6 hours. The most commonly used selective beta-2 agonist is salbutamol. Salbutamol is used using a nebulizer. The effect occurs after 20 minutes, the maximum effect is at 90-120 minutes. Salbutamol can be used alone or in combination with insulin. Sodium bicarbonate may also be prescribed to patients with acidosis, although the benefit of this drug for hyperkalemia remains controversial.
- Thirdly , measures are taken to remove potassium from the body. Potent loop diuretics (eg, 40 to 80 mg furosemide IV) increase renal potassium excretion by increasing urine production and sodium delivery to the distal nephron. But diuretics only work if kidney function is preserved, and many patients with hyperkalemia have acute or chronic kidney disease. Cation exchange resins, which remove potassium from the extracellular fluid in exchange for sodium through the intestine, are also widely used, although their effectiveness is controversial. They work faster as an enema than when administered orally. It may take 6 hours to achieve the effect. Dialysis is the definitive treatment for patients with severe hyperkalemia and progressive kidney disease.
Long-term management of hyperkalemia
After emergency treatment, measures should be taken to prevent recurrence of hyperkalemia.
The first step is to analyze the medications the patient is taking. If possible, reduce or eliminate medications that increase potassium levels. Because AFP inhibitors and angiotensin II receptor blockers slow the progression of chronic kidney disease, using other measures to control hyperkalemia or reducing the drug dose is preferable to stopping these drugs. It is wise to limit your potassium intake to 40-60 mmol per day. The use of diuretics may also be effective. Thiazide diuretics can be used in patients with preserved renal function, but they are usually ineffective if the glomerular filtration rate is less than 40 ml/min, when loop diuretics are more preferable. Fludrocortisone may be used in patients with hyporeninemic hypoaldosteronism. However, this drug should be used with caution, especially in patients with type 2 diabetes, which often occurs with hypertension, as the drug leads to fluid retention and increased blood pressure. Tips for non-experts
- In patients without a predisposition to hyperkalemia, repeat the potassium test to rule out pseudohyperkalemia.
- Don't forget about possible hidden causes of hyperkalemia, including NSAIDs
- ACE inhibitors and angiotensin II receptor blockers should be started at low doses, and potassium levels should be monitored one week after starting treatment and after dose increases.
- All patients with hyperkalemia should undergo a 12-lead ECG.
- ECG changes and arrhythmias associated with hyperkalemia require urgent medical attention.
Questions for current and future researchers
- How important is the contribution of various risk factors to the development of hyperkalemia and how to evaluate them?
- With the increasing use of cardio- and renoprotectors that promote potassium retention, which method is most preferable for monitoring potassium levels?
Improved understanding of the molecular mechanisms underlying the maintenance of extracellular fluid potassium levels, developing new therapeutic strategies for the treatment of life-threatening hyperkalemia.
| Spironolactone – a potassium-sparing diuretic, a competitive antagonist of aldosterone in its effect on the distal nephron. Increases the excretion of Na+, Cl- and water and reduces the excretion of K+ and urea. Trade names: Veroshpiron, Spironolactone. Contraindications: Addison's disease, hyperkalemia, hypercalcemia, hyponatremia, chronic renal failure, anuria, liver failure, diabetes mellitus with confirmed or suspected chronic renal failure, diabetic nephropathy, first trimester of pregnancy, metabolic acidosis, menstrual irregularities or breast enlargement, hypersensitivity to spironolactone. More details on the website vidal.ru: | Exogenous – literally translated, formed from the outside. In medicine it is used in relation to the body and means that a certain factor is formed and comes from the outside. For example, exogenous factors are food. Endogenous is the opposite term, meaning that a certain factor is formed inside the body. |
RAAS – renin-angiotensin-aldosterone system. When the pressure in the kidneys decreases (bleeding, fluid loss, decreased sodium chloride concentration), an enzyme is produced in the juxtaglomerular cells of the kidneys renin. The substrate of this enzyme (the substance on which the enzyme acts) is angiotensinogen. Under the influence of renin, angiotensinogen is converted into angiotensin I. Angiotensin II is formed from angiotensin II under the action of angiotensin-converting enzyme (ACE) and has the following actions:
Hereditary predisposition to severe vascular spasm, including those associated with ACE, is determined using the block of analyzes “Polymorphism of vascular tone genes.” | ECG - electrocardiography - a study based on recording the electric fields generated during the work of the heart using a special device - an electrocardiograph. The ECG is recorded using special electrodes placed on certain areas of the body. ECG is a common method for assessing heart function. ECG analysis, ABC ECG analysis, practice: https://www.practica.ru/BK1/5.htm |
| Acidosis (from Latin acidus - sour) is a change in the acid-base state associated with increased acidity (increased hydrogen ions). Acidosis is said to occur when arterial blood pH falls below 7.35. Contrasted with alkalosis, when the pH is greater than 7.45. Metabolic acidosis is associated with metabolic disorders (excessive formation of acids, insufficient excretion, loss of bases). Respiratory (respiratory) acidosis develops when pulmonary ventilation is impaired (respiratory failure or circulatory failure in the lungs). | Geodialysis (dialysis) is a method of extrarenal blood purification in case of renal failure. Hemodialysis is carried out using an artificial kidney machine. |
| Homeostasis - in physiology - the ability of a self-regulating system to maintain a constant internal state through coordinated reactions aimed at maintaining dynamic constancy. The term was proposed by the American physiologist W. Cannon in 1929. Examples of homeostasis are maintaining blood pH, body temperature, pressure, and so on. | Parenteral nutrition is the administration of nutrients (carbohydrates, amino acids, lipids, salts, vitamins) intravenously when natural food intake is not possible. |
| Gordon's syndrome is a rare disease associated with increased chloride reabsorption in the distal nephron. Characterized by the presence of hyperkalemia, metabolic acidosis, hyporeninemia, hypoaldosteronemia, decreased sensitivity of the kidneys to mineralcorticoids. | |
| Mineralcorticoids are a group of corticosteroid hormones of the adrenal cortex that affect water-salt metabolism (aldosterone, deoxycorticosterone). | |
| The juxtaglomerular apparatus of the kidneys (JRA) is a collection of renal tissue cells that form and secrete biologically active substances, including renin. |
Tags:
hyperkalemia, potassium, electrolytes
Back to section
What does excess magnesium and potassium lead to?
It is very important that a person takes magnesium- and potassium-containing drugs strictly according to indications and in the dosage prescribed by the doctor. You cannot choose a medicine by reading information about it or listening to the recommendations of a pharmacist. The most important thing is to never listen to harmful advice that large doses of such drugs can “strengthen the heart” and “improve blood vessels.”
Excess potassium
The maximum dose of potassium per day is 6 g. If a person consumes 14 g, his heart may stop. An initial excess of this mineral is possible if a person has:
- type 2 diabetes mellitus
- chronic renal failure ;
- extensive injuries with crushing tissue;
- consequences of exposure to radiation or the use of cytostatics.
If you consume high doses of this microelement over a long period of time, the consequence may be:
- heart rhythm disturbances;
- muscle weakness;
- anxiety, irritability;
- nausea, intestinal colic, vomiting, diarrhea ;
- diabetes;
- frequent urination.
Excess magnesium
The maximum daily dose of magnesium is 800 mg per day. An overdose is not fatal, but if it occurs, the following effects may occur:
- stones in the kidneys;
- chronic fatigue;
- psoriasis;
- hyperthyroidism.
Excessive magnesium retention is observed if a person suffers from chronic renal failure.
How much calcium should be added
Remember that you usually only need 1000-1200 mg of calcium each day. There is no point in getting more calcium. It might even be dangerous. There are recommendations that the maximum daily calcium intake should not be more than 2000-2500 mg per day. To avoid the danger of getting too much calcium and causing constipation, hypercalcemia, calcium accumulation in soft tissues, problems with the absorption of iron and zinc, it is not recommended to receive more than 1400 mg of calcium per day for a long time.
If you cannot supplement your diet with foods high in calcium (dairy products, leafy greens, nuts, beans and tofu), you can take up to 500-1000 mg of elemental calcium from supplements.
Potassium and magnesium preparations for the heart and blood vessels
In modern pharmacology, potassium and magnesium tablets are offered in different versions, and their prices also vary. Potassium and magnesium preparations in tablets of varying prices are described below.
Panangin
This is an inexpensive remedy with potassium and magnesium, which many take as a medicine “for the heart.” After all, very often magnesium and potassium for the heart are taken for any problems with this organ, believing that this will help “support” the heart.
However, drugs with these components are not as harmless as many people think.
The main indication for the use of Panangin is the replacement of potassium losses when using diuretic drugs for the treatment of chronic heart failure or diuretics that do not conserve potassium. It is advisable to take Panangin when treating with Torasemide , Furosemide , Diacarb , etc.
If the patient is prescribed to take potassium-sparing diuretics, such as Amiloride , Triamterene , Veroshpiron , Triampur , etc., there is no need to use an additional product with this microelement. There is no need to take potassium-containing medications when taking Indapamide and Hypothiazide .
Panangin normalizes heart rhythm during ventricular arrhythmias . In the treatment of atrial fibrillation and paroxysmal tachycardia , it is usually used as an adjuvant. Along with antiarrhythmic drugs, Panangin is prescribed for atrial rhythm disturbances.
For the purpose of prevention, this drug is prescribed to elderly people who often have repeated attacks of paroxysmal tachycardia, extrasystole, and at the same time the level of potassium in the blood is very low. It is also advisable to take this medicine for unstable arterial hypertension or frequent attacks of angina .
Panangin reduces the severity of side effects when using cardiac glycosides and improves the tolerability of such drugs.
Panangin is contraindicated: for myasthenia gravis , acidosis , cardiogenic shock with low blood pressure, atrioventricular blockade, dehydration, hemolysis , metabolic disorders of magnesium and potassium. Nursing mothers and pregnant women should take it with caution.
When taking Panangin simultaneously with ACE inhibitors, beta-blockers, NSAIDs, cyclosporines, the risk of potassium overdose increases.
Cost – from 300 rubles. per pack 60 pcs.
Asparkam
The composition is similar to Panangin. Asparkam tablets have similar contraindications and side effects. The cost of the drug is from 50 rubles. for 20 pcs.
Also analogues of the drug Panangin are Pamaton , Asparkam , Potassium-magnesium aspartate - tablets and solution for infusion. If the body needs potassium or magnesium, a dropper is placed with this drug.
Orocamage
These are capsules of potassium and magnesium orotate. Orocamag is used as part of complex treatment of supraventricular extrasystole and unstable angina . Contraindications and side effects are the same as for Panangin. Orocamag is not prescribed to expectant mothers or nursing mothers.
ELECTROPHYSIOLOGICAL EFFECTS OF HYPOKALEMIA
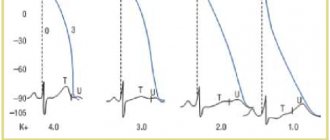
Hypokalemia leads to an increase (more electronegative value) of the membrane PP and, at least during electrical diastole, reduces membrane excitability due to an increase in the difference between the PP and the threshold potential. It is assumed that extracellular potassium is necessary for the opening of delayed rectifying current channels [31]. Low extracellular potassium levels reduce the delayed (outward) potassium current, leading to increased AP duration and slower repolarization. The most important here is the disruption of the AP configuration, especially the slowing down of the “slope” of the 3rd phase of repolarization. An AP with a long “tail” is formed, which leads to an increase in the relative refractory period (RPP) and a decrease in the difference between the AP and the threshold potential in the final phase of the AP. Therefore, the myocardium exhibits increased excitability and an associated tendency to ectopic activity during a significant portion of the AP. Conduction slows as depolarization begins in incompletely repolarized fibers. Moreover, hypokalemia lengthens the plateau phase in Purkinje fibers, but shortens it in ventricular fibers [10]. The repolarization phase (“tail”) of AP in the conduction system is prolonged more than in the ventricles, which increases the spread of repolarization. Hypokalemia accelerates diastolic depolarization in Purkinje fibers, thereby increasing automaticity. In total, the electrophysiological effects of hypokalemia are manifested in a decrease in conduction velocity, shortening of the effective refractory period (ERP), prolongation of the ORP, increased automaticity and early afterdepolarization.
ECG manifestations of hypokalemia:
- due to changes in repolarization:
– decrease in amplitude and expansion of the T wave; – noticeable wave U; – reduction of the ST segment; – fusion of T and U waves (with severe hypokalemia);
- due to conduction disorders:
– increase in the duration of the QRS complex; – atrioventricular block; – increase in amplitude and expansion of the P wave; – slight increase in the P–R interval; - cardiac arrest.
When the U wave exceeds the T wave in amplitude, the plasma potassium level is <3 mmol/L (see figure).
Magnesium preparations
Magnerot
These 500 mg tablets contain magnesium orotate dihydrate . Magnerot is used for a deficiency of magnesium in the body, for arrhythmia associated with such a deficiency, as well as in the treatment of atherosclerosis , endarteritis , chronic heart failure, muscle spasms, myocardial infarction , and metabolic disorders of fats.
Negative effects may include allergic reactions, nausea, diarrhea , and appetite disturbances. Expectant mothers and women during lactation can use the product if they have a normal level of magnesium in their blood.
Contraindicated for use in people with urolithiasis, liver cirrhosis , renal failure, lactase deficiency, and impaired glucose absorption.
Cost – from 330 rubles. for 20 pcs.
Doppelhertz Active
Dietary supplement that combines two microelements. Indications for the use of Doppelhertz Active magnesium + potassium are the same as for the use of Magnerot.
Cost – from 360 rubles. for 30 tab.
Composition and release form
5 ml (1 teaspoon) of syrup contains vitamin B1 4 mg (thiamine 5 mg), vitamin B2 1 mg (riboflavin 1.32 mg), vitamin B6 (pyridoxine hydrochloride) 2 mg, vitamin B12 5 mcg, niacin (nicotinamide, vitamin B3) 8 mg, folic acid 150 mcg, vitamin C (ascorbic acid) 10 mg, pantothenic acid 2 mg, calcium glycerophosphate 10 mg, iron 7 mg (iron ammonium citrate 35 mg), zinc (sulfate) 5 mg, manganese 0 .25 mg (manganese sulfate 21.99 mg), copper 0.25 mg (copper sulfate 0.91 mg), iodine 40 mcg (potassium iodide 52.32 mcg), lysine hydrochloride 40 mg, honey 100 mg, malt extract 500 mg; in dark glass bottles of 200 ml, 1 bottle in a box.
Medicines for seizures
Potassium and magnesium preparations are used for seizures . The manifestation of convulsions, tingling sensations, and “goosebumps” appear as a consequence of impaired neuromuscular transmission. Sometimes such manifestations are the consequences of a lack of magnesium in the body. A person becomes worse due to a lack of B vitamins , since this microelement is directly involved in their synthesis.
The development of muscle cramps occurs in the following cases:
- during dehydration;
- during treatment with laxatives or diuretics;
- with electrolyte disturbances due to diarrhea and vomiting;
- due to frequent bowel cleansing with an enema;
- during fasting.
Most often, cramps bother older people at night. During this period, involuntary twitching and numbness of one or both legs suddenly begin. This unpleasant phenomenon not only disrupts sleep, but also causes very unpleasant sensations. Most often this happens due to the following reasons:
- poisoning with aluminum, lead, cadmium, manganese, nickel, cobalt, beryllium;
- alcohol abuse;
- diabetes;
- resection of the small intestine, malabsorption in the small intestine;
- taking antitumor drugs, Gentamicin .
It is possible that spasms may occur not only in the limbs, but also in different muscle groups. Such manifestations are not uncommon during pregnancy, as well as in children - during the period when the child is actively growing.
Proper treatment, which includes medications with magnesium and vitamin B6 .
Magne B6
This is magnesium in tablets and in the form of a solution for oral use. The product contains magnesium lactate dihydrate (corresponding to 48 mg of divalent magnesium) and pyridoxine hydrochloride (B6).
Magne B6 is used for muscle spasms, a lack of this microelement, heart rhythm disturbances, spasms in the gastrointestinal tract, high excitability and irritability, and sleep problems.
How to take magnesium with B6 is indicated in the instructions. It is prescribed in courses, each of which lasts at least 4 weeks. You need to take 6-8 tablets per day in 3-4 doses. Both the solution and the tablets should be taken with food, washed down with liquid.
People with renal failure , fructose intolerance, and impaired absorption of sucrose and glucose should not be treated with Magne B6 Not prescribed to children under 6 years of age. The active components penetrate the placenta and are detected in milk, so it is not recommended for pregnant and lactating women to take the product.
You cannot combine its use with treatment with Levodopa .
Possible negative effects: vomiting, nausea, flatulence , diarrhea .
Poisoning with the drug is possible only if the glomerular filtration rate of the kidneys decreases significantly. The consequences of poisoning are: a significant drop in blood pressure, depression, vomiting, diarrhea, respiratory depression, and irregular heartbeat.
Magnesium B6 costs in tablets depends on the manufacturer and the drug. Price Magnesium B6 in tablets – from 580 rub. for 30 pcs., in ampoules - from 530 rubles. for 10 pcs. There are also a number of analogues of the drug Magne B6. These medications are Magnesium B6 forte , Magne Express Sachet , Systematic Magnesium+B6 , Magnelis B6 .
Magnistad
These are vitamins with magnesium, which include magnesium lactate dihydrate (470 mg) and pyridoxine hydrochloride (5 mg). These magnesium-containing vitamins are maximally absorbed due to the presence of a coating that dissolves in the intestines.
All negative effects, indications and contraindications are similar to the same points in the instructions for Magna B6.
The cost of Magnistad is from 325 rubles. for 50 pcs.
Vitamins with potassium and magnesium
In every pharmacy on the shelves you can see numerous names of vitamins with magnesium and potassium. Vitamins, which also contain microelements, are widely produced and used for various conditions and diseases.
Popular products are Makrovit , Duovit , Vitrum , Teravit , Complivit , etc. They contain not only potassium, magnesium and potassium in the tablets, but also other microelements and vitamins necessary for the human body.
What tests to take
It is difficult to detect calcium deficiency using a blood test, because the body does everything possible to maintain a constant level of ionized calcium in the blood. But it’s easy to be deficient or deficient in vitamin D by taking a blood test for 25-OH vitamin D.
To identify contraindications and evaluate the effectiveness of treatment with calcium preparations, you should take tests:
- Calcium and phosphorus in the blood
- Calcium in daily urine
- Blood creatinine
- 25-OH vitamin D
In the Lab4U laboratory this can be done with a discount of up to 50%.
Other drugs
Magnesia (Magnesium sulfate)
A medicine with an antihypertensive effect that effectively reduces the swelling of the vascular walls, which leads to a decrease in blood pressure. For a long time, magnesia was used as a medicine to relieve hypertensive crises. It was also used for this purpose for expectant mothers.
Currently, magnesia is primarily used as a medicine that effectively reduces intracranial pressure . To do this, it is administered intramuscularly.
Magnesia powder is a laxative that stimulates the passage of bile . As a result, bile acids have a laxative effect. At one time, many people practiced so-called liver tubages . This procedure consisted of the following: it was necessary to take magnesium sulfate and lie on the right side, placing a heating pad under it to increase the passage of bile. Currently, such actions are no longer practiced, since the effect of ursodeoxycholic acid in this case is more pronounced.
Magnesia is used intravenously during pregnancy to reduce edema, as well as to reduce the tone of the uterus.
In addition, drugs with magnesium and potassium are included in polarizing mixtures, which modern anesthesiologists do not consider seriously.
How many microelements are contained in foods?
To eliminate the deficiency of these elements, you should include foods rich in potassium and magnesium in your diet. For your heart, it is recommended to eat some foods containing potassium and magnesium.
You can find out which foods contain magnesium and potassium from the table below. The list of foods containing a lot of these microelements is quite wide. And everyone can choose the optimal source of these elements for themselves. But provided that the nutrition is complete and absorption occurs normally, a deficiency of these elements should not develop.
The table of foods containing potassium and magnesium informs you which foods contain the maximum amount. Indicators are given in mg per 100 g of product. So, what contains the maximum of these elements?
| Product | Potassium amount | Amount of magnesium |
| watermelon | 175 | 25 |
| avocado | 440 | 125 |
| apricots | 340 | 20 |
| oranges | 160 | 13 |
| bananas | 390 | 40 |
| grape | 215 | 18 |
| cherry | 290 | 27 |
| peach | 150 | 15 |
| apple | 108 | 9 |
| nuts | 750 | 160 |
| beans | 1020 | 130 |
| broccoli, cauliflower | 360 | 18 |
| potato | 470 | 24 |
| carrot | 310 | 38 |
| milk | 140 | 12 |
| cheese | 100 | 46 |
| eggs | 140 | 12 |
| herring | 90 | 160 |
| meat – pork, beef | 100 | 28 |
| buckwheat | 380 | 78 |
| wheat bran | 1150 | 570 |
| oatmeal | 350 | 133 |
| rice | 100 | 30 |
| raisin | 1020 | 60 |
| dried apricots | 1876 | 50 |
| coffee | 1750 | 1 |
| tea | 2367 | — |
| cocoa | 1660 | 170 |
conclusions
Preparations containing these two microelements are of great auxiliary value in the treatment of various diseases. But, above all, they are important as a means of replacement treatment for a lack of magnesium and potassium in the body.
It is a mistake to believe that such drugs are drugs for the heart, and these drugs cannot be taken uncontrolled. Any list of heart pills should be prescribed by a doctor after a comprehensive study, and heart vitamins in tablets are an auxiliary product that is also taken as prescribed by a doctor as part of a comprehensive treatment.
When to think about calcium deficiency
If you have a lack or deficiency of vitamin D, if you don’t get enough sun exposure, drink little or no milk and dairy products, for example due to an allergy or lactose intolerance, follow special types of diet (high protein diet, veganism, etc.) .), if you are addicted to caffeine (coffee, strong tea, chocolate), then you should think about the lack of calcium intake from food. By the way, foods such as spinach, greens, rhubarb, and beans, although rich in calcium, also contain oxalic and phytic acids. As a result, insoluble calcium-oxalate and calcium-phytate complexes are formed, which does not allow calcium to be absorbed.
Diseases of the kidneys, parathyroid glands and inflammatory bowel diseases also disrupt the calcium balance in the body.