Heartburn is an unpleasant symptom that you want to get rid of quickly. After all, eating and feeling full should bring pleasure and relaxation, not torment. Let's find out what medications can help with heartburn.
Heartburn occurs when acidic stomach contents enter the esophagus. The esophageal mucosa is not adapted to such an environment and an unpleasant burning sensation occurs. In the course of life, this condition can happen to anyone through overeating, bending over after eating, or in women during pregnancy. With prolonged symptoms, the esophagus may suffer, erosions, ulcers may develop, and scar tissue may form, which will lead to a narrowing of the lumen. Cell degeneration and the development of neoplasms may occur.
Causes of heartburn
The most common cause of heartburn is gastroesophageal reflux disease (GERD). It occurs in 83% of patients with this problem. In addition to heartburn, symptoms such as:
- regurgitation, esophageal vomiting, belching;
- salivation;
- pain when swallowing food;
- difficulty passing food;
- hoarseness of voice;
- nasal congestion;
- coughing;
- glossitis;
- interruptions in heart function.
In addition to gastroesophageal reflux disease, heartburn may be closely associated with:
- Peptic ulcer of the stomach and duodenum.
- Stomach cancer.
- Functional dyspepsia (a group of diseases that do not lead to changes in the structure of the digestive organs, but cause disturbances in their functions).
Many medications have the property of reducing the tone of the lower esophageal sphincter, which can lead to reflux of contents into the esophagus or themselves cause inflammation. Hormonal, antihypertensive, and anti-inflammatory drugs may have such side effects. Therefore, you need to read the instructions carefully.
Many medications can cause heartburn.
The cause of heartburn can be increased intra-abdominal pressure and conditions leading to this:
- pregnancy;
- ascites;
- flatulence;
- hepato-splenomegaly;
- constipation;
- chronic obstructive pulmonary disease, etc.
Without treating the underlying disease, taking heartburn medications will not only not help in the future, but will also mask the symptoms of the underlying problem.
Pain due to coronary heart disease can be confused with heartburn.
The role of histamine in allergic reactions
Histamine is a biologically active substance produced by the body to regulate vital functions (blood circulation, respiration, digestion). It is concentrated in mast cells, white blood cells that are part of the immune system.
Under normal conditions, there is little histamine in the human body and it is inactive. But when certain substances enter the body, their active production begins. When the allergen binds to immunoglobulin, mast cells degranulate (release substances that cause an inflammatory response). Histamine is released, leaves the cells, and the body comes under its influence. It causes:
- hives;
- swelling of the mucous membranes;
- bronchospasms;
- decreased blood pressure;
- digestive disorders;
- confusion;
- slowing down the conduction of nerve impulses.
The first three reactions are allergic. They are the immune system's response to contact with an irritant. Most allergic reactions develop immediately.
Heartburn medications
If heartburn does not bother you often, once a week or less, you can take antacids and alginates .
Antacids
This group of drugs neutralizes hydrochloric acid produced by the cells of the gastric mucosa. Reducing acidity in the stomach helps to increase the tone of the lower esophageal sphincter.
Modern combination drugs that additionally have an enveloping and sometimes calming effect include:
- Phosphalugel;
- Almagel A;
- Gastal;
- Maalox;
- Relzer.
The main thing is that these medications do not have rebound syndrome, like regular soda. When using it, the acidity first decreases, and after a few hours it increases again.
Alginates
- Gaviscon;
- Gaviscon Double Action.
Preparations from the alginate group form a gel film on the surface, which protects the mucous membrane from the action of acid and pepsin. Some drugs have a double effect, since they contain an antacid component.
H2-histamine receptor blockers
- Ranitidine;
- Famotidine;
- Nizatidine.
They reduce the production of hydrochloric acid by the parietal cells of the stomach. The advantage of their action is that the secretion associated with food intake is suppressed to a lesser extent, which means the digestive processes will be affected to a lesser extent. At the first symptoms of heartburn, it is possible to take halved doses of H2-histamine receptor blockers. The effect can last up to 12 hours, and there is no need for additional antacid medications.
H2-histamine receptor blockers reduce the production of hydrochloric acid by the parietal cells of the stomach.
Proton pump inhibitors (PPIs)
- Nexium;
- Nolpaza;
- Pariet;
- Omez.
Proton pump inhibitors inhibit the final stage of hydrochloric acid formation in the parietal cells of the stomach. The maximum effect of administration develops on days 5-7 of administration. The secretion of hydrochloric acid is restored on the 2nd day after stopping the intake. With prolonged use of drugs for several years and a severe lack of hydrochloric acid in the stomach, pathogenic flora can develop. Drugs in this group do not have an immediate effect and can only be prescribed by a doctor after diagnosis.
Prokinetics
- Ganaton;
- Motilium;
- Motilak.
If the symptoms of heartburn go along with impaired motor function of the stomach, the organ is sensitive to stretching, prokinetics help accelerate the evacuation of food into the small intestine. The propulsive motility of the stomach increases.
UDCA preparations
- Ursosan.
Sometimes not only the contents of the stomach, but also the contents of the small intestine, such as bile, are thrown into the esophagus. This situation can arise in case of liver diseases, when drugs that reduce acidity in the stomach have already been used, there is no reflux of the acidic part, but there is irritation and heartburn in the esophagus. In this case, ursodeoxychoic acid (UDCA) preparations are recommended. They help the liver restore its function, normalize the formation and flow of bile, and can reduce the symptoms of heartburn. The course of application is from 2 weeks to 6 months.
Antihistamines (AGDs), as their name suggests, are a group of drugs that weaken the effects of histamine by blocking histamine receptors (HR) in the body.
Histamine is one of the most important mediators involved in the regulation of vital functions of the body and plays an important role in the pathogenesis of various diseases.
Histamine (β-imidazolyl-4(5)-ethylamine) belongs to the group of biogenic amines and has pronounced biological activity (see figure)
.
Figure 1. Histamine formation.
Histamine is released during inflammatory and allergic reactions, anaphylactic and anaphylactoid shock, pseudoallergic reactions and other conditions. The main depot of histamine is peripheral blood basophils and tissue basophils, or mast cells (MCs). In humans, the highest histamine content is observed in mast cells in the lungs and skin (up to 1·106/g tissue).
In various diseases and conditions (infection, allergic diseases - AD, trauma, stress, etc.) there is an increase in the content of histamine and other biologically active substances - biologically active substances (serotonin, bradykinin, acetylcholine, prostaglandins, etc.).
The histamine content also increases with the consumption of certain foods (seafood, strawberries, egg whites, etc.), and the administration of drugs (anticholinergics, local anesthetics, some analgesics, antibiotics, etc.).
There are specific receptors in the body, the so-called histamine or H receptors (H1, H2, H3, H4), to which histamine binds.
The release of histamine from cells can be caused by immunological (specific) and non-immunological (non-specific) mechanisms.
The immunological mechanism underlies allergic reactions and consists in the interaction of allergen-specific IgE, fixed on basophils and MCs, with antigen (AG), which leads to their degranulation and the release of histamine. The released histamine inhibits further histamine secretion by a feedback principle [1, 2].
One of the main regulators of this process is cyclic guanosine monophosphate. Substances that increase its content (methylxanthines, catecholamines, some bacterial toxins) inhibit the process of histamine release from the cell.
Histamine has a significant influence on the development of symptoms in both the early and late phases of an allergic reaction. Acting through type 1 GH (H1), histamine causes contraction of smooth muscles, especially the bronchi and intestines, vasodilation and increased permeability, hypersecretion of mucus in the upper respiratory tract; decreased blood pressure (BP), the appearance of angioedema and itching.
Histamine leads to an increase in the intracellular concentration of cGMP, increased chemotaxis of eosinophils and neutrophils, increased production of PgE2, thromboxane B, suppression of the synthesis of lymphokines, etc. At the same time, the content of histamine in the blood and the hypersensitivity of effector organ cells to it increase.
The non-immunological mechanism is observed more often and consists of the action on MCs of substances that have the ability to cause nonspecific release of histamine from these cells without specific IgE.
The effects of histamine can be blocked in various ways: by inhibiting its biosynthesis; strengthening its neutralization; blocking histamine access to receptors; inhibition of histamine release from mast cells.
All agents affecting GH are divided into 2 main groups:
1) stimulants of H1 and H2 receptors, or histaminomimetics;
2) H1- and H2-receptor blockers, antihistamines.
Histaminomimetics stimulate H1 and H2 receptors, causing spasm of smooth muscles, dilation of capillaries, decreased blood pressure, increased heart rate, increased secretion of gastric juice, etc. Previously, these drugs were used in the clinic for the treatment of polyarthritis, rheumatism, damage to peripheral nerves, etc. Now for More effective, pathogenetically based means are used to treat these diseases.
Currently, more than 150 drugs of various origins, chemical structures and mechanisms of action are known that can inhibit the release of histamine.
There are 2 subgroups among AGPs:
1) direct action (H1 and H2 receptor blockers);
2) indirect action (cromolyn, INN - acidum cromoglycicum, nedocromil sodium, ketotifen - ketotiphenum, histaglobulin - histaglobulinum, etc.), the effect of which is realized when they are administered through a mediator, synthesis or release of biologically active substances caused by the influence of these drugs.
The antiallergic effect of the indirect action antihistamines cromolyn (sodium cromoglycate) and nedocromil sodium is due to their ability to inhibit the release of mediators from allergy target cells (TCs). Sodium cromoglycate acts through a receptor mechanism. The drug does not penetrate cells, is not metabolized and is excreted unchanged in urine and bile. Cromolyn is slowly absorbed and remains on the mucous membrane for a long time, providing long-lasting action and an extremely low incidence of undesirable effects.
Nedocromil sodium, like sodium cromoglycate, is a lipophobic, highly polar compound found in a concentrated state. It has high therapeutic efficacy in patients with mild to moderate severity of bronchial asthma (BA), allergic rhinitis (AR), allergic conjunctivitis; it has virtually no side effects.
The use of AGPs, H1 receptor blockers, in the clinic is due to the role of histamine in the pathogenesis of various inflammatory reactions.
First of all, histamine is an obligatory participant in almost all clinical manifestations of allergies, so antihistamines will remain the most widely used and sought-after antiallergic drugs.
In addition, the pharmacological effect of AGP is not limited to the known antihistamine properties, but is represented by a wider spectrum of anti-inflammatory activity. The anti-inflammatory effect of histamine is associated with a decrease in the activity of transcription factors involved in the synthesis of anti-inflammatory mediators, which lead to a decrease in the expression of adhesion molecules, accumulation and activation of eosinophils, neutrophils, lymphocytes and other cells involved in the development of inflammation and the production of cytokines by epithelial cells [1, 3, 4].
The established additional antiallergic properties of antihistamines [5, 6] motivated the creation of new classes of drugs with multifunctional action, combining H1-antihistamine activity and the ability to inhibit the activation of allergy target cells and, accordingly, the formation and secretion of proallergic molecular mediators.
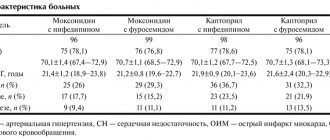
In modern clinics, “classical” or sedative first-generation antihypertensive drugs are used (Table 1)
and modern (non-sedating) second-generation antihypertensive drugs.
During the use of first-generation antihistamines, side effects were identified (sedation, antiserotonin activity, adrenolytic effect, etc.) even more pronounced than the therapeutic effect, and the antihistamine effect is often short-lived (4-12 hours), which dictates the need for their repeated administration 2- 4 times a day. The duration of side effects for first-generation antihypertensive drugs is 7 hours for diphenhydramine (diphenhydramine), and up to 6 hours for clemastine (tavegil).
Nevertheless, this group of drugs has its own niche, its own contingent of patients who are indicated for the use of first-generation antihypertensive drugs, in particular, if parenteral administration is necessary and in people with increased excitability.
First generation antihypertensive drugs are used primarily to relieve the following acute allergic reactions:
- acute allergic urticaria;
- anaphylactic or anaphylactoid shock;
- acute angioedema (parenterally, as an additional remedy);
- acute allergic and pseudoallergic reactions caused by drugs;
- acute allergic reactions to food products;
- serum sickness.
Modern second-generation AGPs differ in their chemical structure, mechanisms of action and are devoid of side effects characteristic of first-generation AGPs (Table 2)
.
Most second-generation H1 GR antagonists bind to H1 receptors noncompetitively. Such compounds are difficult to displace from the H1 receptor, and the resulting ligand-receptor complex dissociates relatively slowly, which explains the longer action of such drugs.
Unlike first-generation antihypertensive drugs, second-generation drugs have higher specificity and higher affinity for H1 receptors, have a longer therapeutic effect (up to 24 hours), do not penetrate the blood-brain barrier in therapeutic doses, do not affect other receptors, and do not cause tachyphylaxis [7].
The second generation AGP does not have a connection between absorption and food intake.
In clinical practice, the main indications for prescribing second-generation antihypertensive drugs are the following ADs and conditions:
— AR persistent (year-round) and seasonal;
- hay fever;
— allergic dermatoses with severe itching (acute and chronic urticaria, atopic dermatitis, etc.);
- year-round or seasonal allergic conjunctivitis;
- allergic contact dermatitis;
— prevention of complications during allergen-specific immunotherapy;
— allergic reactions during vaccination;
- other histamine-dependent allergic and pseudoallergic reactions.
Particularly noteworthy is the group of antihypertensive drugs, which are represented by quinuclidine derivatives: hifenadine (fencarol) and sehifenadine (histafen), created in the laboratory of academician M.D. Mashkovsky in the late 70s - early 80s of the twentieth century.
Historically, quinuclidines in the modern classification are classified as first-generation AGPs. This is due to the fact that during the creation of quinuclidines there was no classification of AGPs. It can be considered that hifenadine (fencarol) and sehifenadine (histafen) are one of the first examples of the creation of a new class of antihypertensive drugs with multifunctional action, combining high selective activity to block GR H1, the ability to block serotonin and destroy histamine directly in tissues due to the activation of the enzyme diamine oxidase ( histaminase), which enhances their antihistamine effect.
Due to their low lipophilicity, quinuclidines poorly penetrate the blood-brain barrier and do not cause pronounced sedative effects, as demonstrated in clinical studies conducted in patients with AR and chronic recurrent urticaria [8, 9].
Fenkarol and histafen belong to quinuclidine derivatives, however, the presence of 2 methyl groups in the structure of the molecule of the active substance sehifenadine changes its spatial structure, enhancing the antiserotonin effect of histafen, which is clinically manifested in a more pronounced antipruritic effect.
AGPs—quinuclidine derivatives—provide a pronounced clinical effect even with long-term use, are characterized by high safety, and do not have atropine-like or cholinergic effects, which makes it possible to compare quinuclidines with second-generation AGPs.
Thus, quinuclidine derivatives (fenkarol and histafen) uniquely combine the advantages of first-generation antihypertensives and modern second-generation antihypertensives, and also block not only the mediator histamine, but also serotonin. Quinuclidine derivatives, unlike other antihypertensive drugs, have antiarrhythmic activity, which is due to the presence of a quinuclidine core in its molecule, since the antiarrhythmic effect is also characteristic of other quinuclidine derivatives (for example, oxylidine).
Another area of application for sehifenadine (histafen) is gerontology. Older people often suffer from chronic recurrent urticaria and itching (senile pruritus). Affordable price, strong antipruritic effect, and lack of cardiotoxicity determine the possibility of widespread use of histaphen in gerontology.
In pediatric practice, hifenadine (fencarol) has proven itself to be an effective antihistamine with high safety. In addition, quinuclidines can be combined with other groups of drugs (antibiotics, antifungals, cardiotonic drugs, etc.).
In clinical practice, the main indications for prescribing quinuclidines, as well as modern second-generation antihypertensive drugs, are:
— AR persistent (year-round) and seasonal;
- hay fever;
— allergic dermatoses with severe itching (acute and chronic urticaria, atopic dermatitis, etc.);
- year-round or seasonal allergic conjunctivitis;
— atopic form of asthma in combination with AR, conjunctivitis or atopic dermatitis;
- allergic reactions to insect bites or stings;
- drug and food allergies;
- pseudo-allergic reactions to various groups of allergens, foods and medications;
— prevention of complications during allergen-specific immunotherapy;
— allergic reactions during vaccination;
- other histamine-dependent allergic and pseudoallergic reactions.
When choosing an antihypertensive drug, preference is given to those drugs that best meet the requirements for this group of drugs, in particular, high clinical efficacy in AD (AR, CRC, etc.); high security; rapid absorption and onset of action, high bioavailability and long half-life, allowing for a long-term clinical effect after a single administration (at least 24 hours); the possibility of use together with other groups of medications (antibiotics, antifungals, cardiac drugs, etc.); no need to change the dose of the drug in case of dysfunction of the gastrointestinal tract, hepatobiliary, urinary, cardiovascular systems, etc., in elderly and senile age; absence of tachyphylaxis; lack of cumulation, etc. [10, 11].
Thus, when prescribing AGP, the doctor is guided by standard provisions: the presence of indications and contraindications for prescribing drugs, age, the presence of concomitant diseases, their severity and stage; It is important to take into account the individual characteristics of the patient. The patient’s desire to be treated and the ability to strictly follow the doctor’s instructions are of great importance.
Preventing recurrent heartburn
There are some rules that can help reduce the symptoms of heartburn.
To prevent heartburn, you need to follow simple rules that will help reduce the load on the stomach and reduce unpleasant symptoms:
- Small portions of food 4-5 times a day.
- Reduce consumption of very spicy, salty, fatty foods.
- Avoid carbonated drinks and foods that cause gas (soda, beer, simple carbohydrates)
- Raise the pillow 15-20 cm while sleeping.
- Try not to eat before bed and not to lie down after eating.
- Give up bad habits (alcohol, smoking).
- Reduce excess weight.
- Do not lean forward too much and do not strain, avoid lifting weights of more than 8-10 kg (do not strain your abdominal muscles).
- Remove corsets and tight belts from your wardrobe, wear looser clothes that do not squeeze your stomach.
How to eliminate allergy symptoms
The more free histamine is released, the more severe the allergic reaction. In some cases it causes inconvenience (constant sneezing, itchy eyes), in others it poses a threat to life (with bronchospasm a person cannot breathe). You can stop the reaction:
- stopping contact with the allergen;
- neutralizing histamine with an antihistamine;
- symptomatic therapy (for example, inhalation to immediately expand the lumens of the bronchi).
In the event of the development of anaphylactic shock, accompanied by a decrease in blood flow and laryngeal edema, it is important to promptly eliminate the threat to life. The set of measures includes the administration of adrenaline and ensuring air flow into the lungs (intubation).
Conclusion
Self-medication can be practiced for mild, rare symptoms. For this purpose, drugs from the group of antacids and alginates are used, and a single dose of Ranitidine 75 mg is also possible. If heartburn bothers you more than once a week , you need to consult a doctor . Taking medications should not be uncontrolled. Self-administration should not last longer than 7-10 days. Otherwise, you may not notice other serious diseases in time, one of the symptoms of which may be heartburn.
What can trigger an increase in histamine?
Allergens are substances that provoke increased release of histamine. Medicine has studied many allergens that can be divided into such groups.
Exogenous infectiousExogenous non-infectiousEndogenousVirusesFoodProtein-containing compounds that make up the cells of the bodyBacteriaPolenFungiIndustrialHouseholdMedicinal
Endogenous allergens are produced by the body itself. They cause autoimmune diseases (attacks of the immune system on healthy tissues).
Exogenous ones enter the body from the environment - through food, plant pollen, house dust. Industrial allergens include a variety of chemicals (dyes, cleaning products, fragrances).
Types of antihistamines
First-generation drugs could block histamine receptor signals only after penetrating the barrier between the circulatory and central nervous systems. As a result, the effects on the central nervous system could not be avoided. Because of this, antihistamines caused drowsiness and loss of coordination.
Pharmacologists took this shortcoming into account when creating second-generation drugs. They do not penetrate the mentioned barrier, act selectively, and do not have a sedative effect.
Third generation antihistamines are metabolites of their predecessors. They give the same effect at a lower dosage and do not affect the functioning of the cardiovascular system. However, some allergists and immunologists do not agree with separating them into a separate group and classify them as the second generation.
In 2015, the Consensus working group on new generation antihistamines led by Professor S.T. Holgate concluded that none of the existing drugs can be classified as third generation.
Examples of AGPs of different generations
AGP 1st generationAGP 2nd generationAGP 3rd generation*DiphenhydramineLoratadineCetirizineTavegilClaritinZyrtecSuprastinKestinCetrinDramamineVisin and Tizin AllergiTelfastDiazolinAllergodilFexofenadineAtarkcFenistilAllerfex
*according to supporters of their existence
II generation H1 blockers
Second generation antihistamines were developed to overcome the shortcomings of their predecessors. Unlike the latter, modern H1 blockers bind and dissociate from H1 receptors slowly. Due to their long-term connection with histamine receptors, they are able to provide a long-lasting effect, allowing them to be used 1-2 times a day. It has been proven that with regular use of all second-generation drugs for a month, their therapeutic response does not decrease, that is, tachyphylaxis does not develop.
Indications
Non-sedating antihistamines are the first-line treatment for mild to moderate forms of allergic rhinitis. They are appropriate to recommend to clients with minor symptoms of allergic diseases, as well as moderate allergies.
Advantages
Being comparable to the first H1 blockers in terms of antiallergic activity, representatives of the second generation do not exhibit sedation and many other adverse reactions, which is associated with their high selectivity and significantly lower ability to penetrate the blood-brain barrier.
The advantages include long-lasting action, the possibility of single use per day, and the absence of tachyphylaxis.
Portability
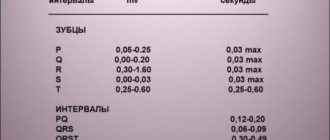
Despite the obvious advantages, some second-generation drugs have a rare but serious side effect - the ability to cause heart rhythm disturbances in the form of prolongation of the QT interval, development of ventricular arrhythmias), atrioventricular block and bundle branch block. Such arrhythmias are manifested by episodes of dizziness and fainting, but can often be asymptomatic.
The cardiotoxic effect is dose-dependent. When using drugs in therapeutic doses, arrhythmogenic properties practically do not appear. This is due to the fact that most second-generation antihistamines are prodrugs that are almost undetectable in the bloodstream due to rapid biotransformation with the formation of active and long-acting metabolites. It should be noted that the biotransformation of second generation antihistamines occurs with the help of the isoenzyme of the cytochrome P450 system, the activity of which can be inhibited by some drugs, in particular, ketoconazole, itraconazole, fluoxetine, a flavonoid contained in grapefruit juice and a number of others.
In case of overdose, increased concentration of the prodrug in the blood, as well as conditions in which the rate of biotransformation of the drug decreases (for example, cirrhosis of the liver, simultaneous administration with drugs that inhibit the activity of the cytochrome P450 system isoenzyme), the severity of the cardiotoxic effect of second-generation H1 blockers increases. Additional risk factors include pre-existing long QT syndrome, concomitant use of drugs with arrhythmogenic activity, and electrolyte disturbances.
At the same time, when used correctly, following the dosage regimen and contraindications, second generation antihistamines are well tolerated and can be considered safe for the treatment of allergic diseases.
Loratadine, both the drug itself and its active metabolite, as well as desloratadine and fexofenadine, do not have arrhythmogenic properties. By the way, the latter are not metabolized with the participation of the isoenzyme of the cytochrome P450 system and do not enter into drug interactions with drugs that inhibit its activity.
What should you warn the client about?
When dispensing drugs of this subgroup, it is important to recall the need to adhere to the dosage regimen in order to avoid the development of side effects, in particular, cardiotoxicity.
In addition, it is appropriate to draw the client’s attention to the fact that second generation antihistamines should not be taken simultaneously with drugs that compete with them for hepatic metabolism (ketoconazole, itraconazole, ranitidine, fluoxetine and others).