What is RFMK, thrombinemia
Dear Luna 78!
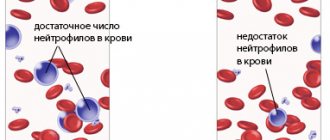
Soluble fibrin monomer complexes (SFMCs) are markers of thrombinemia during intravascular coagulation. The RFMK test allows you to quantify the level of soluble fibrin in plasma, that is, the level of thrombinemia. An increase in the number of RFMK is observed during thrombosis, DIC syndrome, and in late pregnancy in accordance with the increase in fibrinogen content. RFMK is a marker of intravascular coagulation. Thus, its increase indicates the development of DIC syndrome.
Coagulogram: everything you need to know about coagulation
Blood coagulation is a multi-stage, complex process and, at the same time, sensitive to the action of a number of factors. At the same time, the symptoms of “problems”, as a rule, do not make themselves felt for a long time. And clotting tests often reveal abnormalities “by chance.” So who should keep hemostasis “under supervision”? And how can those who are already undergoing treatment understand the indicators?
Who is the analysis for?
Blood clotting testing is primarily indicated for those who:
- suffers from liver disease or has had hepatitis in the past (since most clotting factors are synthesized in the liver);
- suffers from or has a hereditary predisposition to thrombophlebitis and varicose veins;
- suffers from cardiovascular or autoimmune diseases (high risk of vascular inflammation and, as a result, increased thrombosis);
- takes oral contraceptives or has excess estradiol (women);
- miscarriage in the patient’s personal history
Significant risk factors such as smoking, excess weight, sedentary lifestyle, age over 40, frequent flights and others should not be excluded from attention.
And, of course, such an analysis is mandatory before any operation, as well as for those who are already taking “anti-coagulant” drugs.
What the indicators say
The set of “standard” coagulograms (50.0.H94.203) includes the definition of:
- APTT,
- Prothrombin (time, INR),
- Thrombin time
- Fibrinogen.
But what do these indicators mean?
1. APTT, or activated partial thromboplastin time
Estimates the rate of blood clot formation after adding special reagents to plasma, and is measured in seconds.
In other words, APTT demonstrates the effectiveness of stopping bleeding due to plasma coagulation factors (precisely those that are formed in the liver).
At the same time, a lengthening (increase) of the indicator signals the risk of bleeding, and a shortening indicates thrombosis.
And the analysis is especially “relevant” for people taking direct anticoagulants (heparin and others).
2. Prothrombin time (PT)
This is the time period during which the formation of fibrin threads, that is, the actual precursor of a blood clot, occurs.
The indicator is measured as a percentage of the norm, which is 70-120%.
The higher this indicator, the higher the rate of thrombus formation, and therefore the risk of thrombosis.
A decrease in PV is a signal of a tendency to bleeding.
3. INR
In essence, it is a calculated indicator designed to standardize data on prothrombin time obtained using different equipment.
Such “difficulties” have become necessary due to the fact that INR is the basic analysis for the selection and correction of “anticoagulant” drugs (such as warfarin). And data obtained on different equipment (in different laboratories) often did not allow comparison with each other.
Therefore, the International Committee for Standardization in Hematology and the International Committee on Thrombosis and Haemostasis introduced the use of INR in 1983.
And today, its level for a healthy person is at the level of 0.8-1.2. And for those taking indirect anticoagulants – 2.0-4.0.
At the same time, an increase in INR is associated with the risk of bleeding, and a decrease of less than 0.5 may indicate thrombosis.
4. Fibrinogen
Unlike previous indicators, this is directly a substrate for the formation of a blood clot. That is, not an indicator of speed, but a substance. Therefore, the norms for fibrinogen are measured in grams per liter.
An increase in fibrinogen is observed not only with increased thrombus formation, but also with many inflammatory processes (as a way for the body to limit the spread of the “causal factor” and destroyed tissues). And also for those who take oral contraceptives or have elevated estrogen levels, pregnant women, people with high cholesterol and smokers.
A decrease in the indicator can indicate not only the risk of bleeding, but also liver disease.
Of course, the listed indicators are only a “base” for assessing the “health” of the blood coagulation system. And if significant deviations are detected, additional markers may be needed.
Changes in hemostasis in pregnant women
During pregnancy, the hemostatic system plays an important role in maintaining the normal functioning of the placenta and the condition of the unborn child. During this period of a woman’s life, physiological changes occur in the hemostasis system, caused by the appearance of an additional “third” circle of blood circulation—the uteroplacental one. Changes in the volume of circulating blood and hormonal levels, as well as preparation for natural blood loss during childbirth also affect the “pregnant restructuring” of the blood. However, significant changes in the hemostatic system of a pregnant woman are not only undesirable, but also dangerous.
What are the dangers of elevated RFMC levels during pregnancy?
We do not intend to intimidate the expectant mother, but we want to remind you that the significantly increased result is not caused by harmless reasons. It can be:
- Thrombophilia, which is usually hereditary in nature and manifests itself especially aggressively during pregnancy. This pathology, creating a high risk of clot formation, interferes with the normal course of the pregnancy process (miscarriages). The task of the gynecologist in this case is to carefully consider a plan of therapeutic measures that create conditions for bearing the fetus for up to 7 months (35 - 36 weeks), when the baby, although weak, is quite viable;
- A history of thrombosis during pregnancy may reappear, so this condition is considered an indication for more frequent testing of soluble fibrin-monomer complexes;
- Disseminated intravascular coagulation syndrome, which can be caused by a variety of causes (infections, shock, trauma, autoimmune diseases, neoplasms, late toxicosis, purulent inflammation, cardiovascular and other chronic pathologies), during childbirth can become an uncontrollable process with a very sad end. . The risk of developing disseminated intravascular coagulation syndrome makes it necessary to monitor the level of RFMC very often, which the expectant mother must understand and strictly follow the doctor’s prescriptions in order to save the life of herself and her child.
To avoid severe complications during childbirth (in particular, disseminated intravascular coagulation syndrome), unscheduled administration of additional coagulogram parameters (RFMC, D-dimer, etc.) is indicated in the presence of:
- Severe diseases of the liver, kidneys, lungs;
- Autoimmune diseases;
- Cardiovascular pathology;
- Neoplasms;
- Varicose veins of the lower extremities;
- Diseases of the endocrine system, for example, diabetes;
- Purulent inflammation;
- Gestozov;
- Increased RFMC before pregnancy;
- Bad habits (smoking – primarily, including passive smoking);
- Pregnancy that occurs after artificial insemination using IVF;
- Multiple pregnancy.
Any deviations from the normal values of hemostasiogram parameters should be carefully rechecked and studied. If the RFMC is elevated for several weeks, the gynecologist, depending on the degree of increase in the indicator, prescribes treatment, which often takes place in a hospital setting (this, first of all, applies to cases when the concentration jumps sharply and exceeds the norm several times). A pregnant woman, for her part, must be aware of her share of responsibility in order to prevent terrible complications and fully experience the happiness of motherhood. Unfortunately, there are undisciplined pregnant women who ignore doctor’s advice, do not come for tests on time, refuse hospitalization, lead an unhealthy lifestyle, and then indiscriminately make complaints to all doctors in a row.
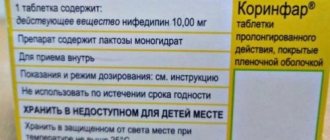
Treatment of DIC syndrome, coagulation disorders, hypercoagulation
If there is a history of problematic pregnancy or miscarriage, then aspirin and/or dipyridamole (chimes), heparin may be prescribed. It is necessary to focus more on your own well-being and the nature of the pregnancy. Considering that normal levels of fibronogen in pregnant women are 2.6 - 5.6 g/l, RFMC up to 5.1 mg/100 ml, you need to make an appropriate correction. It is better to contact the doctor who is managing your pregnancy and consult with him.
Sarklinik wishes you and your future baby good health.
Related posts:
Rigoni-Golyani hormonal test, testosterone, how it is carried out, what it is needed for
Shouting obscene words, phrases, treatment in Russia, Saratov
Lost erection with wife
Problem with feces, child straining, smearing panties, encopresis
Panic attacks, vzd, vegetative-vascular dystonia, neurosis, treatment in Saratov
Comments ()
Norm, increased and decreased values of RFMK
The rate of soluble fibrin-monomer complexes does not vary greatly and is 3.38 + 0.02 mg/100 ml, while the concentration of RFMC should not exceed the upper limit of 4.0 mg/100 ml (according to individual sources).
Meanwhile, as for other tests, you should pay attention to the reference values of a particular laboratory; in some, the norm can be up to 5.0 mg/100 ml or even higher. And a person, focusing on the norm of up to 4 mg/100 ml, may needlessly become nervous. However, is it worth worrying if (based on reference values) it is obvious that the RFMK is increased? Absolutely, because an increased result indicates activation of the coagulation system and, as a rule, no one can tell in advance how this could end.
RFMC is of great importance during pregnancy, where this study is highly desirable for every expectant mother, because thrombosis and disseminated intravascular coagulation are considered to be the main complications that pose a serious threat to the life of a woman and her unborn child. The reasons for increased concentrations of RFMC during pregnancy and the consequences of this phenomenon will be given a separate section below, but for now we will focus on other cases that require the appointment of this analysis. The list of coagulograms is expanded to include RFMC if:
- The patient is awaiting surgery (especially a major one);
- There is a suspicion of the development of thrombosis, thrombophilia or DIC syndrome;
- The patient is given anticoagulant treatment (heparin);
- A woman plans to conceive a child using IVF;
- Pregnancy has occurred and the woman is registered at the antenatal clinic, that is, during the initial examination, then at the beginning of the third trimester and the last analysis, if the pregnancy is proceeding normally, closer to childbirth - between 33 and 37 weeks.
Sometimes the concentration of soluble fibrin-monomer complexes does not reach the above norm. The cause of this phenomenon is usually the use of heparin, so with the help of this test you can monitor the effectiveness of heparin therapy, determine the timing of the start of prophylaxis or the end of the course of anticoagulant treatment.
Preparation for the study, the analysis itself
Such a laboratory test as determining the quantitative content of soluble fibrin-monomer complexes requires, in principle, the same preparation as any biochemical analysis, that is, nothing supernatural.
To avoid the need for repeated rechecks due to receiving inadequate results, you should try to fulfill simple requirements the night before and on the day of the test:
- Having had a normal dinner and even drinking tea or kefir later (it is better to do this before 10 o’clock in the evening), do not eat food in the morning, do not drink any drinks, do not satisfy your hunger with smoking breaks, be patient;
- The use of medications, pharmaceutical and folk, that help thin the blood should be stopped 24 hours before the study, otherwise the information will be unreliable;
- For 1–2 days, try to avoid psycho-emotional stress and excessive physical exertion.
The test itself is done quickly, but whether the patient receives an answer depends on the workload of the laboratory: in some places the results can be obtained in the evening, but in others you will have to wait 2-3 days.
Blood, as usual, is taken from a vein located in the elbow area. Well, then it’s a matter of technology and specialists.