Heart defects are various anomalies of the valve apparatus, septa, large vessels and individual parts of the heart, causing circulatory disorders.
There are a huge number of heart defects, each of which is dangerous to human health in its own way. Almost always, a heart defect requires surgical intervention.
1 Holter - diagnosis of heart defects
2 Diagnosis of heart defects
3 ECG for heart defects
Structural pathology of the heart can begin to develop in a person in the mother's womb - this phenomenon is called congenital heart disease . The cause is usually chromosomal abnormalities or infections suffered by the mother. From 5 to 8 babies out of a thousand are born with this defect. The defect can be detected through fetal ultrasound.
If the disease appears as a consequence of injury, infection or systemic disease, we are talking about acquired heart disease .
At its core, the defect is a collective name for diseases of different parts of the heart. Both types of heart defects have many subtypes, with varying degrees of severity and consequences for human health.
Types of heart defects
In most cases, heart defects affect the valve apparatus. Complications that arise as a result of this pathology can cause early disability and even death.
The main role of the valve apparatus is to freely pass blood through itself when the heart contracts and to delay the reverse movement of blood through the valve when relaxing, maintaining a rhythmic and continuous flow of blood. Defective valves cease to fully perform this work and function, which is why blood hardly flows through the narrowed valve into the cavity of the heart and does not fully leave the chambers or flows back through a closed valve.
Acquired heart defects:
- valve insufficiency (incomplete closure of the valves or damage to the valves) - causes reverse blood flow;
- valve stenosis (narrowing of the lumen between the open valves) - complicates blood circulation;
- prolapse (bulging) of the valve, as a result of which its leaflets bulge into the heart cavity, and often reverse blood flow occurs due to insufficient closure of the valve.
In cardiological practice, combined and associated defects are often encountered, in which several valves are affected at once.
Most often, the mitral (mitral heart disease) and aortic (aortic heart disease) heart valves suffer from abnormal changes.
Congenital heart defects:
- atrial septal defect;
- ventricular septal defect;
- patent ductus arteriosus;
- transposition (violation of position) of large great vessels;
- coarctation of the aorta;
- pulmonary stenosis, etc.
Congenital heart defects can occur either individually or in combination with each other. Thus, the combination of right ventricular hypertrophy, transposition of the aorta, ventricular septal defect and stenosis of the right ventricular outflow tract is called tetralogy of Fallot (or blue heart disease).
1 X-ray for heart defects
2 Diagnosis of heart defects using x-rays
3 Ultrasound for heart defects
Publications in the media
Classification of congenital heart disease by severity classes (J. Kirklin et al., 1981) • Class I. It is possible to perform a planned operation later than 6 months: VSD, ASD, radical correction for tetralogy of Fallot • Class II. Elective surgery can be performed within 3–6 months: radical correction for VSD, open atrioventricular canal (PAVC), palliative correction for TF • Class III. A planned operation can be performed within a period of up to several weeks: radical correction for transposition of the great vessels (TMS) • Class IV. Emergency surgery with a maximum preparation time of several days: radical correction for total anomalous pulmonary vein drainage (TAPD), palliative correction for TMS, VSD, OAVC • Class V. The operation is performed urgently due to cardiogenic shock: various types of defects in the decompensation stage.
Classification of congenital heart disease by prognostic groups (Fyler D., 1980) • 1 group. Relatively favorable prognosis (mortality during the first year of life does not exceed 8–11%): patent ductus arteriosus, VSD, ASD, pulmonary stenosis, etc. • Group 2. Relatively unfavorable prognosis (mortality during the first year of life is 24–36%): tetralogy of Fallot, myocardial diseases, etc. • Group 3. Poor prognosis (mortality during the first year of life is 36–52%): TMS, coarctation and stenosis of the aorta, tricuspid valve atresia, TADLV, single ventricle of the heart, OAVC, origin of the aorta and pulmonary artery from the right ventricle, etc. • Group 4. Extremely unfavorable prognosis (mortality during the first year of life is 73–97%): hypoplasia of the left ventricle, pulmonary atresia with an intact interventricular septum, common truncus arteriosus, etc.
Classification of congenital heart disease according to the possibility of radical correction (Turley K. et al., 1980) • 1 group. Defects for which only radical correction is possible: aortic stenosis, pulmonary artery stenosis, TADLV, triatrial heart, coarctation of the aorta, patent ductus arteriosus, aortopulmonary septal defect, ASD, mitral valve stenosis or insufficiency • Group 2. Defects in which the advisability of radical or palliative surgery depends on the anatomy of the defect, the age of the child and the experience of the cardiology center: various variants of TMS, pulmonary atresia, common truncus arteriosus, tetralogy of Fallot, OAVC, VSD • group 3. Defects for which only palliative operations are possible in infancy: a single ventricle of the heart, some variants of the origin of the great vessels from the right or left ventricle with pulmonary stenosis, atresia of the tricuspid valve, atresia of the mitral valve, hypoplasia of the ventricles of the heart. Abbreviations • PAVK - patent atrioventricular canal • TMS - transposition of the great vessels • TADPV - total anomalous drainage of the pulmonary veins.
ICD-10 • Q20 Congenital anomalies [malformations] of the heart chambers and connections • Q21 Congenital anomalies [malformations] of the cardiac septum • Q22 Congenital anomalies [malformations] of the pulmonary and tricuspid valves • Q23 Congenital anomalies [malformations] of the aortic and mitral valves • Q24 Other congenital anomalies [malformations] of the heart.
Causes of heart defects
Causes of congenital defects (CHD):
- chromosomal and genetic abnormalities;
- infections suffered during pregnancy (for example, rubella, etc.);
- maternal alcoholism and drug addiction;
- side effects of medications;
- irradiation.
Causes of acquired defects:
- infectious, rheumatic endocarditis (rheumatic heart defects, chronic rheumatic heart disease, infective endocarditis - usually insufficiency of the aortic, mitral and tricuspid valves);
- systemic connective tissue diseases;
- heart injuries;
- sepsis;
- infectious diseases (especially syphilis);
- oncology.
Risk factors for developing heart defects
- hereditary predisposition (CHD);
- complications during pregnancy (CHP);
- taking medications (toxic to the fetus) during pregnancy (CHD).
1 Laboratory diagnostics for heart defects: tests
2 VEM for heart defects
3 ECHO-kg for heart defects
Acquired heart defect. Acquired heart defect. Treatment
Classification
Based on the reasons for the formation of defects, the following classifications of the disease are distinguished:
- degenerative;
- rheumatic;
- consequence of endocarditis;
- syphilitic.
There are also functional pathologies of congenital defects. There are three types of violations:
- simple (single) – valve insufficiency, wall stenosis;
- combined – pathologies of several valves;
- combination – several defects localized in one place.
It is important to note that the mitral valve is at greater risk than the aortic valve. The most rare defects are the tricuspid and pulmonary regions.
Diagnosis
An important indicator is the presence of acoustic signs of a defect - noise. A complete medical history of the patient is collected, diseases that could lead to the development of a cardiac defect are determined.
Muscle hemodynamics can be impaired to several degrees:
- weak;
- moderately;
- clearly expressed.
It is mandatory to examine the patient for shortness of breath, cyanosis and swelling. The doctor listens to the heart muscle for the presence of murmurs. The percussion method is used to identify the boundaries of the organ.
An ECG is used for diagnosis. More accurate methods and localization of the disease can be determined using intraesophageal electrocardiography.
MRI and MSCT methods of the heart are quite informative. Tomography gives the doctor numerous sections of the heart muscle, which allows a more accurate assessment of the condition of the organ. In this case, the specialist is based not on a subjective opinion, but on physically prepared images of the heart.
Treatment, prognosis
The capabilities of the main human muscle are not limitless - the progression of the disease gradually depletes the organ’s reserves. The development of heart failure causes a decompensated defect, which can be aggravated by various factors - from psychological to physical.
Conservative treatment is effective in the early stages of the disease. This approach requires the patient to be attentive and follow the doctor’s clear instructions.
Acquired defects can be treated promptly if:
- there is a risk of progression of heart failure;
- valve changes have a major impact on hemodynamics;
- conservative treatment does not bring visible effect;
- there is a possibility of acute complications.
Take care of your heart and at the slightest suspicion, contact a specialist.
For all questions related to the diagnosis and treatment of cardiovascular diseases, you can contact our medical cardiologist.
Symptoms of heart defects
The manifestations of the disease depend entirely on the severity of the lesion.
Thus, mild congenital and acquired defects in the early stages of development can occur unnoticed and have no effect on well-being. However, it should be remembered that severe congenital heart defects often affect the appearance, physical development and resistance of the body. Therefore, blueness or pallor of the skin, low height and weight, as well as a tendency to frequent colds may themselves be symptoms of the disease.
With acquired and congenital defects of moderate severity, obvious symptoms of heart failure appear (shortness of breath during exercise, swelling of the legs), dizziness, tachycardia, weakness, and fatigue.
Severe congenital (for example, blue heart disease) and acquired (valve insufficiency in combination with aortic stenosis) heart defects may be accompanied by symptoms of acute heart failure (asphyxia, pulmonary edema).
Common symptoms of heart disease:
- dyspnea;
- arrhythmia (usually tachycardia);
- cyanosis of the skin (blueness) or pallor;
- dizziness, weakness;
- swelling of the veins of the neck and head;
- decreased blood pressure;
- fainting.
1 Diagnosis of heart defects
2 Diagnosis of heart defects
3 Stress test for heart defects
I51.9 Heart disease, unspecified: description, symptoms and treatment
from 2000-2015. REGISTER OF MEDICINES OF RUSSIA ® RLS ®
Classification of acquired heart defects
(Adopted at the VI Congress of Cardiologists of Ukraine, Kyiv, 2000) Mitral stenosis:
Rheumatic 1.05.0 Non-rheumatic 1.34.2 (with clarification of etiology) Stage I - compensation Stage II - pulmonary congestion
stage - right ventricular failure
stage—dystrophic
Stage V - terminal
Mitral regurgitation
Rheumatic 1.05.1 Non-rheumatic 1.34.0 (with clarification of etiology) Stage I - compensation Stage II - subcompensation Stage III - right ventricular decompensation Stage IV - dystrophic Stage V - terminal Combined rheumatic mitral disease (Rheumatic mitral stenosis with insufficiency: 1.05.2) C predominance of stenosis: stages and indications for surgical treatment, as in mitral stenosis With predominance of insufficiency: stages and indications for surgical treatment, as in mitral regurgitation Without obvious predominance: stages and indications for surgical treatment, as in mitral regurgitation Mitral valve prolapse 1.34.1 Aortic stenosis: Rheumatic 1.06.0 Non-rheumatic 1.35.0 (with specification of etiology) Stage I - full compensation Stage II - latent heart failure Stage III - relative coronary insufficiency GU stage - severe left ventricular failure Stage V - terminal Aortic failure:
Rheumatic 1.06.1 Non-rheumatic 1.35.1 (with specification of etiology) Stage I - full compensation Stage II - latent heart failure
stage—subcompensation
stage - decompensation
Stage V—terminal Combined aortic disease:
Rheumatic aortic stenosis with insufficiency 1.06.2 Non-rheumatic aortic (valvular) stenosis with insufficiency 1.35.2 (with clarification of etiology) With predominant stenosis: stages and indications for surgical treatment correspond to those for aortic stenosis With predominant insufficiency: stages and indications for surgical treatment correspond to those for aortic insufficiency 216
Without obvious predominance: stages and indications for surgical treatment correspond to those for aortic stenosis. Tricuspid stenosis:
Rheumatic 1.07.0 Non-rheumatic 1.36.0 (with specification of etiology) Tricuspid insufficiency:
Rheumatic 1.07.1 Non-rheumatic 1.36.1 (with specification of etiology) Combined tricuspid defect:
Rheumatic tricuspid stenosis with insufficiency 1.07.2 Non-rheumatic stenosis of the tricuspid valve with insufficiency 1.36.2 (with specification of etiology) Pulmonary artery stenosis 1.37.0 Pulmonary valve insufficiency 1.37.1 Combined pulmonary valve disease (Pulmonary stenosis with valve insufficiency 1.37.2 ) Combined heart defects:
Combined damage to the mitral and aortic valves 1.08.0 Combined damage to the mitral and tricuspid valves 1.08.1 Combined damage to the aortic and tricuspid valves 1.08.2 Combined damage to the mitral, aortic and tricuspid valves 1.08.3 The severity of “simple” defects is determined by three degrees:
I degree - insignificant II degree - moderate III degree - pronounced.
The severity of the defects in accordance with their clinical and instrumental characteristics are given below for individual nosological forms of heart defects.
It should be noted that heart disease is considered “combined” when there is stenosis and insufficiency of one valve and “combined” when several valves are affected. If there are several defects, they are listed, and the defect whose severity is greater is indicated first - for example, aortic valve insufficiency, mitral valve disease with a predominance of stenosis.
Considering that valve kalydinosis determines the tactics of surgical intervention, it has been proposed to distinguish 3 degrees of kalydinosis (Knyshov G.V. BendetYa.A. 1996).
Degrees of valve calcification
+ Individual lumps of calcium in the thickness of commissures or valves
++ Significant calcification of the valves and commissures without water
attraction of the valve ring III +++ Massive calcification of the valve with transition to the fibrous ring, and sometimes to the aortic wall and ventricular myocardium. The diagnosis also needs to take into account the etiological cause of the defect (rheumatism, infective endocarditis, atherosclerosis), the degree of heart failure.
For patients who have undergone heart valve surgery, the pre-existing defect should be identified, the date of surgical treatment, and the nature of complications should be indicated. For example, operated mitral heart disease with predominant stenosis, closed commissurotomy (date) or operated aortic valve disease with predominant insufficiency. Aortic valve replacement (specify type of prosthesis and date).
Along with heart defects caused by organic changes in the valve, there are dysfunctions of the valve in the form of relative insufficiency or relative stenosis. The cause of relative valve insufficiency may be a decrease in the tone of the papillary muscles or impaired function of the circular muscles, which normally reduce the lumen of the orifice during systole. With a decrease in the tone of these muscles, the opening remains large during systole, and even unchanged valve leaflets cannot completely cover it. The most typical is relative mitral valve insufficiency in aortic disease, which gives rise to talk about “mitralization of aortic disease.” Relative insufficiency of the valves of the great vessels is observed with an increase in the perimeter of the fibrous ring, in which the area of the valve leaflets is insufficient to completely cover the mouths of the vessels (more often relative insufficiency of the pulmonary valve). Relative stenosis occurs in cases of a sharp increase in blood flow through a normally sized hole, for example, with severe regurgitation of the mitral or aortic valves. The addition of relative valve insufficiency or relative stenosis, despite changes in auscultatory signs and the course of the disease, does not provide grounds for designating the defect as combined.
Diagnosis of heart defects
After talking with the patient, collecting complaints and physical examination, the cardiologist prescribes laboratory and hardware tests.
Methods for diagnosing heart defects:
- biochemical and clinical blood tests;
- electrocardiography (ECG);
- 24-hour Holter ECG monitoring;
- Ultrasound of the heart (ECHO-CG);
- chest x-ray;
- MSCT or MRI of the heart and large vessels;
- Transesophageal ECHO-CG.
Most of the listed diagnostic methods are also used to determine indications for surgical treatment of heart defects.
Treatment of heart defects
Drug treatment for heart defects is generally not considered effective. Therefore, therapy is aimed at antibacterial treatment for acute rheumatism, eliminating the manifestations of chronic rheumatic heart disease, heart failure and other severe complications. The only correct way to treat heart defects today is surgery.
Surgical methods for treating heart defects:
- valve replacement - in case of severe valve insufficiency and severe stenosis, the defective valve is replaced with an artificial one (there are mechanical and biological prosthetic heart valves);
- implantation of several prosthetic heart valves - for combined and combined defects;
- closing the atrial/ventricular septal defect - applying a suture or patch made of artificial material;
- ligation of the patent ductus arteriosus;
- X-ray surgery, transcatheter operations on the beating heart (closure of septal defects with Amplatzer, transcatheter implantation of the aortic valve - TAVI, application of a clip to the mitral valve leaflets in case of severe mitral valve insufficiency, closure of the patent ductus arteriosus, etc.).
In our clinic you can undergo diagnosis and treatment of heart defects. Our cardiologists are also knowledgeable in the outpatient management of patients with heart defects and in the outpatient management of patients with prosthetic heart valves.
Everything necessary for high-precision diagnosis of heart defects and other diseases of the heart and blood vessels is at the disposal of the cardiology department of the MedicCity clinic. You can undergo a full examination of the heart and blood vessels - ECG, ultrasound of the heart, bicycle ergometry, 24-hour blood pressure monitoring and ECG on a 12-channel holter at a convenient time by appointment.
Our clinic staff consists of only experienced specialists with serious scientific training and many years of medical practice!
Mitral stenosis.
II Acquired heart defects.
Heart disease is an anatomical change in the valve apparatus of the heart or the interatrial, interventricular septum and other defects.
Based on their origin, defects are divided into:
- Congenital - arise as a result of a violation of the formation of the heart and blood vessels in the embryonic period.
- Acquired - acquired changes in the heart valves, leading to dysfunction and hemodynamics; acquired defects are a complication of various diseases.
Combined defect is a combination of two defects of one valve. For example, mitral stenosis and mitral insufficiency.
Combined defect - a combination of defects of several valves, for example, mitral stenosis and aortic insufficiency.
An isolated defect is one defect of one valve, for example, mitral regurgitation.
Compensated defect - no complaints, no signs of circulatory failure.
Decompensated defect - complaints of circulatory failure of the left ventricular or right ventricular type appear.
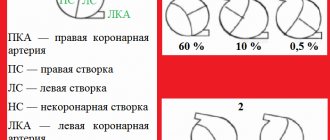
MITRAL HEART DEFECTS.
Mitral stenosis is a narrowing of the left atrioventricular orifice, which prevents the physiological flow of blood from it into the left ventricle during systole of the left atrium.
Mitral insufficiency is the inability of the left atrioventricular valve to prevent the reverse movement of blood from the left ventricle into the left atrium during ventricular systole, that is, incomplete closure of the mitral valves.
Mitral valve prolapse (MVP) is a pathological sagging (bending) of one or both mitral valve leaflets into the left atrium during left ventricular systole.
I05.0 Mitral stenosis, rheumatic.
I05.1 Rheumatic mitral valve insufficiency
I05.2 Mitral stenosis with insufficiency
I05.8 Other diseases of the mitral valve (mitral insufficiency).
I05.9 Mitral valve disease, unspecified
EPIDEMIOLOGY and ETIOLOGY.
■ Mitral stenosis almost always occurs as a result of an acute rheumatic attack, more often in women.
On average, the latent period from the moment of rheumatic heart disease (carditis) to the development of clinical manifestations of the defect is about 20 years, so the disease manifests itself between 30 and 40 years of life.
■ Mitral insufficiency. Causes: MVP, rheumatism (30%), atherosclerosis, infective endocarditis, trauma, connective tissue diseases. In men, mitral insufficiency is more common.
■ PMK. Causes: rheumatism, infections, ischemic heart disease.
CLASSIFICATION.
- The classification of mitral stenosis by severity is based on the severity of the narrowing of the left atrioventricular orifice (mild, moderate and severe stenosis).
- The classification of mitral regurgitation by severity is determined by the volume of regurgitant blood (4 degrees of mitral regurgitation).
PATHOGENESIS
Through the narrowed left atrioventricular orifice, not all the blood during left atrium (LA) systole enters the left ventricle (LV), as a result, an excess volume of blood is formed in the left atrium (remaining after systole and re-entered from the pulmonary veins during subsequent diastole) , this leads to hypertrophy of the left atrium (compensation stage), over time, the atrial myocardium is depleted, the cavity of the left atrium expands, decompensation develops, as a result, the pressure in the ICC increases and hypertrophy of the right ventricle (RV), and then the right atrium (RA) develops.
Your opinion is important to us! Was the published material useful? Yes | No