Neurologist
Chudinskaya
Galina Nikolaevna
Experience 29 years
Neurologist, member of the Association of Interdisciplinary Medicine
Make an appointment
Stroke is an acute cerebrovascular accident (CVA) that causes damage and death of nerve cells. The name itself comes from the Latin word “insultus”, translated as “strike, attack”. Previously, the pathology was called apoplexy (apoplexy), as the Greeks called paralysis - one of its main symptoms and consequences.
The disease is more common than acute myocardial infarction. Over 15 million cases are registered annually in the world. They account for 10% of all deaths (almost 6 million per year), which makes stroke the “No. 2 cause of death” on the planet after coronary heart disease (CHD). But in most episodes, the consequence of stroke is not death, but limitation of life activity; this is the leading cause of disability among people in the older age group.
About 60% of stroke patients have persistent neurological disorders that interfere with their normal lifestyle. Typical abnormalities include impaired movement and ability to move, difficulty swallowing, a high risk of speech and visual disorders, falls, and fractures. Emotional (depression) and cognitive (up to the stage of dementia) disorders are often observed.
Symptoms, signs of stroke
All symptoms of a cerebral stroke develop sharply, quickly, and appear suddenly:
- weakness, numbness, loss of sensitivity, paralysis of one half of the body or face, arms, legs;
- intense headache, described by patients as the worst in life;
- speech impairment (a person cannot speak or has difficulty doing so), misunderstanding of the interlocutor’s speech;
- deterioration in clarity of vision, it is unfocused or completely absent in one eye;
- dizziness, loss of coordination of movements, balance, walking, and sometimes loss of consciousness;
- nausea, vomiting.
Important: if you witness such symptoms, call an ambulance immediately! A stroke is an emergency condition that requires immediate emergency hospitalization!
Uninformed people can easily mistake such signs for alcohol or drug intoxication, so it is extremely important to know and distinguish the symptoms. After all, the speed of medical care plays a key role here - literally minutes count, death from stroke is directly related to delay. The sooner the victim is hospitalized, the less the consequences of a stroke will be and the higher the chances of saving life.
To make it easier to determine the occurrence of a stroke, doctors recommend using three basic recognition techniques. They are called the “UZP” rule, an abbreviation for the first letters of the words denoting the action that a person is asked to perform:
- U - smile. During a stroke, the smile often looks “crooked”, unnaturally skewed, when one corner of the mouth is lowered and the other is raised.
- Z – speak. Say a simple sentence like “Today they promised good weather.” Often (but not always!) there is incorrect pronunciation.
- P – raise your arms at the same time. If one arm involuntarily lags behind in movement or drops, there is a high probability of stroke.
When calling an ambulance, be sure to describe your symptoms to the dispatcher; such cases require calling a specialized resuscitation team and transporting them to a specialized clinic. You should not try to transport the patient to the hospital yourself, since not all medical institutions can provide the required set of emergency medical measures and precious time will be lost.
First aid for stroke
Before the medical team arrives, you need to provide assistance to the patient:
- Place in a horizontal position, raising the shoulders, neck and head 30° relative to the body (place a pillow, a cushion of clothing).
- Provide access to fresh air (unfasten tight clothing, open a window).
- Turn his head to the side to prevent vomit from entering the respiratory tract.
Under no circumstances should you give food or water - partial paralysis of the swallowing organs can cause food or drink to enter the respiratory system and subsequent suffocation. In other words, a person may choke or choke, which is likely to cause death due to stroke.
How to help a person with a stroke
If signs of acute cerebrovascular accident are detected, emergency assistance must be called as soon as possible!
The procedure for providing assistance before the ambulance arrives:
- reassure the victim so as not to aggravate the situation with excitement;
- put the patient on the bed, raise his head 30 degrees; if consciousness is lost, turn your head to the side (vomiting is possible), stretch out your tongue;
- loosen clothes - collar, belt; ensure air flow;
- measure blood pressure and, if it is elevated, give medications to lower it;
- Place your feet in a bowl of hot water or place a heating pad on your feet to help drain blood from the brain.
Prohibited:
- Give the patient vasodilators until the ambulance arrives.
- Give water or food to the patient.
A special case is when a stroke occurs in a car and the victim is driving. Here, not only his life, but also the lives of passengers may be at risk. In this case, you need to stop, call an ambulance, and open all the windows.
Causes of stroke
A stroke is caused by a disruption in the normal flow of blood to an area of the brain due to stenosis (narrowing), embolism (blockage), or rupture of a cerebral artery. If brain cells do not receive enough oxygen and nutrients, they die.
Embolism and stenosis most often develop against the background of atherosclerosis, when an atherosclerotic plaque narrows the lumen of the vessel and promotes the formation of a blood clot. A detached blood clot completely blocks the vessel, this is called thromboembolism. Vascular rupture (essentially, intracerebral hemorrhage) can occur with arterial hypertension (high blood pressure), aneurysm, or severe traumatic brain injury.
There are a number of pathologies, the presence of which significantly increases the risk of stroke:
- cerebral atherosclerosis;
- atrial fibrillation;
- myocardial infarction;
- high blood pressure;
- varicose veins;
- blood clotting disorder;
- diabetes;
- obesity;
- sedentary lifestyle;
- smoking, alcoholism.
The risk of developing this terrible disease increases after 30 years of age, especially in weather-dependent people, as well as in those exposed to chronic stress, regular overwork, and constant excessive physical exertion.
Classification of strokes
There are two types of stroke - ischemic and hemorrhagic:
- Ischemic (also known as cerebral infarction) occurs when the lumen of a blood vessel in the neck or brain is narrowed or completely blocked by a blood clot.
- Hemorrhagic - when hemorrhage occurs in the brain due to a rupture of the vessel wall, as a result of which nerve tissue is compressed, cerebral edema and displacement of brain structures are formed.
- Separately, a transient ischemic attack (TIA) should be mentioned - a short, from 10 minutes to several hours, disturbance of blood circulation in the brain. It is accompanied by symptoms characteristic of a stroke (headache, paresis, speech disorder, etc.), but differs in the short duration of their manifestations and the reversibility of the disorders. In most cases, TIA goes away on its own, without medical attention.
Sometimes people do not attach much importance to TIA due to the transience of this condition and the absence of complaints afterwards. But a TIA indicates a high risk of a full-blown ischemic stroke in the future, often within a few days or weeks. Therefore, such a patient must undergo a full examination to prevent stroke.
About 80% of all strokes are ischemic. There is a generally accepted classification of ischemic stroke according to the mechanism of development:
- Atherothrombotic - among all others, it is recorded in 40-60% of cases. Occurs as a result of atherosclerotic lesions of the precerebral or great cerebral artery. I get sick more often in people over 60 years of age. Often this type of stroke occurs during sleep, preceded by a TIA attack.
- Embolic stroke - develops against the background of mitral or aortic valve disease, after myocardial infarction, with endocarditis, paroxysm of atrial fibrillation, post-infarction aneurysm. The onset is sudden, in a state of wakefulness, the predominant age of patients is 50-65 years.
- Lacunar - due to damage to the small cerebral arteries that supply the deep parts of the brain. A type of stroke characterized by concomitant high blood pressure develops gradually over several hours.
- Hemodynamic – occurs in the presence of severe stenosis of the main arteries, subject to a sharp drop in blood pressure due to:
- orthostatic hypotension;
- deep sleep;
- hyperventilation;
- overdose of antihypertensive drugs;
- myocardial infarction;
- heart rhythm disturbances, etc.
What to do if you have a stroke? The neurologist has compiled simple instructions that can save you
Over the course of a year, more than 30,000 people have a stroke in Belarus. Only 10% of them return to normal life. Neurologist Sergei Marchenko tells how to identify a stroke and what needs to be done before it is too late.
What is a stroke anyway?
– This is an acute circulatory disorder in the brain, which is always a secondary disease. It does not occur in healthy people.
According to the mechanism of circulatory disorders, strokes are divided into ischemic (about 85% of all strokes) and hemorrhagic. In the first case, the vessel is blocked by a thrombus (embolus), in the second, the vessel ruptures. There is also a division of strokes according to severity, but even a mild stroke is a deadly disease.
Do these types have the same symptoms?
Stroke symptoms depend on the location in the brain, not the type of stroke. If blood circulation in the speech center is impaired, speech will suffer, and in the motor center, movements in the arm and (or) leg will be impaired.
How can you tell if a person is having a stroke?
A very simple test has been invented to detect stroke, which is recommended by all national and international protocols. It’s called “Face, Hand, Speech, Time,” and based on it, emergency personnel have the right to make a diagnosis of stroke.
Face: Ask the patient to smile or show teeth. With a stroke, noticeable asymmetry of the face occurs (the corner of the mouth “hangs” on one side).
Arm: The patient is asked to raise and hold both arms 90° in a sitting position and 45° in a supine position for 5 seconds. During a stroke, one of the arms drops.
Speech: Ask the patient to say a simple phrase. During a stroke, the patient is unable to clearly and correctly pronounce a simple phrase; his speech is unintelligible and slurred.
If there is at least one symptom indicating the development of a stroke, it is necessary to urgently call an ambulance - the sooner help is provided, the greater the chance of recovery.
Timing: It is very important to find out when the stroke occurred. You need to ask the person when he or others first noticed these violations. If a person cannot remember when they first noticed symptoms, we ask their loved ones when they last saw them without them.
There is the concept of a “therapeutic window” - the time when you can try to completely restore blood circulation. It refers to ischemic types of strokes, because when a vessel ruptures, you do not need to restore blood flow, but stop the bleeding and remove the hematoma.
The duration of the “therapeutic window” is no more than 6 hours. During the first four and a half hours, blockage of the vessel can be cured both with medications (i.e. using thrombolysis) and endovascular methods (using thrombus extraction) - that is, with the help of special devices that are inserted into the arteries of the brain and remove the blood clot mechanically. In the interval of 4.5–6 hours, only endovascular treatment is possible.
The success of stroke treatment depends entirely on the timing of seeking medical help. Unfortunately, if the symptoms are not very pronounced, people often wait for everything to go away on its own, but it doesn’t, and sometimes it only gets worse.
Can I use this test to determine if I have a stroke?
Certainly. If you realize that something is wrong with you, you can always smile at yourself in the mirror and see how symmetrical the smile is, evaluate your speech, try to hold both hands. But still, most often, strokes are diagnosed for someone. Relatives see that something is wrong with the person.
When a stroke occurs, what happens to the person at that moment? Does he faint and his condition deteriorate sharply?
All options are possible. When a large vessel is blocked, a person may lose consciousness because a large area of the brain is no longer supplied with oxygen. If the vessel is small, the symptoms may be subtle, but gradually become more pronounced.
Should all these symptoms occur during a stroke?
No. Symptoms can be all together, or just one of them: it all depends on how large the vessel is and what part of the brain is affected. In addition, it is important to remember the following nuances: the test only talks about the arm, but weakness may also be in the leg, and a person may develop coordination disorders.
The main thing: if your condition suddenly changes, do not wait, but immediately seek help! This applies not only to stroke; in medicine, a lot depends on time: it is difficult to successfully treat a surgical pathology when abdominal pain lasts a week, and for cardiologists to treat a myocardial infarction when the pain syndrome lasts more than 24 hours.
What can a stroke be confused with?
With diseases that cause the same symptoms. This could be a tumor, an injury, or an infectious lesion of the brain (encephalitis, meningitis). All these diseases are dangerous, and in any case they need to be treated, and not wait until they go away on their own.
These symptoms most likely will not go away on their own. And even if they disappear, you must go to the doctor. There is a concept of “transient cerebrovascular accident” - when neurological symptoms arise, but quickly pass because blood circulation is restored on its own within 24 hours. This is also a very dangerous condition, a harbinger of a full-blown stroke.
Is it possible to miss a stroke?
Can. The brain is responsible for everything in our body, but at the same time it has functionally insignificant zones: if a stroke occurs in one of them, the symptoms will be insignificant or completely unnoticeable. Such a stroke is often detected already in the form of old changes on brain tomograms.
How can I help someone who is having a stroke?
Call an ambulance by dialing 103. Afterwards, lay him down with his body elevated 30–45 degrees, ensure airway patency by freeing his neck from clothing and clearing the oral cavity of vomit and foreign objects, including removable dentures, in case of unconsciousness In case of patient's condition, he must be turned on his side to prevent saliva and vomit from entering the respiratory tract.
No other help should be provided: do not lower the pressure, do not give medications. Treatment for stroke depends on its type, and only a doctor can diagnose it.
What should I do if I have a stroke with speech impairment, and there is no one around?
If they are minor, try to make sure that the emergency medical dispatcher understands what you want. If that doesn’t work, try writing to someone you know and ask them to call you an ambulance.
What to do if a person has a stroke far from the city?
You still need to call an ambulance. Our entire country is divided into service zones; every location is assigned an ambulance substation, from where a team must arrive and provide assistance.
If it is completely out of the way and you understand that it will take a very long time to get there, it makes sense to load a person into a car and drive to the nearest town or hospital.
Currently in Belarus, active work is underway to organize regional vascular centers, which are designed to provide assistance to patients located in an approximately 70-kilometer zone, where both strokes and heart attacks will have to be treated using modern methods.
How does a stroke usually end?
Death, disability or recovery. Statistics on stroke outcomes have not changed for decades: 20–30% of patients die within a year, about 60% remain disabled in various groups, and only about 10% return to normal life.
If our fellow citizens began to seek help in a timely manner, fewer people would remain disabled.
About 60% of patients with strokes treated with thrombolysis or thromboextraction are discharged from the hospital with either no or minimal impairment - this does not take into account the rehabilitation period. This is why I am so happy about timely access to doctors: we have everything for treatment - knowledge, skills and technology.
What exactly are the consequences of a stroke?
Most often, the consequences are symptoms that could not be eliminated during treatment and rehabilitation. They depend on the size of the stroke and its location. In most cases, it is difficult to immediately predict the outcome of a stroke.
Are there any mental consequences?
Of course, they can be, and moreover, they often occur. A stroke is brain damage, you don’t even need to build logical chains here. For example, people with speech disorders sometimes become tense and overly active due to the fact that they are not understood and cannot express their thoughts. Unfortunately, sometimes people become inadequate.
What does recovery depend on?
Firstly, from the time of the patient’s presentation, from whether we were able to restore blood flow to the death of a large part of the brain. When a vessel is blocked by a thrombus (embolus), the area of the brain that is supplied only by this vessel dies in any case (without oxygen, the brain lives only 5-6 minutes) - this is the “stroke core”. The areas of the brain surrounding the “core”, which have adjacent blood supply not only from the damaged vessel, will experience oxygen starvation. And if we restore blood flow in time, they will return to their normal state and these areas of the brain will remain healthy.
Secondly, it depends on the diameter of the blocked vessel: the larger it is, the larger the stroke, the more severe the symptoms and treatment.
Only 30% of patients come to the “therapeutic window”, and half are patients with cerebral hemorrhage, who are treated completely differently, to whom thrombolysis is not applicable. Of these 30% in 2017, thrombolysis and (or) thromboextraction were used in only 4.2% of cases, that is, in every eighth. The rest are treated as usual, these modern methods are not applied to them: they arrive on time, but we find contraindications. In such cases, unfortunately, blood flow cannot be restored: people either die or remain disabled.
What should I do to fully recover?
Arrive at the hospital on time, undergo successful treatment and actively rehabilitate. Rehabilitation includes taking medications, physical therapy on the recommendation of a specialist, visiting a speech therapist, etc. By the way, the effectiveness of recovery is greatly enhanced by the support and help of loved ones. The attending physician will tell you and show you exactly how you can help; the main thing is to work with the sick person.
After a stroke, is it necessary to go to a psychotherapist?
Anything that needs treatment, any deviation in health, needs to be treated. If a person has developed disturbances after a stroke that have not gone away, there is no need to get used to them - this also applies to the psyche.
Is there a chance that the stroke will happen again?
Unfortunately, for those who have had a stroke, the risk of having another one increases many times over, especially in the first year. Further the risk decreases, but still remains high. According to various publications, recurrent stroke occurs in 30–50% of patients.
After treatment, it is imperative to follow secondary stroke prevention measures - this is taking medications, for many on a lifelong basis, qualitative lifestyle changes, and controlling the disease that led to the stroke.
What should I do to avoid having a stroke the first time?
To be healthy. But, unfortunately, over the years this does not work out, so primary prevention is the timely detection of chronic and other diseases that can lead to stroke. For this purpose, our country has a well-thought-out medical examination system: for each age, an examination plan has been developed that allows us to exclude diseases characteristic of it. It is free and accessible, the main thing is to get to the clinic, complete the prescribed examinations, and complete everything with examinations by the necessary specialists. There are many other dangerous diseases besides stroke, and they all need to be treated.
If there are no health problems, you need to eliminate smoking, alcohol abuse, start moving more and eat right.
What diseases cause stroke?
Diseases that occur in the vast majority of patients with stroke are arterial hypertension, cerebral atherosclerosis, heart rhythm disturbances, and diabetes mellitus. Smoking, drinking alcohol, being overweight, and having a sedentary lifestyle will all contribute to a stroke.
What most often triggers a stroke?
It is not always possible to say what caused a stroke. The body can adapt to changes for a long time, as long as they do not exceed the limit of its capabilities. An atherosclerotic plaque can grow for a long time, but sooner or later it blocks the vessel or, if it is unstable, breaks away from the wall and blocks it.
Most often, the “trigger” is a jump in blood pressure.
Does stroke depend on heredity?
If your grandmother had a stroke, it is not necessary that you will have one too. But there is a hereditary predisposition to chronic diseases that cause stroke. If your mom has hypertension, chances are you will have it too.
Does the disease depend on age?
Stroke occurs mainly in older people and those who have retired. But in recent years, there has been an increase in the proportion of patients of working age; modern diagnostic capabilities make it possible to more often detect this disease in young people.
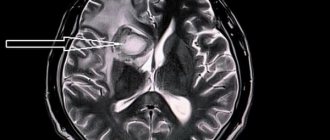
Diagnosis of stroke
Since the therapeutic window for the treatment of acute stroke is limited in time, it is extremely important to make a diagnosis as quickly as possible. Examination of the patient by a specialist and diagnostic tests (including neuroimaging) are carried out almost simultaneously. The choice of neuroimaging method is based on the neurological status and condition of the patient; for example, about 40% of patients with stroke cannot undergo MRI due to contraindications.
Clinical examination remains an important part of diagnosis. At this stage, anamnesis is collected, a general examination, and a neurological examination. Information about the time of onset of symptoms and previous stroke is especially important. A neurological examination is intended not only to establish stroke and its causes, but also to exclude diseases that imitate it, and to differentiate it from pathologies with a similar clinical picture.
For people suspected of having a stroke or TIA, emergency computed tomography (CT) or magnetic resonance imaging (MRI) of the brain is recommended.
Brain CT is today considered the international standard for diagnosing stroke; the accuracy of diagnosing hemorrhage with CT is almost 100%. Spiral CT reliably identifies most conditions simulating stroke (tumor, subdural hematoma, etc.) and distinguishes acute ischemic stroke from hemorrhagic.
MRI is more sensitive and can detect clear changes in the medulla, brainstem and cerebellum that are invisible with conventional CT. The procedure is especially effective in diagnosing stroke in the vertebrobasilar region, lacunar stroke, and acute ischemia. But MRI is less informative for hemorrhages.
Ultrasound methods help in diagnosing stenotic processes. Duplex scanning combines real-time ultrasound imaging to assess the anatomical structure of the arteries with pulsed Doppler analysis of blood flow at any part of the lumen of the vessel. This makes it possible to identify severe carotid artery stenosis at an early stage, for which catheterization angiography and surgery—carotid endarterectomy—are indicated.
Vascular imaging should also be performed as quickly as possible, including:
- CT angiography;
- MR angiography;
- catheter angiography;
- duplex ultrasonography.
Laboratory diagnostics should also be performed as an emergency; basic tests include:
- general clinical blood test with platelet count, hematocrit;
- determination of blood group, Rh factor;
- biochemical blood test: sugar, urea, creatinine, bilirubin, cholesterol, etc.;
- electrolytes (potassium, sodium);
- clinical urine analysis.
Other additional blood tests are possible as prescribed by your doctor.
Periods of rehabilitation after a stroke
Modern medicine recommends starting rehabilitation of a patient who has suffered a stroke in the first hours after the attack, as soon as hemodynamic parameters (heart rate, blood pressure) return to normal. This allows not only to restore lost functions as much as possible, but also to avoid various complications that can aggravate the patient’s condition.
The recovery period can be divided into several main stages:
- acute (first 3-4 weeks after the attack);
- early recovery (first 6 months after an attack);
- late recovery (from 6 months to a year);
- remote (more than a year).
Stroke treatment
Modern approaches to the treatment of stroke are based on the fastest possible hospitalization of the patient; neurologists never tire of repeating: time = life. There is a concept of the so-called “therapeutic window” - 4.5 hours from the onset of an ischemic stroke, during which therapeutic intervention helps the regeneration of damaged cells and the creation of new synaptic connections by neurons to replace the lost ones. The procedure of thrombolysis or systemic thrombolytic therapy (STLT) is highly effective - the administration of drugs that destroy the blood clot and help restore normal blood flow.
The Ministry of Health has approved unified clinical protocols developed on the principles of evidence-based medicine, taking into account modern international recommendations. According to such protocols, the patient must be hospitalized in specialized stroke departments of multidisciplinary medical institutions, intensive care or emergency departments, which have the ability to provide round-the-clock neuroimaging (CT/MRI), monitoring of vital functions, laboratory control and assistance by specially trained personnel.
To determine treatment tactics, it is necessary to determine the type of stroke. The choice of therapy will depend on this: thrombolysis, anticoagulants, regulation of general hemodynamics, treatment for atrial fibrillation. General therapy is aimed at restoring the functions of the nervous and cardiovascular systems, normalizing water and electrolyte balance, controlling the metabolism of blood plasma glucose and body temperature.
Surgical intervention
For large cerebral infarctions, covering more than half of the middle cerebral artery and accompanied by edema and dislocation of the brain, conservative treatment methods are ineffective, and the mortality rate reaches 80%. In such cases, in order to avoid a critical increase in intracranial pressure, wide decompression craniotomy is used - hemicraniectomy. This can significantly reduce mortality and improve treatment results.
One of the most promising methods for treating acute ischemia has become endovascular interventions, when the operation is performed under X-ray or angiographic control. Several specific techniques have been developed: emergency angioplasty with stenting, mechanical destruction and/or removal of a blood clot - thrombectomy. The use of endovascular operations is limited to highly specialized centers where there are the necessary technical resources and qualified specialists - only under such conditions are these interventions safe.
You need to understand that the effectiveness of treatment depends on the area of brain damage and which areas were damaged. The treatment process is long and requires a lot of patience and effort, primarily from the patient himself and his loved ones. Proper rehabilitation after a stroke is extremely important to maximize the restoration of body functions and return the patient to as normal a lifestyle as possible.
Which doctors treat stroke?
Most patients with ischemic or hemorrhagic stroke are subject to urgent hospitalization in a specialized neurovascular (stroke) department or center, or, in the absence of one, in a neurological department. In case of violation of vital functions, they are hospitalized in the intensive care unit, in case of epi-, sub-, intracerebral hematomas - in neurosurgery.
The leading doctors in the treatment will be neurologists, neurosurgeons and neurovascular specialists. In addition to them, doctors of instrumental and laboratory diagnostics, cardiologists, ophthalmologists, psychologists, speech therapists, endocrinologists, rehabilitation specialists and physiotherapists, and other specialists take part in the treatment process.
Cost of initial appointment, research, treatment
It is advisable to talk about the price of the initial appointment during a preventive examination, when there is no stroke as such, but the person has pathologies that increase the risk of its development. The cost of diagnostic procedures for stroke can be found in the corresponding table, but it must be taken into account that many studies are used repeatedly to monitor the treatment process.
It is quite difficult to determine even the approximate cost of stroke treatment in Moscow. Much depends on the type of stroke, the extent of brain damage, the patient's condition, the timeliness of medical care and other important factors. In any case, the cost of medical services will be justified - after all, we are talking about preserving life.
Treatment of patients in specialized stroke departments, cardiology centers - stroke units (IB) - reduces mortality and disability by 20%, reduces financial costs at all stages of treatment.
Possible consequences
A stroke can result in temporary disability, disability, or even death. Only 20% of people who have had this disease can fully return to work. Every year in Russia, stroke occurs in about 450,000 people. According to statistics of recorded deaths from stroke, this cause ranks second among all deaths in our country. The most common consequences of the disease include:
- impaired movement, weakness in the limbs, numbness of various parts of the body;
- memory, speech, and urination disorders;
- loss of ability to care for oneself independently.
Advantages of treatment at the clinic of JSC "Medicine"
On the basis of a multidisciplinary medical center (academician Roitberg’s clinic) there is a cardiac rehabilitation center specially created for the treatment of strokes. How does IB differ from a regular neurological or therapeutic department:
- specializes in the treatment of patients with stroke, its staff is trained to care for this group of patients;
- the necessary diagnostic facilities - from computer and magnetic resonance imaging scanners to a laboratory with round-the-clock operation, an intensive care unit;
- work according to local protocols developed on the basis of domestic and international principles of stroke treatment;
- early mobilization and intensive rehabilitation.
multidisciplinary team:
- vascular neurologists;
- nurses are trained to care for stroke patients;
- rehabilitators who help restore physical capabilities and self-care skills;
- speech therapists – restore the ability to oral and written communication, correct swallowing disorders;
- neuropsychologists - working to restore cognitive functions.
In addition, in the cardiac rehabilitation center there is a constant opportunity to consult with doctors of various specialties: cardiologist, neurosurgeon, psychiatrist, urologist, endocrinologist, etc. In developed countries, hospitalization in stroke units has become the “gold standard”. In the UK and Germany, 9 out of 10 patients with stroke are treated in an IB, in Poland - 8 out of 10.
Rehabilitation after stroke in the early recovery period
The early recovery stage is crucial for the patient and should ideally take place in a sanatorium or rehabilitation center. When deciding to leave the victim at home, you should remember that successful recovery after a stroke is impossible without the active participation of specialized specialists who will have to be invited to the home.
The first three months after the onset of the disease are especially productive and favorable for rehabilitation. At this stage, they move from the simplest exercises to more complex ones - they teach a person to roll over, rise, sit down, and stand up independently. Next, elements of active physical therapy are gradually introduced, physiotherapy, massage, speech work are continued, and complexes are performed to restore vision and eye movements, cognitive functions (memory, thinking, attention).
A common consequence of a stroke is complete or partial loss of vision, dysfunction of the eyelid, presbyopia, when a person cannot distinguish small print or small objects at close range. All these disorders require qualified assistance from an ophthalmologist, who will prescribe either medication or surgical treatment. In mild cases, they can do with therapeutic exercises for the eyes.
To restore attention, memory, and intellectual abilities, there are many exercises: memorization tasks, memorizing poetry, solving riddles, rebuses, putting together puzzles, chess, checkers. However, for complete rehabilitation of cognitive functions, psychological and correctional classes are necessary individually or in groups. Additional stimulation is provided by medications that should be prescribed by a doctor.