Most people measure their blood pressure on one arm. But this is not entirely true. Quite often, the indicators differ on different hands, which can be considered both the norm and a pathology indicating the presence of diseases.
In the literature you can find references to the fact that nearly half of people who have a well-defined difference in pressure in different extremities (more than 20 millimeters of mercury) die within 10 years. Having become familiar with such information, people whose blood pressure levels are normal panic and begin self-medicating a non-existent disease. In reality, only 15-20% of cases of pressure differences in the arms require treatment.
First of all, you should see a therapist. After studying the medical history and preliminary examination, the doctor will determine the cause and select the optimal treatment to eliminate it. If necessary, he will refer the patient for a consultation with a vascular surgeon, cardiologist or neurologist. Accurate diagnosis and adequate therapy will not only return blood pressure to normal, but will also prevent the development of severe complications.
Normal or disease: how to find out?
If, when measuring blood pressure, you find differences between the results on your left and right arms, then analyze the facts indicated in the table.
| Factor | Impact factor |
| Magnitude of difference | A small range (up to 10 millimeters of mercury) is considered acceptable. The larger the range, the higher the likelihood of pathology |
| Increase or decrease in pressure | If the pressure on one arm is normal or increased, and on the other it is higher, then such a situation poses less of a danger than the pressure meeting the norm on one arm and decreasing on the other. |
| Age | More often there is a difference in pressure on the left and right hands in adolescents and older people |
| Left-handed or right-handed | The norm is an increase in pressure on the main working hand |
| Physical activity or sports | The difference may be a result of increased physical activity |
| Presence of complaints and unpleasant symptoms | If they are present, the pressure difference is a consequence of the disease |
For those who measure blood pressure very rarely, it is recommended to perform tonometry on both arms. Those who take measurements every day need to determine the left and right indicators at least monthly.
On which hand does the pressure increase?
An increase in pressure on one arm is not as dangerous as a decrease in pressure if the values on the other arm are within the normal range or slightly higher.
In right-handed people who lead a sedentary lifestyle, the pressure in the right hand may be lower than in the left. Left-handers involved in sports or physical work show similar indicators. In addition, the difference can increase and amount to close to 20 millimeters of mercury. There is a completely reasonable explanation for this situation. The subclavian arteries carry blood to the arms: the left one comes from the aorta, therefore, the pressure in it is quite high, and the right one comes from the brachiocephalic trunk, the pressure in which is much lower.
If a right-handed person is constantly exposed to increased physical activity, then the pressure on the right hand may be higher, but it should not go beyond acceptable limits. This is due to the fact that with systematic training, the muscles of the right shoulder girdle become denser and increase in volume. As a result, the arteries supplying the right arm are compressed, which leads to increased blood pressure.
Dear patients!
Introduction to the problem
Data from numerous studies convincingly show: a difference in pressure of more than 10 mm Hg. Art. between the right and left arms may be a marker of vascular disease of the extremities. With a stable systematic difference of 15 mmHg. Art. and higher, the probability of having significant damage to the cerebral vessels, and therefore the risk of stroke, increases by 1.5 times, and the probability of death from cardiovascular diseases - by 70%.
The difference in pressure on the right and left hands can make itself felt by discomfort, weakness, dizziness, tinnitus, decreased reaction, weakness in the hand, rapid fatigue when performing physical activity, and chilly fingers. But sometimes the pressure difference does not manifest itself in any way, and it can only be detected by regularly measuring the pressure on both hands. At the same time, patients who do not suffer from high blood pressure may have different pressures in different arms.
But, in practice, pressure on both arms is measured extremely rarely, even in medical institutions.
Causes of pressure difference
If you notice a difference in pressure in your hands, you shouldn’t panic right away: a difference in pressure is a symptom of many conditions, both serious and not so serious, including, for example, different tone of the hands. With the help of additional examination, you can understand what causes the difference.
The results of measuring pressure on different hands may differ due to a number of reasons:
1. Excitement. When our blood pressure is taken, we may be a little worried. Then we calm down, and the indicator on the second hand can return to normal. 2. Anatomical features. For many people, blood pressure measured on the right arm will be higher than on the left. This is especially true for those who often work physically. Sometimes fibrosis can develop in the muscles of the shoulder girdle. It causes compaction and thickening of the legs of the left scalene muscle. In this regard, the neurovascular bundle, which runs on the left side of the body, may be infringed. 3. More developed muscles on one of the arms. 4. Impaired blood circulation, including due to atherosclerosis.
Risks associated with pressure differences
As mentioned above, if the difference when measuring pressure on the hands does not exceed 5-10 mm, there is no reason to worry. If the indicators differ by 15-20 mm or more, then this is a reason for examination. For example, for young people this may mean the presence of vascular abnormalities, for middle-aged and elderly people - most often atherosclerosis. Coronary heart disease, cerebrovascular accident, hypertension, intermittent claudication (muscle pain when walking) - this is what vascular atherosclerosis often leads to.
The difference is more than 20 mmHg. Art. between the results obtained on the right and left arm may indicate atherosclerotic narrowing or occlusion of the subclavian artery. And this pathology already significantly increases the risk of stroke.
Response measures
A timely detected deviation from the norm will help to make a timely diagnosis and take the necessary measures for effective treatment, and in some situations will help prevent a stroke or heart attack. The difference in pressure between the right and left hands makes it possible to identify atherosclerosis in the early stages, which speeds up the start of treatment and increases its effectiveness. We should not forget that atherosclerosis in the early stages, regardless of the target organ, often occurs without noticeable symptoms.
Early diagnosis of pressure differences can be an additional reason to quit smoking, change your lifestyle, and take medications prescribed by your doctor.
Diagnosis of stenosis of the subclavian arteries
To find out whether you have stenotic artery lesions or not, your doctor will examine you. Even if you have no symptoms, your doctor may listen for a murmur over the carotid or subclavian arteries caused by blood flowing through the stenotic area. If necessary, first of all, a duplex ultrasound scan of the main arteries of the head and the initial parts of the upper extremities (US-DS) will be prescribed. It allows you to determine the localization of the narrowing, its degree and significance.
For a more detailed assessment of the condition of the arteries, your doctor may recommend angiography (X-ray examination of blood vessels). This study is performed by catheterization, usually of the femoral or wrist artery, under local anesthesia in a special operating room equipped with an angiography unit.
Treatment of stenosis of the subclavian arteries
For those cases when stenotic lesions of the arteries are diagnosed and it is no longer possible to do without surgery, there are two methods of surgical treatment. The first is open bypass surgery performed by vascular surgeons. The second is a modern, low-traumatic, X-ray surgical operation - stenting, performed by X-ray endovascular surgeons (under local anesthesia through a puncture). Both methods have their indications and contraindications. Therefore, the question of choosing one of them is always decided individually.
Clinical cases
Clinical case No. 1
A patient complains of dizziness, lack of pulse in the left arm, periodic spasms in the shoulder, weakness in the left arm during physical activity, paresthesia in the fingers, hand and forearm. The angiogram shows severe (up to 90%) stenosis of the left subclavian artery in the initial segment.
A balloon-expandable stent is installed into the area of stenosis under local anesthesia through a femoral approach (puncture on the thigh) (see before and after photos below).
The stenosis (and the associated pressure difference across the arms) is completely eliminated.
The patient's well-being improved significantly.
Clinical case No. 2
A patient complains of weakness in the left hand, worsening with minimal physical activity, chilliness of the fingers of the left hand, episodes of dizziness, and headaches. At the time of measurement before angiography, the pressure on the right arm was 190/100, on the left – 110/75. The difference in systolic pressure between the arms is 80 mm! The angiogram shows occlusion (blockage) of the left subclavian artery in the initial segment (Fig. 1 - angiography from the aorta, Fig. 2 - angiography from the left arm). Due to complete blockage of the subclavian artery, the blood supply to the left arm was carried out according to an emergency scheme, bypassing through the brain - along the vertebral artery, that is, the brain was stolen.
With the help of special instruments, to minimize the risks of intervention using only local anesthesia and access only through the vessels of the upper extremities (!), it was possible to pass through the blocked area, expand it and install a balloon-expandable stent (Fig. 3).
Adequate blood flow through the subclavian artery (and therefore the blood supply to the left arm and brain through it) was completely restored. By restoring the physiological direction of blood flow, brain stealing was eliminated. During the control pressure measurement, there is no longer any pressure difference between the hands.
The patient's health improved significantly.
Clinical case No. 3
A similar case. A patient complains of weakness in the left hand, which worsens with physical activity, chilliness of the fingers of the left hand, episodes of dizziness, and headaches. The difference in systolic pressure between the arms is 40 mm. The angiogram shows subocclusion (critical stenosis) of the left subclavian artery in the initial segment (Fig. 1 - angiography before intervention). Due to complete blockage of the subclavian artery, the blood supply to the left arm was carried out according to an emergency scheme, bypassing through the brain - along the vertebral artery, that is, the brain was stolen.
Using special instruments to minimize the risks of intervention, using only local anesthesia and access only through the radial artery (at the wrist) of the right upper limb, it was possible to pass through the blocked area, widen it and install a self-expanding stent.
Adequate blood flow through the subclavian artery (and therefore the blood supply to the left arm and brain through it) was completely restored. By restoring the physiological direction of blood flow, brain stealing was eliminated. With a control pressure measurement, there is no longer a difference in pressure between the hands.
The patient's well-being improved significantly.
The presented clinical cases are the result of examination and successful treatment of patients at the Medservice MC, by specialists with extensive experience in this area using the most modern angiographic complex Philips Allura Xper FD20 (Netherlands). This device with a new digital image processing system has a unique technology for suppressing noise and artifacts, which makes it possible to significantly increase image clarity without increasing radiation exposure and to see the thinnest vascular structures and stents. The latest generation X-ray tube minimizes radiation exposure to the patient.
You can ask questions related to angiographic and X-ray endovascular interventions at Medservice LLC: Tel. Email mail Ivanov Andrey Gennadievich (Head of the Department of X-ray Surgical Methods of Diagnostics and Treatment, doctor of the highest category in the specialty “X-ray endovascular diagnostics and treatment”)
Why does asymmetry appear?
Some causes of pathology can be approximately determined using a table. But only a specialist can make the correct diagnosis and prescribe adequate treatment.
| Problem | Possible reason |
| On one hand (it doesn’t matter which one) the pressure is normal, but on the other it is higher than normal. | Individual characteristics of the structure of arteries, vegetative-vascular dystonia |
| There is increased pressure on one hand, and even higher on the other | Hypertension, vegetative-vascular dystonia, stress, frequent worries, constant lack of sleep |
| On one arm the pressure is below normal, and on the other it is normal or high | Impairment of the patency of the arteries providing blood supply to the arm |
The patency of the arteries is impaired when they are compressed or the lumen is blocked.
The following diseases can provoke a similar problem:
- Atherosclerosis – cholesterol is deposited on the inner lining of blood vessels and atherosclerotic plaques are formed, closing the lumen.
- Thrombosis and thromboembolism – blood clots (thrombi) form inside the vessels, obstructing the movement of blood.
- Aneurysm - a dilation forms on the blood vessels, which has a sac-like shape.
- Aortoarteritis - the walls of blood vessels become inflamed, which leads to thickening of their membranes.
- Scalenus syndrome - muscle fibers located around the subclavian artery become very dense and compress the artery.
- Benign and malignant tumors that form in the bone or soft tissue of the shoulder or chest.
- Injury.
- Surgical intervention performed on blood vessels.
Bian-Qiao
The Eastern school of pulse diagnostics is associated with the name of the legendary Chinese physician Bian Qiao, who lived in the 6th century BC. According to legend, one day Bian Qiao was invited to the house of a mandarin whose daughter was ill. Diagnosis and treatment were complicated by the fact that the noble girl could not be touched. Bian Qiao found a way out of the situation. He asked to tie a long cord to the patient’s arm and give him the other end. The mandarin's servants decided to play a prank on the doctor and tied a cord to the dog's paw. Bian Qiao immediately said that the vibrations he felt were not the vibrations of a person, but of an animal, moreover, sick with worms. Realizing that it was difficult to deceive the doctor, the servants tied a cord to the hand of the mandarin’s daughter, and Bian Qiao immediately made a diagnosis from the pulsation of the rope.
Clinical manifestations of pathology
The main reason for low blood pressure in one arm is impaired blood circulation due to blockage of blood vessels.
In this case, the pathology is accompanied by the following symptoms:
- the strength of the hand is weakened;
- the fingers turn pale and cold, there is numbness;
- the skin on the fingertips, and often on the entire hand, may acquire a bluish tint.
When the pressure on the right hand decreases, in addition to the above signs, symptoms appear indicating a circulatory disorder in the brain:
- headache and dizziness;
- nausea and vomiting;
- speech difficulties;
- weakening of memory and absent-mindedness;
- facial distortion;
- paralysis of one side of the body.
This situation is due to the fact that the arteries supplying the right arm and brain with nutrients and oxygen depart from the aorta in one trunk.
Pulsation of the world and man
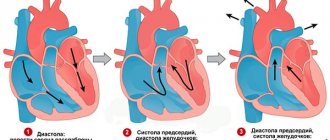
Diagnosing health by pulse is the oldest method of health monitoring. Research on the relationship between pulse activity and human condition was carried out both in the East and in the West. The very first full-fledged work on pulse diagnostics known to Western civilization is the treatise by the Alexandrian physician of the Ptolemaic dynasty Herophilus of Chalcedon “Peri sphigmon pragmateias”. Herophilus believed that one could determine the state of health by the pulse, as well as “foresee the future.” The doctor compared different types of pulse with musical rhythms and introduced the concepts of systole and diastole. These terms, as well as the concept of “jumping pulse”, have been preserved in modern medicine. All famous physicians of antiquity, from Galen to Paracelsus, practiced pulse diagnostics. The very ancient perception of the world as a macrocosm, and man as a microcosm (the alchemical principle of similarity) indicated that rhythmic pulsations are one of the key principles of the world order, and therefore they should be studied in detail.
Therapy methods
Treatment for pressure differences may include:
- taking medications that thin the blood and restore vascular patency, which helps improve blood circulation (the doctor selects medications in accordance with the disease that caused the problem);
- physical therapy that activates blood circulation;
- physiotherapeutic procedures.
If conservative treatment does not give the desired result, then the attending physician recommends surgery, during which blood clots and atherosclerotic plaques are removed, stents are installed on the vessels, or damaged arteries are replaced with prostheses.
If you contact a specialist in a timely manner, you will be able to not only find the cause of the problem, but also completely get rid of the disease.
Pulse rate
The normal pulse rate according to the WHO classification is 60-80 beats per second, although the very concept of “normal pulse” is, by and large, no more than a figure of speech, since each person’s pulse is individual. Moreover, the concept of normal may vary not only depending on the physiological state of a person, but also on the time of day. At night, the pulse can reach 38 beats per minute, which is a critically low point for daytime, after which activation of cardiac activity by a pacemaker is prescribed. In women, the pulse beats 6-8 beats faster than in men; during exercise, the pulse can reach up to 250 beats per minute. So, Kostya Tszyu’s pulse during training was 240 beats per minute, which was quite normal for him.