Painful periods darken life and disrupt the usual rhythm of most women. Many of them have resigned themselves and perceive this as an inevitable condition during PMS. Is this so and is it worth sounding the alarm if your stomach hurts severely during menstruation? Gynecologists say that pain during menstruation is not normal!
What is dysmenorrhea: is pain during menstruation normal?
The content of the article
It is not for nothing that menstruation is called critical days, since at this time the fair sex experiences a whole range of unpleasant feelings. One of the most common associations associated with periods is pain.
For some reason, it is believed that painful menstruation is the norm, which is actually a misconception. Any pain, including menstrual pain, requires mandatory diagnosis and treatment, which will significantly make a woman’s life easier and restore her productivity and self-confidence.
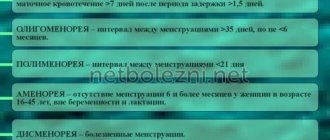
In medicine, pain during menstruation is considered a disease and has an independent diagnosis. A patient who comes with this problem is diagnosed with dysmenorrhea (algomenorrhea). Dysmenorrhea is one of the most common gynecological disorders.
Dysmenorrhea has different causes, most often it is inflammation of the reproductive organs and hormonal diseases, which means that after undergoing examination and treatment, you can forget about the problem forever.
How should normal periods proceed?
Menstrual pain can be a natural ailment or indicate the presence of a serious pathology.
The normal state of a woman during menstruation is characterized by mild pain or minor discomfort. Light, nagging, short-term pain indicates contractions of the uterus, getting rid of the “outdated” inner layer of the mucosa - the endometrium. A new endometrium is formed every month - during pregnancy it will serve as a bed for a fertilized egg.
If a woman regularly suffers from unbearable, severe pain, accompanied by dizziness, nausea, fainting and other symptoms that impair performance, then the disease is dysmenorrhea (algomenorrhea, algomenorrhea). This condition indicates various disorders in the hormonal, vascular, nervous or other system of the woman’s body.
Manifestations of premenstrual syndrome
Almost all women are familiar with the feeling of premenstrual syndrome. But it manifests itself differently in everyone. In general, experts identify more than 100 symptoms. Hormonal changes in a woman’s body before menstruation entail a lot of consequences. Literally every internal organ, all vital systems find themselves in a stressful situation. The nervous system, the vegetative-vascular system, is under particular stress. The heart is an organ that finds itself at the very center of internal changes. In addition, pain in the left hypochondrium may indicate neuralgia, which has nothing to do with heart disease.
Types of dysmenorrhea
This disease can be primary, when there is no extraneous physical cause of pain, and secondary, caused by any concomitant disease.
- Primary (functional) dysmenorrhea.
Primary dysmenorrhea most often affects girls and young women under the age of 25, and with the onset of sexual activity and the birth of their first child, this pathology disappears in half of them. It is believed that this is due to the normalization of hormonal levels. The disease is most severe in girls with a late onset of menarche (first menstruation) and smokers. Primary dysmenorrhea can also be hereditary. - Secondary (organic) algomenorrhea
is the result of gynecological and internal pathologies. It occurs regardless of age, but is more common in patients over 30 years of age who have given birth.
Primary dysmenorrhea can be of two types:
- essential – occurs due to a low pain threshold;
- psychogenic – caused by fear of waiting for menstruation.
Based on the intensity of pain, the pathology is:
- compensated – symptoms and their intensity do not change from year to year;
- decompensated - the pain of menstruation and the severity of symptoms increases over time.
Dysmenorrhea is also classified according to severity:
- Mild (1st degree) – moderate, short-term painful menstruation, not leading to loss of ability to work;
- Moderate (2nd degree) – a slight decrease in working capacity, pain in the lower abdomen is complemented by a number of symptoms (weakness, nausea, chills, frequent urination, psycho-emotional instability);
- Severe (3rd degree) – complete loss of ability to work, intense unbearable pain in the lower abdomen and lower back, complemented by moderate symptoms and significant neurovegetative and metabolic-endocrine disorders (loss of consciousness, vomiting, heart pain, etc.).
Moderate and severe degrees of algomenorrhea occur in every tenth patient.
Symptoms of dysmenorrhea
Dysmenorrhea pain begins in the lower abdomen before or along with menstruation. They have a cramping nature with impact in the back, groin and anus. Women complain of fatigue, diarrhea, headache, nervousness, dizziness, fainting, nausea and vomiting. Some people experience the whole range of symptoms, while others are only bothered by pain.
The pain lasts from several hours to 2-3 days. During the break between critical days, the woman does not feel any unpleasant symptoms. During vaginal and rectovaginal examination in patients suffering from primary dysmenorrhea, as a rule, no pathology is detected.
Pain during menstruation and accompanying symptoms can be of varying degrees of severity depending on the type of pathology. Alarming symptoms requiring special attention:
- Pain syndrome
: severe pain in the lower abdomen of a pulling, stabbing or cramping nature, occurring 1-2 days before menstruation and radiating to the rectum, appendage area, bladder, lumbar region, inner thighs. - Emotional and mental disorders
: sleep disturbance, irritability, nervousness, excessive sensitivity, anxiety, emotional depression, anorexia, bulimia, odor intolerance, taste perversion. - Autonomic disorders
: nausea, belching, hiccups, chills, fever, increased sweating, dry mouth, frequent urination, bloating, diarrhea alternating with constipation. - Vegetative-vascular manifestations
: loss of consciousness, dizziness, headache, arrhythmia, tachycardia, bradycardia, heart pain, numbness of the extremities, swelling of the face. - Metabolic and endocrine disorders
: increased or decreased temperature, weakness, loss of strength, vomiting, feeling of “woolly” legs, itchy skin, joint pain, swelling.
How to relieve a symptom
In the absence of organ diseases, you can cope with painful sensations on your own. Physical exercise, proper breathing, and sedatives will help with this. To remove pain, it is necessary to eliminate the cause. In this case, it is only possible to reduce the negative manifestations of PMS.
- When the heart hurts, there is dizziness and weakness. In some cases, all this ends in loss of consciousness. During the period of unpleasant sensations in the left side of the hypochondrium, it is recommended to drink Valocordin, Validol. The drugs have a sedative effect and help relax blood vessels. Better blood circulation.
- As soon as an organ begins to hurt in attacks, you need to sit or lie down, relax, and breathe deeply. Deep but calm breathing normalizes the functioning of the organ, and the heart will stop hurting.
- Shortly before the start of menstruation, it is necessary to introduce iron-rich foods into the diet. Then the risk of a decrease in hemoglobin will decrease. The most affordable products are apples, liver, meat, buckwheat porridge.
- Raise blood pressure with green tea, chocolate, and red wine. You can take a tablet of citramon, citropak, or any drug containing caffeine. As well as a complex of vitamins containing iron.
- If your heart hurts, you should take sedatives in the form of tinctures of motherwort, valerian, and glod. You can make a “cocktail” of these drugs. Mix 10 drops of each, wash down with water, tea, juice. Tea made from chamomile, lemon balm, and mint has a beneficial effect on the nervous system.
It is imperative to adhere to a sleep and rest schedule. Go for walks and light jogging. Spend more time outdoors. Then your heart will stop hurting and other manifestations of premenstrual syndrome will decrease.
Causes of primary dysmenorrhea
Causes of primary dysmenorrhea:
- Physiological – disruption of hormone synthesis. There is an increased production of prostaglandins - substances responsible for uterine contractions during PMS. Their excess quantity leads to strong uterine contractions and, accordingly, to the occurrence of pain. Also, discomfort is caused by increased production of adrenaline, norepinephrine, dopamine and serotonin.
- Psychological – the patient’s fear of menstruation and neurological disorders. A reduced pain threshold, psycho-emotional instability and other neurological disorders exacerbate the perception of pain;
- Magnesium deficiency in the blood;
- Congenital anomalies of connective tissue development;
- Vascular disorders;
- Atypical position of the uterus, its underdevelopment and malformations.
Primary dysmenorrhea occurs:
- Adrenergic
, in which the level of adrenaline, norepinephrine and dopamine - special hormones that can affect a woman’s well-being - increases in the body during critical days. As a result, various functions of the body are disrupted, causing, along with the main signs of the disease, changes in skin color and heartbeat. Due to impaired blood circulation, the skin of the face turns pale, the hands and feet become cold and acquire a bluish tint. - Parasympathetic
, characterized by hypersecretion of serotonin, another important hormone. The general symptoms characteristic of this disease include swelling, sweating, weight gain on the eve of critical days, associated with fluid retention in the tissues.
Causes of secondary dysmenorrhea
The occurrence of secondary dysmenorrhea can be caused by the following reasons:
- inflammatory processes in the organs of the reproductive system, endometriosis;
- varicose veins of the pelvic veins;
- adhesions in the pelvis and fallopian tubes caused by adnexitis (inflammation of the tubes, ovaries) or operations in the past;
- uterine fibroids, ovarian cysts, adenomyosis;
- sexually transmitted infections;
- dysplastic pathologies, oncological diseases;
- fluctuations in hormone concentrations;
- installation of an intrauterine device (promotes enhanced synthesis of prostaglandins);
- abnormalities in the development of the genital organs, complicating the outflow of menstrual blood;
- injury, consequence of surgery, frequent medical abortions;
- psychological and physical fatigue, constant stress, violation of rest and work schedules.
In women over 40 years of age, algomenorrhea is often a symptom of metabolic disorders and diseases of the cardiovascular system. Painful periods often occur after the introduction of intrauterine contraceptives. This is caused by an exacerbation of existing gynecological pathologies due to the use of an IUD.
Painful periods - what to do?
Menstruation accompanies women throughout the reproductive period. For several days in each cycle, women experience some discomfort and malaise. Unfortunately, the severity of discomfort varies quite widely: from moderate tugging sensations in the lower abdomen to severe pain, forcing significant adjustments to the usual lifestyle.
Painful menstruation, of course, is far from the norm. Moreover, this condition is well studied and is reflected in the International Classification of Diseases as dysmenorrhea.
Dysmenorrhea can be primary or secondary. In order to understand what the patient is faced with, doctors begin a diagnostic search. If the cause could not be found, and menstruation became painful in youth, we need to think about the primary
, or
idiopathic dysmenorrhea
.
Secondary dysmenorrhea
- this is when pain during menstruation is a symptom of a disease: inflammation, cyst, endometriosis, abnormal development of the genital organs, etc. Treatment of secondary dysmenorrhea is the treatment of the disease for which menstrual pain is a symptom. For endometriosis, for example, long-term hormone therapy will be carried out. For abnormalities in the development of the genital organs, surgical treatment options will be considered.
Treatment of dysmenorrhea
Helping patients with primary dysmenorrhea is very simple - just choose the right NSAID (non-steroidal anti-inflammatory drug): indomethacin, ibuprofen, ketoprofen, celecoxib, etc. In most cases, one tablet is enough to completely relieve pain in the current cycle. For severe pain and regular menstruation, you can start taking NSAIDs 2-3 days before menstruation.
- What kind of treatment is this? They're just painkillers. - Not really. NSAIDs suppress the synthesis of prostaglandins, so they act not only symptomatically (simply relieve pain), but also pathogenetically (affect the mechanism of pain development in primary dysmenorrhea).
If you take NSAIDs in each cycle for primary dysmenorrhea, the severity of pain decreases from cycle to cycle.
It is very easy to help patients who are sexually active and not planning a pregnancy. The ideal way to get rid of menstrual pain would be COCs (combined oral contraceptives). It is not without reason that among the non-contraceptive advantages of COCs, the elimination of dysmenorrhea and other menstrual irregularities comes first.
Rarely, but still there are patients who do not respond well to NSAIDs and COCs. In this case, a combined method is used: COC + NSAIDs.
Treatment errors
Despite the obvious simplicity of the situation, there is a whole bunch of myths, misconceptions and nonsense surrounding painful menstruation.
Most patients with painful menstruation do not seek medical help, probably not considering such pain as a sign of illness. Mothers who suffered from dysmenorrhea in their youth boldly transfer their experience to their daughters: “It will go away when you give birth to a baby.” With moderately severe symptoms, our women prefer to “drink something” or lie down. Unfortunately, this “something” is most often no-shpa.
— I don’t understand why 80% of my patients take no-shpa for menstrual pain. - Well, they say on TV that no-spa helps. - Where do they say? Who's speaking? - Well, they are playing an advertisement where a bride is standing in a white dress, and her mother is giving her no-shpu. — Why do you think that the bride is menstruating???
No-shpu really accepts a huge number of women. Some were advised by their mother, others by a friend, others by a gynecologist. She doesn't help much. Actually, he has the right not to help at all, because menstrual pain is almost unrelated to spasm. Although in case of severe dysmenorrhea, no-spa may be recommended and appropriate as part of combination therapy.
The most curious thing is that the majority of patients who prefer “no-shpu and lie down”, as a rule, have had successful experience in taking NSAIDs, but continue to use not very effective drugs, fearing regular use of “too strong” or “too harmful” pills. NSAIDs, of course, have a damaging effect on the stomach wall with long-term regular use. Although application once every 24–30 days can be called regular, serious additional damaging factors are required for the formation of a peptic ulcer. If the patient already has a stomach disease, you can offer drugs containing celecoxib - they are most gentle on the gastrointestinal mucosa.
A special case
Sometimes we come across girls suffering from severe menstrual pain. Pain gradually turns an enthusiastic and carefree young lady into a person with rapidly declining self-esteem.
- What's wrong with you? Get your act together! Why can't you "cope" with your regular periods? - reproach peers. “We don’t understand what happened to her.” “She’s not the same carefree girl anymore,” the parents are perplexed. “Perhaps she just doesn’t want to go to school?”
Regular sanitary tampons can increase pain. Medicines help little or not at all. Girls skip school, refuse to go to the pool and participate in sports events, and it becomes increasingly difficult for them to maintain relationships with friends.
The pain can be so severe that you have to call an ambulance. Doctors rule out acute appendicitis, pregnancy and recommend screening for sexually transmitted diseases, ultrasound and computed tomography. Such an experience leaves an extremely negative aftertaste. For some young patients, such active intervention is not much different from physical violence. When even after all the above, no answers are received except that the girl does not have any of the above-mentioned conditions, she is advised to take some kind of painkiller.
But if:
- cyclical pain lasts more than 6 months;
- the patient is bothered by severe pain, and upon examination the doctor finds no (or almost no) signs of the disease;
- treatment helps poorly, hardly helps or does not help with a second course of therapy,
endometriosis and associated secondary dysmenorrhea can be suspected.
Unfortunately, in order to diagnose endometriosis in women, it is necessary to undergo a diagnostic laparoscopy.
Alas, not every representative of the fairer sex is ready to decide on surgery for diagnostic purposes. Just imagine how difficult it is to explain to the parents of a young girl that their daughter needs surgery to make sure that her menstrual pain is not related to endometriosis.
World Endometriosis Society expert Professor Robert Albee in his article calls on all humanity: “Please believe young women when they say they are in pain!”
The idea that the young woman is pretending, exaggerating her suffering, occurs not only to her relatives, but also to her attending physicians. This is a very dangerous misconception. There is nothing more offensive to a suffering person than the mistrust of people from whom he expects help.
Oksana Bogdashevskaya
Photo thinkstockphotos.com
Products by topic: [product](indomethacin), [product](ibuprofen), [product](ketoprofen), [product](celecoxib), [product](drotaverine), [product](no-spa)
Diagnostics
Before starting treatment, the woman or girl is carefully examined to find out the cause of painful periods. This makes it possible to distinguish the primary form of the disease from the secondary one.
The gynecologist conducts an examination based on complaints and clinical manifestations, always taking into account the age, life history and illness of the patient.
- Initially, the gynecologist performs a gynecological examination and palpation of the mammary glands.
- Further, the diagnosis continues with the appointment of clinical minimum tests - general and biochemical blood tests. With their help, it is possible to identify signs of inflammation and anemia (signals about an inflammatory process, endometriosis or intra-abdominal bleeding).
- Laboratory tests of vaginal smears and hormonal status are carried out.
Then an instrumental examination is carried out, including:
- vulvoscopy and colposcopy to identify abnormalities of the vagina, inflammatory diseases and pathologies of the cervix.
- Ultrasound of the pelvic organs to detect adhesions, tumor formations, inflammatory processes in the uterus and appendages, genital endometriosis.
In some cases, hysteroscopy, laparoscopy, diagnostic curettage of the walls of the uterine cavity, MRI, and CT may be prescribed. If there are complaints of headache, encephalography is performed to exclude other causes. Additionally, you may need to consult an endocrinologist, oncologist and surgeon.
Treatment of painful periods: is it necessary to go to a gynecologist?
The goal of treating dysmenorrhea is to identify the cause of the disease, eliminate it and eliminate pain. The gynecologist prescribes therapy based on the form of dysmenorrhea, the nature of the pain syndrome, its cause and the individual characteristics of the patient.
Most women “treat” menstrual pain with medications that relieve pain. At the same time, they believe that such a decision is the best way to avoid visiting a doctor. In fact, dysmenorrhea can be a symptom of a serious gynecological disease.
By temporarily eliminating the pain, you will not get rid of the cause that gives rise to it, so visiting a gynecologist is only a matter of time. This is especially true for secondary dysmenorrhea that occurs after normal menstruation. This pathology often occurs as a result of inflammation of one of the organs of the reproductive system.
What to do if you have chest discomfort during menstrual periods
The occurrence of intense pain in the heart area during any phase of the menstrual cycle is an alarming symptom that requires emergency medical attention.
If cardiac pain appears in the first phase of the menstrual cycle (the first 15 days after menstruation), the development of coronary heart disease is excluded. The most common provoking factor for angina pectoris (one of the forms of coronary artery disease) is physical activity. Cardialgia against the background of hormonal changes is caused by:
- emotional turmoil;
- acute stress factors;
- smoking;
- drinking alcohol.
The most effective method of preventing pain is modifying lifestyle and preventing situations that cause cardialgia.
In order to eliminate the adverse effects of nervous system lability and spasm of the smooth muscles of the coronary vessels, the following is used:
- nitrates (“Nitroglycerin”, “Isoket”, “Nitrosorbide”) - drugs that stop an attack of angina, restore adequate blood flow through the coronary vessels to the muscle fibers of the heart;
- calcium channel blockers (“Amlodipine”) – used to eliminate vasospasm;
- sedatives (“Valerian extract”, “Glitsed”, “Novo-Passit”) - used for stress etiology of pain syndrome;
- cardioprotective drugs (“Mildronat”) – substances that increase the resistance of the myocardium to oxygen deficiency.
In addition, regular repetition of episodes of heart pain before the upcoming menstruation requires a detailed examination by a cardiologist in order to exclude organic pathology. Laboratory diagnostics of the concentration of sex hormones in different phases of the menstrual cycle is also recommended.
Drug treatment of dysmenorrhea
Drug treatment is based on the use of several groups of drugs that reduce pain during menstruation:
- Progestins are hormonal drugs used to renew the mucous membrane of the uterine cavity and relax its muscles;
- Oral contraceptives - suppress the ovulation process, reduce the synthesis of prostaglandins, which reduces the frequency and amplitude of uterine muscle contractions and, accordingly, pain;
- Non-steroidal anti-inflammatory drugs - drugs that suppress the production of prostaglandins (aspirin, diclofenac, ibuprofen, nimesulide).
In some cases, it is advisable to prescribe drugs such as:
- sedatives;
- vitamin complexes;
- homeopathic medicines that normalize the menstrual cycle and alleviate the general condition during menstruation;
- metabolic agents that replenish the deficiency of magnesium and potassium in the body;
- antispasmodics that reduce spasm of the uterine muscles.
Physiotherapy, as a rule, is prescribed to a woman in combination with drug treatment and is used in the second phase of the cycle. Suitable in many cases:
- acupuncture;
- electrophoresis;
- phonophoresis;
- massage;
- ultrasound therapy;
- manual therapy;
- treatment with electric current impulses;
- ultraviolet treatment;
- therapy using laser or magnetic radiation;
- breathing exercises;
- psychological help;
- auto-training.
Treatment of menstrual pain by type of disease
Treatment of dysmenorrhea is determined by the primary disease and may have a radically different medical approach.
- Endometriosis is a pathological growth of tissue of the uterine lining, causing pain during menstruation, requiring surgical removal of the nodes with further hormonal correction.
- Hormonal disorders - if, as a result of a blood test for hormones, a patient’s hormonal imbalances are detected, a rational solution would be to take hormonal medications, which are selected individually by a specialist, depending on the identified disorders.
- Infectious and inflammatory processes - as already mentioned, the cause of dysmenorrhea can also be inflammation of the pelvic organs, which is often infectious in nature. The cause of this phenomenon may be, in particular, a sexually transmitted infection. In this case, you will have to be treated with antibiotics, which the doctor will select based on the sensitivity of the identified pathogen.
- Dilatation of the pelvic veins is eliminated by taking vasoconstrictor drugs.
- Tumors of the pelvic organs - any neoplasm of the pelvic localization, both malignant and benign, can be accompanied by pain that intensifies during menstruation. Treatment in such situations may require surgery, which in most cases is performed by modern laparoscopy. It is worth adding that laparoscopy does not require dissection of the abdominal wall and does not leave ugly scars. Recovery after the procedure occurs very quickly and without complications.
- Adhesions - just like neoplasms, dysmenorrhea that occurs for a similar reason is most often treated laparoscopically.
The need for surgical intervention appears only in severe cases of dysmenorrhea, which is caused by the presence of pathologies of the organs of the woman’s reproductive system.
Nature of pain
Many women are not even aware that they have a cyst until they undergo a medical examination or develop complications. But sometimes, as the formation develops, a feeling of discomfort in the abdomen may appear in the early stages. This indicates the presence of irritated nerve nodes and pressure on the bladder.
As the formation grows, early pain occurs. With an ovarian cyst, the side hurts, it swells, increases in size, and the sensation of discomfort is constant. This is due to the fact that the formation presses on the wall of the abdominal cavity.
As the disease progresses or complications occur, a woman may notice severe discomfort, a feeling of squeezing, bursting from the inside. If such sensations appear, you should immediately consult a specialist.
Different types of cysts manifest themselves differently, and symptoms may also vary:
- Follicular. It causes virtually no pain. It manifests itself in the form of discomfort or nagging pain on the side where the formation occurred.
- Cystic formation of the corpus luteum. This form of cyst has almost no effect on the condition and does not cause pain. When localized on the right, discomfort may appear in that area.
- Dermioid. Causes intense pain at the location. This is due to the fact that the formation can greatly increase and affect the functioning of other organs.
- Muciotic. Benign formation with a tendency to malignancy. The pain is increasing in nature and radiates to the legs. As the formation grows, neighboring organs and tissues suffer.
- Endometriotic. Develops as a complication of endometriosis. With such an ovarian cyst, the lower abdomen hurts, problems with bowel movements arise, and convulsions and seizures may occur.
With polycystic disease, which is characterized by the development of several formations at once, severe nagging pain occurs. They are localized in the abdomen, in its lower part, and almost never stop. With prolonged growth of functional cysts and lack of proper treatment, hemorrhagic formations can occur. They are characterized by nagging pain that intensifies in the period before menstruation. At the same time, menstrual bleeding itself becomes more abundant.
Why are birth control pills prescribed for dysmenorrhea: are hormones needed?
Since it is known that attacks of pain occur only during menstruation with the ovulatory cycle (the so-called maturation and release of the egg), which can lead to pregnancy, the gynecologist selects oral contraceptives to alleviate the condition. They lead to inhibition of ovulation (the egg does not mature) and the disappearance of severe symptoms.
Since modern contraceptives have different hormone contents, they must be selected by a gynecologist. It is worth considering that this method is only suitable if the woman does not currently want to become pregnant. It is necessary to stop taking contraceptives 3 months before the desired pregnancy.
A new method of treating primary algomenorrhea is the administration of vasopressin hormone antagonists. Painful periods are often caused by an increase in its levels, resulting in uterine cramps. Vasopressin antagonists can normalize hormonal balance; the selection of these drugs is carried out by the doctor strictly individually.
Causes of pain
If an ovarian cyst hurts, this most often indicates the occurrence of a number of problems or complications of the condition. If you ignore the gynecologist's recommendations, discomfort may appear during:
- Active sex.
- Excessive physical activity.
- Injuries and impacts to the pelvic area.
If a woman followed all the recommendations, then the appearance of pain may indicate:
- Changing capsule sizes.
- Cyst rupture.
- Twist the legs.
These conditions require emergency intervention and constant medical monitoring, so if discomfort occurs, you should immediately seek help.
General recommendations for reducing menstrual pain
In addition to taking medications, there are a number of recommendations that, if followed, will help in the fight against menstrual pain:
- giving up bad habits: alcohol, smoking, caffeine;
- normalization of work and rest regimes;
- avoiding stress and emotional stress;
- good sleep;
- a healthy diet that excludes hard-to-digest foods, sweets, fatty and fried foods;
- normalization of body weight (if overweight);
- moderate physical activity: yoga, Pilates, swimming, various gymnastic exercises, jogging.
Complications of dysmenorrhea
Late diagnosis and treatment of pathology can lead to serious consequences:
- psychosomatic disorders – possible development of psychosis;
- the risk of the underlying disease becoming incurable (oncology, etc.);
- permanent loss of performance;
- infertility.
Pain during menstrual periods is not a direct symptom of infertility, but may be a consequence of diseases that reduce the ability to conceive. It is not surprising that women with painful periods sometimes cannot get pregnant. By consulting a doctor to treat dysmenorrhea, you can avoid infertility, because the doctor will diagnose and treat the cause itself.
Advantages of MC “HEALTHY FAMILY”
WE USE ONLY EUROPEAN, AMERICAN AND SOUTH KOREAN DRUGS ALL DRUGS ARE CERTIFIED YOUR COSMETOLOGIST HAS ABOUT 30 YEARS OF EXPERIENCE LOW PRICES FOR 100% US WE HAVE BEEN WORKING FOR COSMETOLOGICAL SERVICES OVER 1000 PATIENTS SINCE 2006 LOW COST OF BOTOX FROM 200 RUB. PER UNIT WE PROVIDE MORE THAN 5,000 COSMETOLOGY PROCEDURES PER YEAR
Cost of treatment for ovarian cysts
Ovarian cysts are a fairly common disease, which, despite a favorable course, can lead to a number of serious complications. To maintain women's health and diagnose as early as possible, you need to regularly visit a gynecologist and undergo preventive examinations.
With early diagnosis, specialists prescribe conservative treatment followed by physical therapy, but if large formations are detected, a tendency towards malignancy or other complications, surgery may be required. The cost of treatment depends on:
- Forms of education.
- Conditions of a woman.
- Presence of complications.
- The chosen treatment method.
You shouldn't skimp on your health. Contact qualified gynecologists and forget about living with pain.
Prevention
To prevent the occurrence and development of pain during menstruation, it is necessary to apply preventive measures:
- regular visits to the doctor for a gynecological examination (at least 2 times a year);
- refusal of the intrauterine device;
- timely treatment and diagnosis of gynecological diseases;
- avoidance of curettage and abortion;
- compliance with general treatment recommendations and doctor’s orders;
- Immediately visit a gynecologist if pain occurs during menstruation for two or more cycles.
How to relieve pain before going to the medical center
If pain with a left ovarian cyst greatly affects the quality of life, then before contacting a specialist, you can use painkillers. Painkillers are most often used in combination with antispasmodics:
- Ibuprofen.
- No-shpa.
- Paracetamol.
- Spazmolgon.
Additionally, you can use sedatives that will reduce the intensity of pain and help relax the muscles. In some cases, it is possible to use a heating pad, which is placed at the location of the cyst. This allows you to relieve spasm and further relax the muscles.
But you should not resort to self-medication and simply dull the pain. Based on the strength and nature of the manifestations, the doctor can determine:
- The patient's condition.
- Presence of complications.
- Localization of the cyst.
When pain is dulled by taking medications, this diagnostic method becomes ineffective, so immediately before visiting a doctor you should stop taking pills.
Traditional methods of treating painful menstruation
The use of traditional medicine recipes is effective for primary dysmenorrhea in combination with traditional therapy. Taking medicinal infusions is possible only in consultation with a gynecologist and only as an additional treatment that does not cancel the main therapy. Infusions begin to be taken 2 days before the onset of bleeding and continue throughout the entire period of menstruation. They have a relaxing, analgesic and calming effect.
The most common recipes:
- Oregano. 1 tbsp. Pour a glass of boiling water over the plants, leave for 30 minutes and strain. Drink small portions throughout the day on an empty stomach.
- Raspberries. 1 tbsp. pour a glass of boiling water over the leaves, leave for 15 minutes and strain. Drink the infusion in small portions a day.
- Valerian. 2 tbsp. Pour a glass of boiling water over the plants, heat in a water bath for 15 minutes, cool and strain. Drink the infusion 4 times a day after meals, 2-3 tablespoons.
- Elecampane root. 1 tbsp. finely chopped roots, pour 0.5 liters of boiling water, leave in a thermos for 2 hours, then strain. Take 0.5 cups 2 times a day.
- Carrot. Pour 50 g of seeds into 1 liter of water, boil over low heat for 1 minute, then leave for 30 minutes and strain. Drink the product in small portions throughout the day.
- Melissa. 2 tbsp. crushed leaves, pour 400 ml of boiling water, leave for 30 minutes and strain. Take 0.5 cups 3 times a day.
- Lovage. Pour 35 g of finely chopped roots into 1 liter of water, leave overnight in a thermos, boil in the morning over low heat for 5 minutes and strain. Take 2 tbsp. 3-4 times a day.
- Shepherd's purse and wormwood. Take 25 g of each plant, mix and pour 1 liter of boiling water. Let it brew in a thermos for 30 minutes, then strain. Take 150 ml 3 times a day.
Where to go for diagnosis and treatment of menstrual pain in St. Petersburg
Examination for such conditions is best done in specialized gynecological clinics that have modern diagnostic equipment. In St. Petersburg, the Diana Clinic provides treatment and diagnosis of pain during menstruation.
Gynecologists with the highest category work here, there is a new ultrasound machine, and a modern laboratory. The cost of an expert pelvic ultrasound is only 1000 rubles. The conclusion is issued in person.
If you find an error, please select a piece of text and press Ctrl+Enter