Feeling dizzy before your period is not uncommon. There are many possible causes, most of which are related to hormonal changes.
Other health conditions such as anemia, low blood pressure, and even pregnancy can cause dizziness. In some cases, dizziness may not be associated with menstruation at all.
In this article, we will discuss the most common causes of dizziness before menstruation, as well as treatments, prevention, and when to visit a doctor.
A sign of pregnancy?
Dizziness before your period can be a sign of pregnancy. Dizziness before pregnancy is associated with changes in the vascular system, which cause shifts in blood volume. Decreased blood volume can cause low blood pressure, which can cause weakness and dizziness.
Dizziness due to pregnancy often accompanies other early pregnancy symptoms such as nausea and vomiting. If you have no other symptoms, your dizziness is likely due to other hormonal changes.
Take a pregnancy test on the first day of your missed period to determine whether you are pregnant or not.
Before menstruation
With the onset of menstruation, progesterone always increases. This is a physiologically active substance produced by the endocrine system, which creates favorable conditions for the hatching of the embryo in the uterus. It relaxes its internal mucous membrane, preparing it to receive a fertilized egg, and also improves blood circulation in the pelvic organs, dilating blood vessels and participating in the formation of new branches necessary for the successful development of the unborn child.
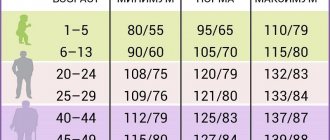
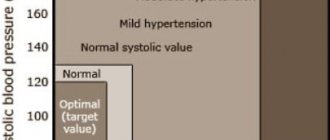
Vasodilation leads to increased blood pressure. Normally, its value should be 120/80 mmHg. Art., but for many women it is much higher or lower.
Other symptoms
Other symptoms that may accompany premenstrual dizziness depend on the cause.
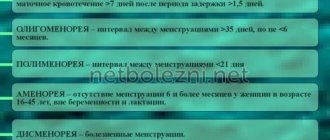
With PMS, PMDD and dysmenorrhea, these symptoms can include mood swings, insomnia, gastrointestinal discomfort and more. If you're pregnant, early pregnancy symptoms may also include increased urination, fatigue, and morning sickness.
Low blood sugar and low blood pressure may be accompanied by more serious symptoms such as sweating, shaking, and even loss of consciousness. These symptoms are dangerous and require immediate medical attention.
Migraine attacks can also have similar neurological symptoms. However, these symptoms usually go away after the attack ends.
Reduced body temperature
Iron deficiency
33138 09 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Low body temperature: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
Low body temperature, or hypothermia, is a disorder of heat metabolism, manifested by a decrease in body temperature due to exposure to low temperatures and/or a decrease in heat production and an increase in heat output.
There are several mechanisms for active heat production.
Mandatory heat production
- heat produced as a result of normal physiological and metabolic processes. It is enough to maintain normal body temperature in a comfortable ambient temperature.
Additional heat production
activates when the ambient temperature drops and includes:
- non-contractile thermogenesis
, which is carried out by the breakdown of brown fat. Brown fat is present in large quantities in newborns and protects them from hypothermia. In adults there is little of it, it is localized in the neck, between the shoulder blades, near the kidneys; - contractile thermogenesis
, which is based on muscle contraction.
When the body becomes hypothermic, muscle tone (tension) increases and involuntary muscle tremors appear.
Passive heat retention is carried out using subcutaneous fatty tissue.
The rate of metabolic processes and adaptation reactions is influenced by hormones of the adrenal glands and thyroid gland, and the center of thermoregulation is located in the hypothalamus.
For a person, the comfort zone is considered to be the air temperature range from +18°C to +22°C, subject to light clothing and normal physical activity.
There is a distinction between central body temperature (maintained in the internal organs and central vessels at 36.1–38.2°C) and the temperature of peripheral tissues (extremities, body surface) - normally it is tenths of a degree lower than the central temperature.
Central body temperature is measured in the rectum, external auditory canal, and mouth. In a medical facility, it is possible to measure temperature in the lumen of the esophagus, in the nasopharynx, and in the bladder. Peripheral temperature can be measured on the forehead or armpits.
In general, body temperature indicators are individual and each location has its own normal range. Body temperature changes throughout the day. Due to the intensity of metabolic processes, young children have a higher normal temperature level. The metabolism of older people is slow; the internal temperature can normally be at 34–35°C.
Varieties of low temperature
A decrease in temperature can be endogenous (with pathology of internal organs and imperfect thermogenesis) and exogenous (depending on environmental conditions).
An exogenous decrease in temperature includes drug-induced hypothermia. Its task is to reduce the functional activity and metabolism in organs and tissues in order to increase their resistance to oxygen deficiency. It is used in the form of general controlled hypothermia when there is a need to temporarily slow blood circulation; and local controlled hypothermia of individual organs and tissues.
Drug hypothermia is used during open operations on the heart and large vessels, for ischemic stroke, injuries of the central nervous system (brain and spinal cord), and for severe oxygen starvation of newborns.
The severity of a person’s condition is assessed by the level of decrease in core temperature and clinical manifestations.
At a low temperature (36.5–35°C) a person can feel quite well. It follows from this that she is a variant of the norm for him. If a person feels unwell, it is necessary to look for the cause of the drop in temperature.
Body temperature below 35°C is considered low.
Low temperature is detected:
- mild severity (35.0–32.2°C)
, in which drowsiness, increased breathing, heart rate, and chills are observed; - moderate severity (32.1–27°C)
– a person may become delirious, breathing slows down, the heartbeat slows down, reflexes decrease (reaction to an external stimulus); - severe severity (below 27°C)
- a person is in an extreme degree of depression of consciousness (in a coma), blood pressure is reduced, reflexes are absent, deep disturbances in breathing and heart rhythm are noted, the balance of the internal environment of the body and all metabolic processes are disturbed.
Possible causes of low temperature
Possible causes of hypothermia include:
- damage to the central nervous system;
- decreased muscle mass;
- physical fatigue;
- decrease in the speed of metabolic processes;
- pregnancy;
- period of convalescence after a protracted illness;
- dysregulation of vascular tone;
- various intoxications, including alcohol;
- exposure to medications, including overdose of antipyretics;
- intravenous infusion of large volumes of unheated solutions;
- hypothermia in conditions of low air temperature;
- prolonged exposure to wet or damp clothing;
- prolonged exposure to cold water, on cold objects, etc.
All of the above factors can lead to disruption of thermoregulation, decreased heat production, and increased heat loss.
What diseases cause low temperature?
Body temperature can decrease with paresis and paralysis of muscles and/or a decrease in their mass that occurs due to diseases (syringomyelia) and spinal cord injuries, damage to the nerve fibers innervating the muscles, calcium deficiency, hereditary diseases (Erb-Roth muscular dystrophy, Duchenne).
A slowdown in metabolism occurs with chronic insufficient function of the adrenal glands (for example, in autoimmune processes) and the thyroid gland (hypothyroidism), diffuse diseases of the liver, kidneys, with a significant decrease in glucose levels (hypoglycemia), with reduced hemoglobin and/or a decrease in the number of red blood cells (anemia) , with insufficient nutrition, severe exhaustion (cachexia) and thinning of subcutaneous fat.
Violation of thermoregulation is observed with traumatic, medicinal or toxic effects on the hypothalamus.
Hypothermia can occur with extensive multiple trauma or during a systemic infectious process (sepsis).
Which doctors should I contact if I have a low body temperature?
To save a person with severe hypothermia, an emergency medical team must be called.
If a person has recorded a decrease in body temperature by 1–2°C in relation to his individual norm, this condition persists for a long time and is not associated with hypothermia, he should consult a therapist, and, if necessary, a neurologist or endocrinologist.
Diagnostics and examinations for low body temperature
Diagnosis of low body temperature consists of examining and interviewing the patient, measuring body temperature and blood pressure, and assessing blood oxygen saturation (pulse oximetry, blood gas testing).
To identify disturbances in the functioning of organs and systems, the following laboratory and instrumental studies may be prescribed:
- clinical blood test;
During and after menstruation
The main cause of dizziness before menstruation is due to hormonal changes . Estrogen rises twice during the menstrual cycle—once during the follicular phase and once during the luteal phase. Because one increase in estrogen levels occurs just before your period, this is exactly the time when you feel dizzy.
However, you can also experience dizziness from hormonal changes right before ovulation .
This is when estrogen and progesterone levels are highest, which can affect symptoms.
When to see a doctor
If the deterioration in well-being occurs sporadically, does not cause significant inconvenience to the patient and stops immediately with the end of menstruation, you can not consult a doctor, but limit yourself to reducing physical activity and devoting more time to rest.
If surges in blood pressure continue during and after menstruation, this may indicate indolent diseases of the cardiovascular system - hypertension or hypotension. Heart rhythm disturbances, lethargy, hot flashes, and in some cases fainting can also often be observed.
All these symptoms require immediate consultation with a doctor, since untreated diseases can not only significantly reduce the quality of life, but also, in the event of negative developments, cause hospitalization.
Treatment
If pre-menstrual dizziness is caused by hormonal changes, you can ease symptoms through lifestyle changes such as:
- to drink a lot of water
- get some sleep
- exercise regularly
- eat a balanced diet
As for other causes of dizziness before your period:
Iron deficiency anemia , which can be diagnosed with blood tests. Once diagnosed, your doctor may prescribe iron supplements and offer dietary recommendations to increase your iron intake.
Low blood pressure. If your blood pressure drops before your period starts, make a few changes to your daily schedule to help your body. Drink enough water, don't stand up abruptly, and be aware of any other symptoms that develop.
Low blood sugar. Low blood sugar before your period is most likely a temporary symptom of hormonal changes. Eat small, frequent meals to maintain blood sugar levels.
Migraine. Making lifestyle changes to avoid triggers is the most important step in treatment. If this is not enough, consider asking your doctor for medications that may help.
Regarding medical conditions and other medications that cause dizziness, it is important to see a doctor for diagnosis, treatment, and medication adjustments if necessary.
Prevention
To eliminate the pressure from the future, follow the diet, nutrition and use preventive measures accordingly:
- reduce the amount of salt and sugar in your daily diet;
- Limiting the strength of training, preferring equally effective exercises for women: Pilates, yoga or breathing exercises;
- Replace coffee drinks with herbal infusions;
- Quit smoking and drinking alcohol.
Don't forget that every woman's body is a separate system. They must be carefully analyzed to find out how to overcome pressure surges or avoid them. If necessary, please contact specialists.
Risk factors
Certain habits can affect your hormone levels, which can lead to an increased risk of dizziness before your period. These include:
- chronic stress
- excess weight
- unbalanced diet
- certain medications
- environmental factors such as toxins
Some medical conditions can also cause an imbalance in hormones, which can predispose you to dizziness. The endocrine system influences important hormones in the body.
Why does the pressure rise?
High blood pressure can be caused by the following reasons:
- Violation of the water-salt balance of the body, stagnation of fluid in the tissues and resulting tension in the blood vessels;
- constant changes in blood vessels and the active pulsation of blood they cause;
- Significant decrease in serotonin levels in the body.
In the first case, the woman begins to swell greatly, in the second her heartbeat quickens and she feels slight pain behind the sternum, in the third she becomes the subject of frequent emotional outbursts, and sometimes even falls into hysterics.
Conclusion
Dizziness before menstruation is often caused by hormonal changes during the menstrual cycle. PMS, PMDD and dysmenorrhea are the most common causes. Other conditions that cause dizziness, such as low blood pressure, can also be caused by hormonal changes during menstruation.
Lifestyle changes can help relieve many of the symptoms of these conditions. However, if you experience other symptoms or dizziness is affecting your daily life, see your doctor for diagnosis and treatment.
What to do if there are changes at different periods of the cycle?
The algorithm of actions in case of fluctuations in indicators depends on the general condition of the woman, the degree of changes and the main cause.
Minor physiological changes do not require drug correction. If attacks of weakness, nausea, or headache occur, it is recommended:
- active or passive rest (depending on the severity of the condition);
- removing salty, smoked, sour and spicy foods from the diet (more effective with high blood pressure);
- drink a sweet warm drink;
- take a soothing herbal medicine (valerian extract or chamomile decoction).
If pathological signs appear that persist for several cycles (at least 2), or the woman’s condition is serious, a doctor’s consultation is necessary.
It is recommended to contact:
- gynecologist;
- endocrinologist;
- cardiologist;
- psychologist.
After the consultation, the doctor will prescribe the necessary tests (laboratory analysis of a hormonal panel, daily blood pressure monitoring, etc.) and adequate therapy.
Doctors' opinion
Many experts note that patients often complain at appointments about deterioration in health due to pressure surges during menstruation. To reduce negative symptoms, doctors advise adhering to the following simple rules:
- During menstruation, you should adjust your diet. It is necessary to limit the consumption of salty foods, and also replace coffee and caffeine-containing drinks with juices and herbal teas. The fact is that such products themselves can provoke pressure surges, and during menstruation they can only aggravate negative well-being.
- It is important to dose physical activity, especially if heavy bleeding is observed. In this case, it is recommended to remain in bed and return to normal activity after the end of the critical days.
- You should eat as many foods rich in vitamins and minerals as possible.
- It is important to avoid stressful situations, as they can contribute to the occurrence of blood pressure disorders.
- Follow a daily routine, sleep at least 8 hours and give up bad habits.
- It is extremely important to stop taking painkillers uncontrollably, as their effect on vascular tone can be significant. You should consult with a gynecologist so that the doctor selects the optimal pain reliever based on the patient’s health condition and concomitant pathologies.
All these recommendations will help not only reduce the risk of increased or decreased blood pressure, but also smooth out other negative manifestations that occur during menstruation.