Diagnostics
Silent myocardial ischemia is detected using the same diagnostic methods as other forms of coronary artery disease. Along with studying the medical history and a thorough examination conducted by a cardiologist, the following types of examination are used:
- Holter monitoring. It is prescribed for suspected painless myocardial ischemia.
- Stress tests. It is usually performed on a treadmill or exercise bike and monitors your heart rate, blood pressure and breathing. If your doctor suspects you have myocardial ischemia but you do not have any signs or symptoms, they may order this cardiovascular test.
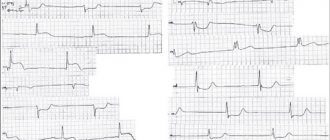
- Electrocardiogram (ECG). Records abnormalities in the electrical activity of your heart, which indicate subepicardial or subendocardial myocardial ischemia.
- Clinical blood tests.
- Echocardiogram. It will help determine the area of heart damage and dysfunction.
- Coronary angiography. Coronary angiography uses X-ray images to look at the inside of your heart's blood vessels. During a coronary angiography, a contrast agent is injected into the blood vessels of your heart, which is visible on X-ray images. In this case, the X-ray machine takes a series of images (angiograms), which makes it possible to study the condition of the blood vessels.
- CT scan of the heart. A CT scan reveals the presence of calcification of the heart vessels, the main symptom of atherosclerosis. The condition of the coronary vessels is also assessed using CT coronary angiography.
Classification of the disease
Experts distinguish 2 main forms of silent ischemia:
A feature of the pathology is that the patient feels healthy. He may not be aware of the problem until complications begin to develop.
In some cases, the disease is accompanied by:
- weakness;
- rapid fatigue;
- dizziness.
Usually patients do not pay attention to a symptom that manifests itself once!
Meanwhile, the pathology is progressing! It can transform into a new form and clearly manifest itself with attacks of pain.
Complications of the disease include:
- heart rhythm disturbances;
- chronic heart failure;
- myocardial infarction.
In some cases, ischemia causes sudden death. Medical professionals assess the prognosis of pathology without adequate therapy as unfavorable. This is due to the fact that the mortality rate reaches 35%.
Treatment
Treatment of the painless form of myocardial ischemia is carried out using the same methods as the treatment of coronary heart disease, which occurs with characteristic symptoms. Depending on the stage of the disease and its characteristics, the doctor will prescribe:
- Drug treatment. Some heart medications help stop the development of coronary artery disease. Necessary medications include medications that normalize blood pressure and improve the quality of the heart muscle. Patients also take medications that lower blood cholesterol levels and reduce blood viscosity.
- Myocardial revascularization. To treat coronary artery disease, coronary artery bypass surgery or intravascular surgery is used. If indicated, the best option is considered to be endovascular surgery to restore the affected vessels - stenting. This type of surgery is painless because it does not require general anesthesia or incisions. During the operation, an endoprosthesis is installed into the vascular lumen from the inside - a stent, which holds the walls of the vessel and ensures normal blood flow.
- Normalization of lifestyle and secondary prevention. It is recommended to exclude factors that cause the growth of cholesterol plaques: fatty foods, sedentary lifestyle, smoking. We will talk more about the prevention of coronary disease in the next publication.
Asymptomatic myocardial ischemia
Myocardial ischemia is a reliable indicator of physiologically significant coronary heart disease (CHD). Over the past two decades, epidemiological studies and prospective observation have shown that asymptomatic myocardial ischemia (ASMI) detected on ECG is an unfavorable prognostic factor, as well as in patients with proven CAD. The results of these studies revealed such a high prognostic value of myocardial ischemia in asymptomatic patients that the American Heart Association and the American College of Sports Medicine recommended before starting intensive physical training programs in men over 45 years of age and in women over 55 years of age without obvious heart disease and even without risk factors. their development, conduct a maximum exercise test on a treadmill.
Despite these recommendations, the feasibility of conducting routine screening studies in apparently healthy individuals to detect myocardial ischemia remains controversial. This is due to the fact that in practically healthy individuals, myocardial ischemia is often diagnosed during a stress test only by changes in the ST segment, but without accompanying chest pain. The absence of symptoms led to the assumption that ST segment changes during an exercise test, not accompanied by chest pain, do not always reflect ischemic changes in the myocardium and may be a source of false-positive data. Such doubts arose due to improper selection of patients for the stress test, in which the majority of those examined initially had a low probability of being diagnosed with coronary artery disease. At the same time, with proper selection for the study (individuals with a high probability of coronary artery disease), painless depression of the ST segment during exercise allows us to identify a group of patients with a high risk of developing cardiovascular events and cardiac death.
Diagnostics
Transient myocardial ischemia is most often subendocardial. Episodes of subendocardial ischemia are usually diagnosed using ECG monitoring by horizontal or downward ST segment depression >1 mm at a distance of 0.06-0.08 s from the J point for at least 1 minute.
Having overcome the initial technical difficulties of correctly reproducing low-frequency ECG signals, modern technology allows reliably reproducing the position of the ST segment using ECG monitoring devices. The ability to detect myocardial ischemia using ECG monitoring has increased through the use of bipolar precordial leads. In this case, one of the leads must be a modified lead V5 - CM-V5, since it has the greatest sensitivity for detecting ST segment depression, regardless of the location of ischemia. Currently, ECG monitors have appeared that allow recording from 3 and even 12 leads. However, the question of the advisability of using more than 2 leads to improve the diagnosis of subendocardial ischemia has not yet been resolved.
The absence of angina pectoris during myocardial ischemia in some cases can be explained by the short duration and/or mild severity of ischemia. With significant severity and duration of ischemia, the absence of pain can be caused by several mechanisms. Probably, the reasons for the absence of angina are different: in patients with a combination of painful and painless attacks, in patients with predominantly painless attacks and in patients with diabetes mellitus.
A combination of episodes of painful and silent myocardial ischemia. Impulses carried along cardiac afferent nerve fibers are modulated in the cardiac ganglia, mediastinal and thoracic ganglia (cardiac afferent fibers passing in the sympathetic nerves) or in the nuclei of the tractus solitarius (cardiac afferent fibers passing in the parasympathetic nerves). Then the modulation of impulses is carried out in the gray matter of the brain, located near the aqueduct of Sylvius, in the hypothalamus and thalamus. After this, the impulses bilaterally approach different parts of the cerebral cortex, where they can be transformed into pain sensations.
The response of the internal ganglia of the heart changes at excitatory and inhibitory synapses. Local exposure to internal cardiac neurons of a number of factors (substance P, bradykinin, oxytocin, acetylcholine, nicotine, adenosine and ATP) leads to changes in the activity of internal cardiac neurons. It has been established that the application of these factors to the epicardial surface of the heart changes the activity of neurons in the nodular ganglia for up to 45 minutes. Infusion of very low doses of adenosine can reduce the severity of exercise-induced angina. These data indicate that the perception of ischemic chest pain depends not only on the production of signals initiated by myocardial ischemia, but also on their modulation in the internal cardiac ganglia, mediastinal ganglia and chest wall.
Further changes in impulses caused by ischemia can occur in the central nervous system at the spinal or supraspinal level. However, after reaching the central nervous system, afferent impulses are conducted in the spinothalamic tract together with other visceral and somatic afferent nerve impulses. It is unlikely that selective suppression of ischemic chest pain of the same duration and severity is possible at this level. Thus, the exact mechanism of the absence of pain in patients with a combination of painful and painless ischemic attacks remains unknown.
Absence of angina in patients with BMI. In individuals who have never experienced anginal pain, even with the development of severe, prolonged ischemia, or who experience predominantly painless episodes, the absence of pain may be due to psychological factors that persistently suppress the perception of pain. This assumption is supported by a generalized disturbance in pain perception. Indeed, patients with PMI have a higher threshold and tolerance to painful stimuli compared to those with painful ischemia. These data are confirmed using the following types of stimulation: forearm ischemia, cold exposure, intravenous adenosine, dental pulp irritation, etc. A study of the personality characteristics of patients with asymptomatic ischemia also reveals lower rates of nervousness and excitability and higher rates of masculinity and a lower predisposition to complaints.
There is an assumption about the role of endogenous opioids in the pathogenesis of BIM. There are three groups of endogenous opioids, derived from three different precursor molecules: 1) endorphins, which are secreted mainly by the pituitary gland; 2) enkephalins secreted by the adrenal glands; 3) dynorphins, the source of which is not yet known. Endogenous opioids act centrally to cause selective suppression of nociceptive neurons. At the same time, according to positron emission tomography data, patients with myocardial infarction compared with patients with angina pectoris had significantly less activation of the cerebral cortex during myocardial ischemia.
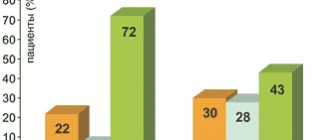
Clinical and prognostic significance of BIM in stable course of coronary artery disease. Assessment of the daily rhythm of episodes of myocardial ischemia in a stable course of coronary artery disease reveals the peak of their occurrence in the morning, especially during the first hours after awakening and the start of work activity, that is, during the period corresponding to maximum sympathetic activation with a corresponding increase in myocardial oxygen demand and coronary tone arteries. According to ambulatory electrocardiogram monitoring (AECGM), in patients with stable coronary artery disease, the presence of asymptomatic episodes of myocardial ischemia during normal daily activities may indicate a poor prognosis. Thus, with 24-hour ECG monitoring, D. Tzivoni et al. Among 224 patients with a stable course of coronary artery disease after myocardial infarction, 33% had episodes of silent myocardial ischemia. During 28-month follow-up, the incidence of cardiovascular events (death, reinfarction, hospitalization for angina, balloon angioplasty, or CABG) was 51% among patients with ischemic episodes compared with 12% among patients without such changes (p<0. 0001). According to monitoring data, myocardial ischemia was a more significant unfavorable prognostic factor compared with ischemia detected by exercise testing (P<0.001).
Data on the higher prognostic significance of detecting myocardial ischemia during AECGM compared with the exercise tolerance test (ETT) were also confirmed in the Asymptomatic Cardiac Ischemia Pilot (ACIP) Study. Reliable direct correlations were established between ischemia indices according to the TFT data (number of ECG leads with ST segment depression, exercise time before the development of ST segment depression, persistence of ST segment depression in the recovery period, maximum depth of ST segment depression) and the presence and frequency of asymptomatic ischemia according to the data AECGM. Despite the presence of correlations between TFT and AECGM in establishing the fact of ischemia, the correlations between indices of the severity of ischemia during TTF and AECGM turned out to be low.
The Angina and Silent Ischemia Study Group (ASIS) did not find significant correlations between the number of episodes of myocardial ischemia during AECGM and the duration of exercise before the onset of ST segment depression. Thus, although TTFF was useful in identifying patients with a high likelihood of myocardial ischemia during AECGM, the frequency of ischemic episodes detected during AECGM did not reflect the severity of ischemia according to TFTN. Since the prognosis of patients with stable angina pectoris can be determined not only by the severity of myocardial ischemia during TFA, but also by the presence and frequency of asymptomatic episodes of ischemia during AECGM, monitoring provides additional and independent prognostic information.
Ambulatory ECG monitoring provides significant diagnostic assistance in the evaluation of patients with the so-called cardiac syndrome X (anginal pain, positive TFT, normal coronary arteries on coronary angiography), which is considered a manifestation of microvascular coronary disease. Analysis of episodes of ST segment depression revealed their similarity with those in patients with stable coronary artery disease. It has also been shown that AECGM detects episodes of ST segment depression in some patients (up to 50%) with angina pectoris and normal coronary arteries, but negative TFT, which may indicate vasomotor microcirculatory disorders in the genesis of the pain syndrome in this category of patients, as well as and with classic syndrome X.
In patients with coronary artery disease who have undergone surgery (not on the heart), the presence of episodes of myocardial ischemia in the postoperative period (97% of them painless) is highly correlated with an unfavorable outcome due to cardiac complications.
Clinical and prognostic significance of BIM in acute coronary syndromes. Acute coronary syndrome, which includes unstable angina and non-Q wave myocardial infarction, has a very high risk of developing Q-wave myocardial infarction or death. An important prognostic sign in acute coronary syndromes is transient myocardial ischemia, determined by changes in the ST segment during long-term ECG monitoring.
Back in 1986, SOGottlieb et al. Based on an analysis of 24-hour ECG monitoring in patients hospitalized with unstable angina, it was found that myocardial infarction develops in 16% of patients with episodes of transient ischemia, but only in 3% without them (p = 0.005). At the same time, an increase in ischemia time >60 minutes per 24 hours increased the prognostic value of the development of coronary events, including revascularization procedures. A. Rebuzzi et al. when examining 102 patients with unstable angina, they found that in a multivariate analysis, transient myocardial ischemia according to 24-hour ECG monitoring turned out to be the strongest predictor of adverse cardiac events. The prognostic value of ST segment depression detected during daily ECG monitoring in patients with unstable angina increases with the simultaneous study of frequency indicators of heart rate variability.
A detailed analysis of the characteristics of myocardial ischemia in patients with acute coronary syndrome was carried out in a study by DJ Patel et al. 256 patients with unstable angina or non-Q wave myocardial infarction underwent 48-hour ECG monitoring while receiving maximum drug therapy. During 10,629 hours of monitoring, 44 patients (17.2%) experienced 176 episodes of transient ischemia. The average heart rate at the time of development of ischemia was 68 beats per minute, and during asymptomatic myocardial ischemia it did not differ significantly from the pulse during painful ischemia. More than half of the episodes of myocardial ischemia developed without a previous increase in heart rate.
The majority of ischemic episodes (64%) occurred between 10 pm and 8 am. The time of occurrence and nature of ischemic episodes did not differ in patients with myocardial infarction without a Q wave and unstable angina, but with myocardial infarction, ischemic episodes occurred more often compared with unstable angina (27.3% and 15.1%, respectively) and were longer lasting ( on average 20 minutes and 13.5 minutes, respectively, p<0.01). Thus, in acute coronary syndromes there is a low threshold for the occurrence of transient ischemia, which occurs without increasing the myocardial oxygen demand, more often at night rather than in the morning. This distinguishes myocardial ischemia in acute coronary syndromes from ischemia that occurs during stable coronary artery disease.
Prognostic significance of BIM in acute myocardial infarction and after it. Several studies have demonstrated the prognostic value of BMI during predischarge ECG monitoring of patients who have suffered acute myocardial infarction. JBGill et al. Based on a study of 406 patients, one-year mortality was 11.6% among patients with signs of transient ischemia during 48-hour ECG monitoring and only 3.9% among patients without ischemic episodes (p = 0.009). The same trend was noted for the combined endpoint of death or reinfarction: 23.2% and 9.6%, respectively, in the group of patients with and without ischemic episodes (p=0.001).
When observing 239 patients with myocardial infarction for more than 2 years, it was found that among patients with myocardial ischemia during ECG monitoring before discharge, 29% experienced death or recurrent infarction, and among patients without ischemia, these events occurred in only 8% ( p<0.01). In multivariate analysis, silent ischemia was the only independent predictor of recurrent infarction.
Silent myocardial ischemia as a prognostic factor is thought to gain added value in a subgroup of high-risk patients, including those in whom TfT is contraindicated and those with low left ventricular contractility.
Apparently, the prognostic value of BIM decreases as the time after the infarction increases. A. J. Moss et al. studied the role of TTFN and the stress test with assessment of myocardial perfusion using AECGM in 966 patients 1-6 months after acute myocardial infarction and did not reveal the prognostic value of BIM according to AECGM in relation to repeated ischemic events, and the stress test had only borderline statistical significance regarding the forecast of these events.
In a study by G. Casella et al., which included 766 sick patients with stable coronary artery disease after myocardial infarction (average period after myocardial infarction was 2.8 + 0.75 years), it was found that painless ischemia during TFT indicated less severe ischemia myocardium. Thus, patients with silent ischemia had a longer duration of exercise, a higher ischemic threshold and a shorter period until ST segment normalization compared to patients with painful myocardial ischemia (p<0.001 for all indicators). Based on the data obtained, the authors conclude that patients with stable coronary artery disease after myocardial infarction represent a low-risk category, and the asymptomatic nature of myocardial ischemia in these patients is not an unfavorable prognostic factor.
Silent myocardial ischemia in patients with diabetes mellitus. Patients with diabetes mellitus have a significantly increased risk of developing coronary atherosclerosis and can suffer asymptomatic myocardial infarction, not accompanied by chest pain. Based on these premises, one would expect a higher incidence of asymptomatic myocardial ischemia in patients with coronary artery disease and diabetes mellitus compared with patients with coronary artery disease but without diabetes.
Some authors explain the asymptomatic course of IHD in patients with diabetes mellitus by the presence of autonomic neuropathy involving the afferent nerves of the heart. I.Fearman et al. in a study of the hearts of 5 patients with diabetes mellitus who died from BMI, it was found that intramyocardial nerves have morphological changes characteristic of diabetic neuropathy (clear thickening of nerve fibers, their spindle-shaped change, fragmentation of fibers, decrease in the number of neurons).
Niakan et al. studied the relationship between the presence of peripheral neuropathy and the incidence of silent myocardial infarction in 73 patients. It was found that in patients with signs of neuropathy, BIM developed in 20% of cases, in patients without signs of autonomic dysfunction - only in 4% of cases.
However, data on the prevalence of silent myocardial ischemia (according to TFT and AECGM data) among patients with diabetes mellitus and coronary artery disease compared with patients with coronary artery disease but without diabetes are ambiguous. Some authors point to a higher incidence of MI in patients with diabetes mellitus, while others do not note significant differences in the prevalence of asymptomatic myocardial ischemia during TFA depending on the presence or absence of diabetes mellitus.
Attempts to answer the question of the prevalence of silent myocardial ischemia were made by analyzing data from the ACIP study already mentioned above. The incidence and characteristics of myocardial ischemia during TFT and 48-hour ECG monitoring were compared in 77 patients with coronary artery disease and diabetes mellitus controlled by hypoglycemic drugs or insulin, and in 481 patients with coronary artery disease but without diabetes. Multivessel coronary artery disease was more common in patients with diabetes compared with patients without diabetes (87% and 74%, respectively, p=0.01). The percentage of patients without angina pectoris during TFA was almost the same in the group of patients with diabetes and without diabetes (36% and 39%, respectively). The time to the onset of ST segment depression (1 mm) and the time to the development of an angina attack did not differ significantly between groups. The proportion of patients who had only asymptomatic ST segment depression at 48-hour AECGM was also almost the same in the group of patients with and without diabetes (94% and 88%, respectively). At the same time, in the group of patients with diabetes, compared with patients without diabetes, a shorter total duration of ischemia over 24 hours, a shorter average duration of one ischemic episode, and a smaller depth of ST segment depression were noted. Thus, the ACIP study made it possible to establish the same incidence of asymptomatic myocardial ischemia according to TFT and 48-hour AECGM in patients with coronary artery disease on the background of diabetes mellitus and patients with coronary artery disease without diabetes, despite more pronounced and diffuse damage to the coronary arteries in the first group of patients.
Some authors dispute the validity of the conclusions of the ACIP study about the absence of significant differences in the prevalence of silent myocardial ischemia in patients with coronary artery disease with diabetes mellitus and in patients with coronary artery disease without diabetes, emphasizing the lack of data on the frequency of autonomic dysfunction among the examined patients with diabetes mellitus.
Despite the theoretical premises, evidence that diabetic autonomic neuropathy is the main cause of asymptomatic CAD in many patients with diabetes has not yet been rigorously demonstrated in clinical or epidemiological studies. The higher frequency of asymptomatic ischemic heart disease in patients with diabetes mellitus is often explained by the higher prevalence of ischemic heart disease among these patients and more severe coronary atherosclerosis, in which the frequency of detection of myocardial ischemia, including asymptomatic ones, increases.
Treatment
The general therapeutic strategy in patients diagnosed with coronary artery disease is the modification of risk factors and the use of antiplatelet agents. This approach is recommended for all patients, regardless of the presence or absence of asymptomatic ischemia.
Evidence has been obtained that lowering plasma cholesterol levels can reduce the severity of silent myocardial ischemia in patients with proven coronary artery disease. In a small randomized study that included 40 patients with proven coronary artery disease and episodes of ST segment depression during AECGM, on the background of diet and lovastatin therapy after 4-6 months, complete disappearance of episodes of myocardial ischemia was noted in 65% of patients, while in the control group only in 10%. The decrease in the severity of ischemia in the treatment group compared to the control group turned out to be statistically significant (p<0.001). A decrease in the incidence of BMI during statin therapy is associated with an improvement in endothelial function.
Treatments directly aimed at reducing myocardial ischemia include pharmacological (therapy with beta-blockers, calcium antagonists and nitrates) and invasive methods (coronary angioplasty and coronary artery bypass grafting).
The Atenolol Silent Ischemia Study Trial (ASIST) is the first randomized placebo-controlled trial to demonstrate the ability of beta-blockers to reduce the incidence of silent myocardial ischemia and improve clinical outcomes of patients. In this study, 306 patients with proven coronary artery disease and signs of myocardial ischemia during AECGM were randomized to treatment with atenolol at a dose of 100 mg/day or placebo. After 4 weeks of atenolol therapy, the number of ischemic episodes decreased (on average from 3.6 + 4.4 to 1.7 + 4.6; p < 0.001) and their duration (from 30 + 3.3 to 16.4 + 6, 7 minutes) according to 48-hour ECG monitoring. Survival without cardiac events was higher in the atenolol group compared with the placebo group (p <0.0066). The strongest predictor of cardiac event-free survival was the absence of ischemia during AECGM 4 weeks after the start of treatment.
In the Circadian Anti-ischemia Program in Europe (CAPE) study, 315 patients with stable coronary artery disease and more than 4 episodes of myocardial ischemia during 48-hour ECG monitoring were randomized to receive amlodipine or placebo. Two thirds of patients in each group received beta blockers. Compared with placebo, amlodipine significantly reduced the incidence and duration of ischemic episodes (p=0.025).
The Canadian Amlodipine/Atenolol in Silent Ischemia Study (CASIS) compared amlodipine therapy with placebo, atenolol with placebo, and combination therapy with atenolol and amlodipine in 100 patients with stable coronary artery disease and myocardial ischemia during treadmill exercise and AECGM. Amlodipine was more effective in reducing exercise-induced ischemia, while atenolol was more effective in preventing ischemia detected by AECGM. Combination therapy with amlodipine and atenolol had a more pronounced anti-ischemic effect compared to monotherapy with each drug.
The Total Ischemic Burden Bisoprolol Study (TIBBS) included 330 patients with stable angina, positive TBI, and more than 2 episodes of myocardial ischemia during 24-hour ECG monitoring. 161 patients were included in the bisoprolol treatment group, and 169 patients were included in the long-acting nifedipine treatment group. Bisoprolol and nifedipine significantly reduced the average number of ischemic episodes. However, bisoprolol was more effective than nifedipine in reducing the frequency and duration of ischemia.
The Total Ischemic Burden European Trial (TIBET) randomized 682 patients with stable angina to treatment with atenolol, nifedipine, or a combination of both. Before randomization and during treatment, patients underwent TFT and AECGM. Reductions in ischemia were noted in all three groups. In the combination therapy group, the degree of reduction in ischemia was more pronounced than in each of the monotherapy groups. The annual incidence of the primary endpoint (death or nonfatal cardiovascular event) did not differ between the two groups.
One of the most significant studies of asymptomatic myocardial ischemia is the Asymptomatic Cardiac Ischemia Pilot (ACIP) study, which compared various treatment strategies for patients with ischemic heart disease and myocardial infarction. The study included 558 patients with angiographically proven coronary artery disease and coronary anatomy allowing revascularization. Randomization was carried out in one of three groups: 1) treatment of angina with titration of doses of antianginal drugs until its disappearance (n=183); 2) treatment of angina and ischemia under AECGM control (n=183); 3) revascularization with angioplasty or coronary artery bypass grafting (n=192; of these, 49% underwent angioplasty, 41% underwent coronary artery bypass grafting, and 10% without intervention). Drug therapy in the first two groups was carried out with atenolol, a combination of atenolol with nifedipine, diltiazem, or a combination of diltiazem with isosorbide dinitrate. Myocardial ischemia during AECGM 12 weeks after the start of treatment was not recorded in 39% of the angina treatment group, in 41% of patients in the angina and ischemia treatment group, and in 55% of the revascularization group. All three treatment strategies resulted in a reduction in the average number of ischemic episodes and the total duration of periods of ST segment depression in AECGM. However, the most important finding of the ACIP study was the improved rate of cardiac event-free survival in the revascularization group compared with the medical therapy groups at 1 year of follow-up. Moreover, 65% of patients in the revascularization group did not require drug therapy. Comparison of drug therapy revealed more effective suppression of myocardial ischemia in the subgroup of treatment with atenolol and/or nifedipine compared with the subgroup of treatment with diltiazem and/or isosorbide dinitrate.
Nitrates in the form of oral or transdermal forms are often used to treat patients with stable coronary artery disease. The rapid development of tolerance limits the effectiveness of long-acting nitrates. To reduce tolerance, it is recommended to take 8-12 hour breaks from taking nitrates, but during this period patients are left without drug protection.
S. B. Freeman et al. A placebo-randomized, controlled crossover study compared the effectiveness of beta-blockers, calcium antagonists, and nitroglycerin patches in 52 patients with stable angina. AECGM was used to assess myocardial ischemia. For one week, nitroglycerin or placebo patches were applied at 8 a.m. and removed at 10 p.m. (nitrate-free period was 10 hours per day). ECG monitoring was performed during the last 48 hours of each period to assess ischemia. The average duration of ischemia during this period was the same between active treatment and placebo. 88% of ischemic episodes were asymptomatic. During the period free from the use of a patch with nitroglycerin, the duration of ischemia compared to the ischemia time when using a patch without an active drug increased, respectively, to 46.9 + 17.9 minutes and to 22.5 + 9.2 minutes per day. The opposite pattern was revealed during the period of exposure to a patch with nitroglycerin or placebo: episodes of ischemia lasted 27.5+14 minutes per day and 34.5+11 minutes per day, respectively. Although the differences in the duration of ischemia during the withdrawal of nitroglycerin or placebo did not reach statistical significance, the identified trends indicate the development of a withdrawal syndrome in the form of an increase in periods of ischemia during intermittent therapy with transdermal forms of nitroglycerin.
An increase in ischemic episodes as measured by AECGM during nitroglycerin patch withdrawal compared with placebo patch withdrawal was confirmed in the Second Transdermal Intermittent Dosing Evaluation Study (TIDES-II), a multicenter, randomized, double-blind, placebo-controlled crossover study that included 72 patients with stable angina. The study was carried out against the background of therapy with beta blockers, calcium antagonists or a combination thereof. The incidence of ischemic episodes was lower after discontinuation of placebo patches compared with the period after discontinuation of nitroglycerin patches, respectively, while during the patch period, the incidence of ischemia was lower in the nitroglycerin group compared with placebo, respectively. Indeed, withdrawal syndrome limits the effectiveness of using long-acting nitrates to treat patients with MCI.
Despite the official registration of the metabolic cytoprotective drug trimetazidine for the treatment of coronary artery disease, there is still no evidence of its effectiveness in the treatment of asymptomatic myocardial ischemia. In particular, MSUlgen et al., who assessed the effectiveness of trimetazidine in 64 patients who had suffered myocardial infarction, did not reveal its significant effect on BMI according to ECG monitoring.
The results of randomized clinical trials indicate the importance of treating asymptomatic myocardial ischemia, although a unified treatment strategy has not been developed. Published data are based on studies of a relatively small number of patients with proven CAD. Their results cannot be applied to patients without clear evidence of coronary artery disease. Only a small proportion of patients included in the study were women. There is also a small number of patients with coronary artery disease due to diabetes mellitus. There is no data on the threshold reduction in BIM at which an improvement in prognosis is possible. In the ACIP study, even with revascularization, it was possible to completely suppress ischemia in only 55% of patients, but the prognosis after revascularization after 12 months was significantly better compared to drug therapy.
Studies evaluating the treatment of patients with MCI lack data on the cost-effectiveness of interventions. Although the advisability of ECG monitoring for the detection of myocardial infarction and unstable angina is generally accepted, the role of screening ECG monitoring in patients with stable coronary artery disease or after revascularization procedures has not yet been resolved.
There have been reports that screening with electron beam computed tomography (EBCT) among individuals without clinical manifestations of coronary artery disease can identify patients at high risk of asymptomatic myocardial ischemia. The advantage of EBCT is its high sensitivity, achieved by detecting coronary atherosclerosis and the severity of coronary artery calcification. These data correlate with the results of coronary angiography.
Zuo-Xiang He et al. Over the course of 2.5 years, 3895 individuals without clinical manifestations of coronary artery disease were prospectively examined. All subjects underwent EBCT, and 411 underwent a stress test with myocardial perfusion tomography and a treadmill stress test. The obtained data coincided with the indicators of the coronary artery calcification scale, based on the results of EBCT. Asymptomatic myocardial ischemia was detected in 22% of subjects with signs of coronary artery pathology according to EBCT data. Among individuals with a coronary artery calcification scale value <10, myocardial ischemia was not detected; with a scale value from 11 to 100, it was detected in 2.6%, from 101 to 399 - in 11.3%, and with a scale value of about 400 - in 46% cases (p<0.0001). Indicators of the coronary artery calcification scale predicted the risk of detecting BMI, regardless of the age and gender of patients. EBCT screening testing among asymptomatic individuals at high risk of CAD is considered to be cost-effective.
So, asymptomatic myocardial ischemia is a common phenomenon, the causes of which are not well understood. Its high prognostic value has been established in patients with acute coronary syndrome and acute macrofocal myocardial infarction. In all other clinical situations, data on the role of BIM in risk stratification of patients with coronary artery disease are contradictory and need clarification.
Vladimir ORLOV,
Head of the Department of Clinical
pharmacology and therapy, professor.
Sergey GILYAREVSKY,
Professor of the department.
Russian Medical Academy of Postgraduate Education.