Magnetic resonance imaging is recognized as one of the most informative neuroimaging research methods. During the procedure, detailed layer-by-layer images of the brain are obtained, allowing one to assess the organ’s compliance with standards.
MRI is relevant in the diagnosis of post-traumatic conditions, inflammatory, tumor, and neurodegenerative changes. One of the most severe disorders detected by tomography is brain atrophy. This is a chronic progressive disease accompanied by the death of neurons, a decrease in the volume and density of brain structures.
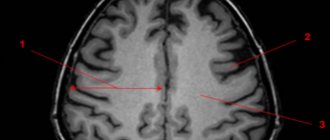
Atrophy of the frontal and temporal lobes on MRI scans
The pathology is based on organic changes in the nervous tissue. The progression of atrophy leads to a decrease in the functionality of the central nervous system. In fact, this means a gradual decline in the work (involution) of the brain until vital processes stop. The prognosis is unfavorable, since the changes are irreversible. Prospects depend on the etiology, form, rate of progression of the disease and the quality of medical care provided.
Using MRI, it is possible to identify and localize these processes in the early stages of development.
Alzheimer's disease
This is a progressive disease with increasing impairment of memory, thinking, intelligence, speech, praxis and recognition, ultimately leading to dementia.
Data on the prevalence of the disease are conflicting. According to some reports, it is 4–5% among people over 60 years of age. The main clinical forms of the disease are Alzheimer's disease itself (with onset mainly in presenile age) and senile dementia of the Alzheimer's type (with onset mainly in old age). An atypical form of the disease with a predominance of frontal lobe atrophy and Alzheimer's type dementia within Down syndrome are also distinguished. Here is a description of the main forms of the disease. 1. Alzheimer's disease . In approximately 80% of cases, it begins at the age of 45–65 years, less often - at the age of about 40 or after 65 years. The duration of the disease is on average 8–10 years, possibly protracted (more than 20 years) and catastrophic (from 2 to 4 years). There are three stages of the disease.
| | Read about diagnosing and treating Alzheimer's disease |
The initial stage includes the stage of “doubtful” dementia and the stage of “mild” dementia. The first stage is manifested by mild disturbances in memory, thinking, speech, praxis, and personality, which are noticeable mainly to the patients themselves and which they manage to hide or compensate for for some time. At the stage of mild dementia, impairments become more serious. Memory for current events decreases, chronological and spatial types of memory suffer.
Violations of various thinking operations are revealed. Disorders of speech, praxis, recognition, and psychopathic personality changes are detected. The severity of the disorders is such that patients can no longer cope independently with professional responsibilities and other types of social activities, such as shopping, paying bills, receiving guests, writing texts, etc.
Patients cope with self-care, although they need outside control and encouragement. Affective and delusional disorders are often observed at this stage. These are subdepressions, sometimes chronic and combined with anxiety, hysteriform and hypochondriacal manifestations; episodic or protracted delusional ideas of damage, theft, less often - ideas of relationship, persecution or jealousy. Some patients show increased exhaustion and headaches; the duration of the initial stage ranges from 4–8 to 15–20 years. At the same time, in some patients, memory impairments predominate, while in another, larger group, focal impairments (aphasia, etc.) prevail.
At the stage of moderate dementia, impairments in the cognitive sphere and higher cortical functions reach a degree where patients can no longer cope with professional and social responsibilities. They need help even with everyday life and self-care. Neurological disorders appear, such as muscle stiffness, akinesia, hyperkinesis, and seizures. A critical attitude towards the disease nevertheless remains. Along with deficient ones, productive disorders are sometimes observed: episodes of hallucinatory confusion, a state of psychomotor agitation, often not associated with a deterioration in the somatic condition. The aphato-apracto-agnostic syndrome (three A syndrome) characteristic of this stage is finally formed, the weakening of memory takes on the character of progressive amnesia. Confabulation and ecmnesia often do not occur.
The stage of severe dementia is characterized by the breakdown of memory, thinking and intelligence, as well as higher cortical functions. Patients need help even with basic self-care. Basically, only in Alzheimer's disease are such profound disturbances, to the point of insanity, observed, as well as fetal position, contractures, multiple violent motor phenomena, violent laughter and crying, and epileptic seizures. At the same time, there are pronounced somatic changes: weight loss, extreme decrepitness, bulimia, endocrine disorders.
2. Senile dementia of the Alzheimer's type. In approximately 80% of cases, it begins between the ages of 65 and 85 years. The duration of the disease ranges from 4 to 15 years or more. In the initial stage of the disease, significant memory impairment for current events develops, often with a revival of memories of the distant past. Thinking operations suffer, as well as intelligence (creativity, planning, forecasting, etc.). Personality changes are characteristic: egocentrism, narrowing of interests, emotional impoverishment, conflict, opposition and suggestibility. Moral decline and disinhibition of drives are also observed.
The suspicion inherent in patients later develops into a tendency to develop delusions. However, half of the patients experience psychotic episodes with low-level delusions. Subdepressive states are also observed, especially gloomy depression. In the second stage of the disease, memory impairment takes on the character of progressive amnesia. There may be scanty confabulations, as well as states of amnestic disorientation with a “shift of the situation into the past.” At the stage of moderate dementia, disorders of higher cortical functions also become clear. At the stage of severe dementia, a complete breakdown of mnestic-intellectual functions is observed, and serious neurological disorders are also detected.
The etiology of Alzheimer's disease has not been established. The role of genetic factors in the development of familial forms of the disease can apparently be considered proven. However, this role remains unclear in sporadic forms, which account for about 90% of all cases of the disease. Aging is essential.
The leading place in the treatment of patients is occupied by replacement therapy aimed at overcoming neurotransmitter deficiency. To compensate for cholinergic deficiency, tacrine, amiridine, exelon, memantine, Aricept, and reminyl may be recommended. To eliminate the deficiency of other neurotransmitter systems, other drugs are recommended, in particular Yumex and Citalopram. To increase the survival of neurons, nootropics are prescribed, especially Cerebrolysin, as well as vasoactive drugs, in particular sermion or nicergoline. Anti-inflammatory treatment such as indomethacin may be helpful. Therapy for psychotic disorders is carried out with the help of antidepressants, antipsychotics, and tranquilizers. The prognosis of the disease is unfavorable.
What atrophies does the brain undergo?
Subatrophic changes in the brain precede global neuronal death. At this stage, it is important to diagnose brain disease in a timely manner and prevent the rapid development of atrophic processes.
For example, with hydrocephalus of the brain in adults, the free voids released as a result of destruction begin to be intensively filled with released cerebrospinal fluid. This type of disease is difficult to diagnose, but proper therapy can delay further development of the disease.
Changes in the cortex and subcortical substance can be caused by thrombophilia and atherosclerosis, which, in the absence of proper treatment, first cause hypoxia and insufficient blood supply, and then the death of neurons in the occipital and parietal zone, so treatment will consist of improving blood circulation.
Alcoholic brain atrophy
Brain neurons are sensitive to the effects of alcohol, so drinking alcohol-containing drinks initially disrupts metabolic processes and addiction occurs.
Alcohol breakdown products poison neurons and destroy neural connections, then gradual cell death occurs and, as a result, brain atrophy develops.
As a result of the destructive effect, not only the cortical-subcortical cells suffer, but also the fibers of the brain stem, blood vessels are damaged, neurons shrink and their nuclei are displaced.
The consequences of cell death are obvious: over time, alcoholics lose their sense of self-esteem and their memory decreases. Further use entails even greater intoxication of the body, and even if a person comes to his senses, he still later develops Alzheimer's disease and dementia, since the damage done is too great.
Multiple system atrophy
Multiple system brain atrophy is a progressive disease. The manifestation of the disease consists of 3 different disorders, which are combined with each other in various ways, and the main clinical picture will be determined by the primary signs of atrophy:
- parksionism;
- destruction of the cerebellum;
- vegetative disorders.
At present, the causes of this disease are unknown. Diagnosed using MRI and clinical examination. Treatment usually consists of supportive care and reducing the impact of the disease's symptoms on the patient.
Cortical atrophy
Most often, cortical atrophy of the brain occurs in older people and develops due to senile changes. Mainly affects the frontal lobes, but spread to other parts is possible. Signs of the disease do not appear immediately, but ultimately leads to a decrease in intelligence and the ability to remember, dementia; a striking example of the influence of this disease on human life is Alzheimer's disease. Most often diagnosed through a comprehensive examination using MRI.
Diffuse spread of atrophy is often accompanied by impaired blood flow, deterioration of tissue repair and decreased mental performance, impairment of fine motor skills of the hands and coordination of movements; the development of the disease radically changes the patient’s lifestyle and leads to complete incapacity. Thus, senile dementia is a consequence of brain atrophy.
The most famous bihemispheric cortical atrophy is called Alzheimer's disease.
Cerebellar atrophy
The disease involves damage and death of small brain cells. The first signs of the disease: incoordination of movements, paralysis and speech disorders.
Changes in the cerebellar cortex are mainly provoked by diseases such as vascular atherosclerosis and tumor diseases of the brain stem, infectious diseases (meningitis), vitamin deficiency and metabolic disorders.
Cerebellar atrophy is accompanied by symptoms:
- speech and fine motor impairment;
- headache;
- nausea and vomiting;
- decreased hearing acuity;
- visual disturbances;
- During instrumental examination, a decrease in the mass and volume of the cerebellum is noted.
Treatment consists of blocking the signs of the disease with neuroleptics, restoring metabolic processes, using cytostatics for tumors, and possibly removing tumors surgically.
Pick's disease
This is a systemic degenerative disease with onset in presenile age, leading to personality and adaptation disorders, and subsequently to total dementia, most often of the frontal and frontotemporal type.
Pick's disease accounts for 0.4 to 2% of all cases of dementia in old age. The prevalence of the disease in people over 60 years of age is about 0.1%. Women get sick slightly more often than men (in a ratio of 1.7:1). The disease begins between the ages of 50 and 70 years. The average duration of the disease is six years.
The disease usually begins gradually and progresses quite quickly. The initial stage of the disease is manifested primarily by personality changes. If the pole of the frontal lobe suffers, then apathy and spontaneity predominate. When the orbital cortex is damaged, a pseudoparalytic syndrome develops with euphoria, disinhibition and impaired abstract thinking; memory does not change significantly. When the temporal lobes are damaged, stereotypies of speech, behavior and movement come to the fore. Other variants of the onset of the disease are much less common: a) asthenia and asthenodepressive symptoms, b) aphasia phenomena, c) psychotic disorders with delusions of persecution, jealousy, harm, d) memory loss, due to which there is a similarity with Alzheimer's disease.
In the middle stage of the disease, against the background of disturbances in the most complex forms of mental activity (planning, forecasting, understanding the meaning of life situations, flexibility, criticality, creativity), focal cortical disorders are also detected. Speech impairments usually predominate. This is dynamic, amnestic or sensory aphasia. Echolalia and standing speech patterns are characteristic. Agraphia, alexia, acalculia, and apraxia are relatively less pronounced. There are attacks of muscle relaxation without complete loss of consciousness, amyostatic syndrome, extrapyramidal hyperkinesis, and rarely spastic hemiparesis. The appearance of epileptic seizures most likely indicates Alzheimer's disease. The initial state is similar in its manifestations to the symptoms of the terminal stage of Alzheimer's disease.
The etiology and pathogenesis of the disease have not been sufficiently studied. Treatment is similar to that for Alzheimer's disease. Relatively early-onset personality and behavioral disorders usually require hospitalization.
Classification
According to the international classification, atrophic lesions are divided according to the severity of the disease and the location of the pathological changes.
Each stage of the disease has special symptoms.
Atrophic diseases of the brain of the 1st degree or subatrophy of the brain are characterized by minor changes in the behavior of the patient and quickly progress to the next stage. At this stage, early diagnosis is extremely important, since the disease can be temporarily stopped and how long the patient lives will depend on the effectiveness of treatment.
Stage 2 of the development of atrophic changes is manifested in a deterioration in the patient’s communication skills, he becomes irritable and unrestrained, and the tone of speech changes.
Patients with degree 3 atrophy become uncontrollable, psychosis appears, and the morality of the patient is lost.
The last, 4th stage of the disease, is characterized by a complete lack of understanding of reality by the patient; he stops responding to external stimuli.
Further development leads to complete destruction; vital systems begin to fail. At this stage, hospitalization of the patient in a psychiatric hospital is highly advisable, as it becomes difficult to control him.
Classification according to the location of the affected cells:
- Cortical atrophy most often develops in older people and lasts as long as a person lives, affecting the frontal lobes;
- Diffuse atrophy of the brain is accompanied by impaired blood supply, atherosclerosis, hypertension and decreased mental abilities. Stage 1 of this form of the disease most often develops in the cerebellum, and then affects other parts of the brain;
- Multiple system atrophy develops as a result of mutations and gene disorders during pregnancy. In this form of the disease, not only the brain is affected, but also other vital systems. Life expectancy directly depends on the degree of mutation of the entire organism and its viability;
- Local brain atrophy of the 1st degree appears as a result of mechanical lesions, strokes, focal infections and parasitic inclusions. Symptoms depend on which part is damaged;
- The subcortical or subcortical form of the disease is an intermediate condition in which the centers responsible for speech and thought processes are damaged.
Huntington's chorea
This is a hereditary neurodegenerative disease in the middle and second half of life with a predominant lesion of the striatal system of the brain and less severe damage to other subcortical nuclei and the neocortex. The main manifestations of the disease are decreased intelligence, psychotic phenomena and choreic hyperkinesis.
Due to the fact that the latter sometimes does not develop even in the later stages, the process is also referred to as “Huntington’s disease”.
The prevalence of the disease reaches 4–8 people per 100 thousand population. Among patients in psychiatric hospitals it is 1%. The peak incidence rate occurs between 35 and 50 years of age. The disease lasts from 1 to 25 years.
In approximately half of the cases, the disease develops “due to a nervous defect” (Davidenkov, 1932) in the form of a personality disorder, mental underdevelopment and motor “moronism” (clumsiness, poor handwriting, etc.). The disease does not have a single development pattern. Choreic dementia is characterized by damage to the most complex forms of intellectual activity and uneven mental performance. Intellectual deficits are believed to be based on gross disturbances of attention and spasmodic loss of direction in the movement of thoughts. As intellectual impairments develop, they move closer to dementia.
Psychotic phenomena are recorded in 60% of patients. In Alzheimer's disease they occur in 43.5%, and in Pick's disease - in 11% of patients (Sternberg, 1967). In the early stages of Huntington's disease, predominantly psychogenic disorders are observed, including depression with apathy, hypochondria, or dysphoria. Paranoid psychoses with delusions of jealousy, persecution, and poisoning are relatively common. Later, paraphrenic states with delusions of grandeur, hallucinatory and hallucinatory-paranoid psychoses may develop. The most common hallucinations are tactile, visceral and fragmentary verbal. Choreic hyperkinesis is usually slow, low-amplitude, separated by large intervals; It is also typical that they include torsion and athetoid components and occur against a background of mild muscle hypotonia. Muscle strength decreases, eyelid ptosis and dysarthria occur.
There are abortive forms of Huntington's disease: a) neurological, with a predominance of akineto-hypertensive syndrome; usually begins early, b) with typical hyperkinesis and minimally expressed mental disorders, c) with minimal hyperkinetic and severe mental disorders, d) stationary forms, in which, despite extensive symptoms, the disease lasts for decades, so that patients die from intercurrent diseases. Most patients die in a state of mental insanity; in the terminal stage of the disease, hyperkinesis usually decreases or stops.
It has been established that predisposition to the disease is inherited in an autosomal dominant manner and usually leads to atrophy of the striatum, and to a lesser extent, the cortex. Men get sick more often. Huntington described the disease in two brothers. In 12 families descended from them, 100 cases of the disease were described.
When treating patients, drugs that block dopamine receptors (phenothiazine derivatives, butyrophenones) or reduce the content of dopamine in tissues (reserpine, methyldopa) are used. Psychotic disorders are an indication for the use of aminazine, tizercin, propazine or teralen, and other antipsychotics. The results of therapy are usually disappointing. The prognosis of the disease is generally unfavorable.
Brain atrophy in children
Depending on the age at which brain atrophy begins, I distinguish between congenital and acquired forms of the disease. The acquired form of the disease develops in children after 1 year of life.
The death of nerve cells in children can develop for various reasons, for example, as a result of genetic disorders, different Rh factors in mother and child, intrauterine infection with neuroinfections, prolonged fetal hypoxia.
As a result of the death of neurons, cystic tumors and atrophic hydrocephalus appear. Depending on where the cerebrospinal fluid accumulates, cerebral hydrocele can be internal, external or mixed.
A rapidly developing disease most often occurs in newborns, in which case we are talking about serious disorders in the brain tissue due to prolonged hypoxia, since the child’s body at this stage of life is in dire need of intensive blood supply, and a lack of nutrients leads to serious consequences .
Parkinson's disease
This is an atrophic disease of the brain in old and senile age, manifested by extrapyramidal and mental disorders, including dementia.
Occurs with a frequency of 0.08 to 0.2%. 11% of patients show symptoms of dementia. Men get sick more often. The disease begins between the ages of 45 and 75 years, more often at 50–65 years. The main symptoms of the disease are tremor, muscle rigidity, hypokinesia, and paralysis. Obligatory disorders also include permanent and paroxysmal autonomic disorders, as well as personality changes in the form of psychopathization. Half of the patients experience depression, including suicidal tendencies. Querulant tendencies, low-grade delirium, and, in later stages of the disease, hallucinosis, visual or tactile, and states of confusion (delirium) may occur. Visceral hallucinosis is very characteristic. In 15–25% of patients, signs of cognitive deficit are detected, and in elderly patients, in addition, defects in memory, praxis and optical-spatial activity are detected. Pictures of dementia resemble those of Alzheimer's disease. Prospective studies have shown that there is a positive correlation between the ilateral presentation of motor disorders and the risk of developing cognitive deficits.
Predisposition to the disease is transmitted in an autosomal dominant manner with 25% penetrance. The main role in the genesis of symptoms is given to dopaminergic dysfunction of the brain, especially neurons of the substantia nigra. Other brain systems, including cortical structures, may also be involved in the disease process.
The leading place in the complex treatment of the disease is occupied by therapy with L-DOPA and drugs containing it (Madopar, Sinemet, Nakom). These drugs are usually combined with the prescription of anticholinergic drugs (midantan, akineton, parkopan, cyclodol, etc.). There is evidence of positive results from the administration of bromocriptine, parlodel, selegiline, Yumex, and cognitive, which increase dopamine levels in the brain. If psychotic disorders occur, it is recommended to prescribe small doses of antipsychotics while simultaneously reducing the doses of antiparkinsonian drugs and detoxification. The prognosis of the disease is determined by the severity of neurological disorders and its progression.
Back to contents
Prevention and treatment
Adhering to simple rules can significantly facilitate and prolong the life of the sick person. After diagnosis, it is best for the patient to remain in his/her familiar environment, as stressful situations can aggravate the condition. It is important to provide the sick person with feasible mental and physical activity.
Nutrition for brain atrophy should be balanced, and a clear daily routine should be established. Mandatory cessation of bad habits. Control of physical indicators. Mental exercises. A diet for brain atrophy consists of avoiding heavy and unhealthy foods, eliminating fast food and alcoholic beverages. It is advisable to add nuts, seafood and greens to your diet.
Treatment consists of the use of neurostimulants, tranquilizers, antidepressants and sedatives. Unfortunately, this disease cannot be completely cured, and therapy for brain atrophy consists of reducing the symptoms of the disease. Which drug will be chosen as maintenance therapy depends on the type of atrophy and what functions are impaired.
Thus, for disorders in the cerebellar cortex, treatment is aimed at restoring motor functions and using drugs that correct tremor. In some cases, surgery to remove tumors is indicated.
Sometimes medications are used to improve metabolism and cerebral circulation, ensure good blood circulation and access to fresh air to prevent oxygen deprivation. Often the lesion affects other human organs, therefore, a complete examination at the Brain Institute is necessary.