In adults, the normal resting heart rate is 60-80 beats per minute. This frequency may increase or decrease due to structural or electrical abnormalities of the heart. Changes may also be caused by certain behavioral or environmental factors. Irregular heart rhythm is accompanied by increased heart rate. This condition is called arrhythmia or dysrhythmia
and manifests itself as a feeling of anxiety, but does not always lead to serious health complications.
Heart rate surges - causes
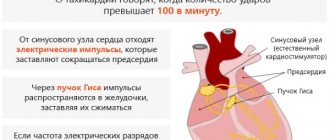
Tachycardia
With tachycardia, the heart rate exceeds 100 beats per minute. There are several types of tachycardia:
Sinus tachycardia
With sinus tachycardia, the heart rate increases, but the heart continues to beat at a normal rhythm. Sinus tachycardia occurs when the heart rate increases for expected reasons, such as during exercise, if a person feels anxious, or during periods of dehydration. Inappropriate sinus tachycardia, which is rare, occurs when the heart rate increases for no apparent reason. This may be the result of a problem with nerve signaling in the heart.
Supraventricular tachycardia
Supraventricular tachycardia is a type of arrhythmia. The word supraventricular means that the arrhythmia originates from the upper chamber of the heart.
The main features of this type of arrhythmia are a sharp increase in heart rate and the persistence of a pathological rhythm for a certain period of time. Supraventricular tachycardia can manifest itself with symptoms such as:
- chest pain
- weakness
- dizziness
- fatigue
- nausea and vomiting
However, sometimes it can be asymptomatic.
Supraventricular tachycardia rarely leads to sudden death.
According to a 2021 study, a patient with supraventricular tachycardia who wants to slow the heart rate can use some type of Valsalva maneuver. To try the most famous type of Valsalva maneuver, a person must push for 10 to 15 seconds. If this method doesn't work, you can try the following types:
- cough
- immersing face in cold water
- blow on the thumb (in children) or into an empty syringe
Atrial fibrillation
Atrial fibrillation occurs as a result of complex waves in the upper and lower chambers of the heart, causing an irregular heartbeat. With atrial fibrillation, the following symptoms are noted:
- cardiopalmus
- shortness of breath during exercise
- exercise intolerance
- dizziness
- difficulty breathing at rest
- fatigue
- chest pain
According to some studies, women with atrial fibrillation are more likely to have symptoms than men.
Treatment for atrial fibrillation may include taking blood thinning medications such as:
- warfarin
- dabigatran
- rivaroxaban
- apixaban
- edoxaban
Surgical treatment of atrial fibrillation:
- ablation
- pacemaker
- and etc.
What are heart failures?
An irregular heartbeat, called an arrhythmia, means it is beating too fast or too slowly with an irregular rhythm.
The basis of arrhythmia is a change in the conditions for the formation of excitation of the heart muscle, as well as a violation of the paths of its distribution. The causes of arrhythmia can be both functional disorders and severe organic lesions of the heart, in some cases, such as congenital structural features of the conduction system of the heart. The state of the nervous system also plays a role in the occurrence of arrhythmia, namely mental and emotional stress, causing changes in the pace, and often in the rhythm, of heart contractions, including in healthy people. Arrhythmia often occurs in people with diseases of the central and autonomic nervous system.
Under the influence of one or more reasons, the functions of the heart are disrupted:
- automaticity (automatic generation of impulses by cardiomyocytes by the pacemaker)
- excitability (the ability of cardiomyocytes to generate an action potential in response to stimulation)
- conduction (impulse conduction through the conduction system of the heart)
- contractility (contraction of contractile cardiomyocytes)
- refractoriness (electrical inertia of the CMC for some time after the impulse is carried out, which does not allow the return of the transmitted impulse and the imposition of a subsequent one)
- aberration (the ability to conduct an impulse along additional pathways of the cardiac conduction system)
The disorder may affect one or more functions of the heart at the same time.
It has a pulse system that tells you when to pump blood to your organs. If there are problems with this mechanism, then interruptions in heart rhythm may occur. Heart rhythm disorders are often called cardiac arrhythmias (this is technically incorrect, as in most cases there is a heart rhythm, but it is abnormal). Cardiac dysrhythmia may be a better term, although it is used much less frequently.
The pulse system of the heart has the following process. The sinus node, sometimes called the SA node, is a special group of cells. It is known as a natural pacemaker and sends an electrical signal to the chambers of the heart that tells them when to contract and push blood through. If the organ is working properly, the electrical signal will travel from the sinus node to the upper chambers of the heart (atria) and then to the lower chambers (ventricles).
Content:
- What are heart failures?
- Symptoms of heart failure
- Types of heart rhythm disturbances
The normal electrical pattern is known as sinus rhythm (usually produces a heartbeat between 60 and 100 beats per minute (bpm) when you are resting - at rest).
Interruptions can be caused by electrolyte abnormalities in the bloodstream, abnormal hormone levels (such as thyroid hormones associated with too high or too low thyroid function), and certain medications. Any abnormality in the electrical cycle in the heart that generates an abnormal rhythm—too fast, too slow, skipped, or irregular—is considered dysrhythmia.
Heart conduction disorders (blocks)
Conduction disorders, particularly blockages, can disrupt the conduction of electrical signals. This disorder affects the rhythm and frequency of the heartbeat, and as a result, the heart cannot pump the amount of blood necessary for the body to function.
Cardiac conduction disorders can manifest as the following symptoms:
- fatigue
- dizziness
- slow heartbeat
- dyspnea
- cardiopalmus
- chest pain
- abdominal pain
- nausea
- fainting
Treatment will depend on the type of blockade and may include medications such as atropine, glycopyrrolate or antiarrhythmic drugs, or surgery such as a pacemaker.
Why does a teenager's pulse fluctuate?
In adolescence, the pulse fluctuates almost every day, and not only against the background of physical activity and any emotional experiences, often the causes of a rapid pulse are:
- active growth of the body - puberty is characterized by uneven growth of muscles, bones and blood vessels;
- hormonal changes in the body - too active production of hormones necessarily affects the heart rate, and the vessels are simply not able to cope with the sudden surge of blood;
- strain on the organs of vision – we are talking about long periods of time at the computer or on the phone.
If pulse fluctuations do not occur regularly, the frequency quickly normalizes, there are no chest pains or headaches, nausea, tremors (trembling) of the limbs, decrease/increase in body temperature, then parents and the teenager himself do not have to worry - this is how the period of active maturation of the body manifests itself.
Dehydration
If a person does not drink enough water, they may become dehydrated. Dehydration can affect a person's mental and physical functioning, including heart rate. According to a 2021 review, some immediate symptoms of dehydration may include:
- decreased physical activity
- decreased thinking ability
- mood change
- fatigue
In the short term, dehydration can cause your heart rate to increase due to the following reasons:
- affects the function of the endothelium, which lines the inner wall of the heart and blood vessels;
- affects the sympathetic nervous system, causing changes in breathing and heart rate;
- affects the body's ability to regulate blood pressure. The person feels dizzy when standing up.
If a person is dehydrated for a long period of time, their risk of developing problems such as heart disease increases.
Apart from drinking water, a person can consume a lot of fruits and vegetables. If symptoms of dehydration occur, oral rehydration solutions can quickly restore electrolyte balance. If the above methods do not help and the symptoms become more severe, intravenous fluid administration is necessary.
Prevention measures
Preventive measures aimed at stabilizing the heart rate will “work” only if they are followed on a regular basis:
- Lose weight - obesity is considered a direct danger to the heart and blood vessels. You need to adjust your diet and regimen, refuse or reduce the amount of fatty, smoked, salty foods and desserts/sweets you consume. You can’t start losing weight suddenly by following some strict diets - this will only worsen the situation, and there will be no results. The best option is to seek help from a nutritionist.
- To refuse from bad habits. We are talking not only about smoking and drinking alcoholic beverages, but also about drinking coffee at night, excessive consumption of drinks with caffeine - these include energy drinks.
- Give your body regular physical activity. Doctors constantly emphasize that in trained people the pulse slows down, and this indicates the strength of the entire cardiovascular system. There is no need to engage in professional sports; even regular walking and simple morning exercises will be useful.
Jumps in pulse and blood pressure may be physiological in nature, but often they are the only symptoms of the development of serious pathological conditions. If your heart rate increases regularly, you should contact a cardiologist for examination, because the lack of qualified medical care can lead to heart attacks and strokes, coronary heart disease and myocarditis.
Medicines
Some drugs can affect your heart rate and may cause abnormal heart rate. Some types of medications that can cause tachycardia:
- anesthetics
- antiarrhythmic drugs
- antibiotics
- antitumor drugs
- antidepressants
- thyroid hormone medications
- stimulant drugs
A person with atrial fibrillation should be careful when taking the following medications, such as:
- Antiarrhythmic drugs, including: adenosine
- amiodarone
- flecainide
- propafenone
Lack of sleep
Sleep deprivation can negatively impact your heart rate and blood pressure. Getting enough rest is important for the body to function properly. Symptoms of sleep deprivation include:
- fatigue
- irritability
- difficulty concentrating
Insufficient sleep can increase your risk of developing conditions such as high blood pressure and obesity. Sleep deprivation can also lead to conditions such as atrial fibrillation.
The following habits can help you sleep better:
- reducing caffeine intake
- developing a specific sleep pattern
- getting enough physical activity during the day
Stress
The interaction between the heart and brain causes the body to respond to certain emotions, such as anger, depressed mood and stress. According to a 2014 article, negative emotions cause disproportionately more activity in the right hemisphere of the brain. To explain this, the heart must change the way it beats, causing disproportionate or extra beats. This makes the electrical signals unstable and, as a result, can cause arrhythmia.
Stress can manifest itself in a range of physical and mental symptoms, including:
- anxiety
- feeling depressed
- headache
- cardiopalmus
- nausea
- fatigue
- insomnia
Stress management can be important in reducing the risk of developing arrhythmia. Stress reduction and relaxation techniques, such as meditation, can be effective forms of treatment.
Symptoms of heart failure
Symptoms of an irregular heart rhythm depend on what type of arrhythmia you have. The most common ones are:
- palpitations (a fluttering or fluttering feeling in the chest);
- dizziness;
- dyspnea;
- feeling tired;
- fainting.
There are many factors that can cause your heart rate to go wrong. The main causes of abnormal heart rhythms are:
- electrical impulses that come from a part of the heart other than the sinus node (the place in the heart where natural electrical impulses are normally generated)
- electrical impulses originate from the sinus node, but go to the lower parts of the heart;
- an abnormality in blood chemistry levels.
Some abnormal heart rhythms are inherited. If this is the case for this condition, your doctor may talk to you about checking other family members (this will help them know if they need treatment now or in the future).
Heart rhythm disturbances can arise from problems within the heart itself or be the result of abnormalities in the body's environment that directly affect the heart's ability to conduct impulses. The heart muscles become irritated when they are not filled with oxygen. This can happen during a heart attack in which the coronary arteries, the blood vessels that supply blood to the heart, are blocked. Lack of oxygen can occur when the lungs are unable to naturally extract oxygen from the air. Significant anemia or low levels of red blood cells reduces oxygenation of the blood and may prevent adequate oxygen delivery. Heart rate is associated with "electrical wiring" problems with the impulse pathways in the heart. This causes a “short circuit,” in which the heart speeds up and beats 150 or more beats per minute. The abnormality is triggered by a physical factor, such as that seen in Wolff-Parkinson-White syndrome, or occurs with changes in electrical physiology between several cells (in atrial flutter).
Having different rhythms throughout the day is absolutely normal for the human heart. It will be slower when you are resting, but may become faster when you are physically active or excited about something. Many people experience heart palpitations at some point in their lives and describe it as a feeling like everything inside is pounding or fluttering. For most people, an abnormal heart rate is unpleasant, but it is harmless and does not always mean obvious problems with the body. You may feel like your heart skipped a beat or had an extra beat - this is called an ectopic beat (very common, harmless, no treatment required).
Talk to your doctor about abnormal heart rhythms if:
- intermittent heartbeat lasts a long time and does not improve or worsen;
- Along with palpitations, you begin to feel weak or dizzy;
- you have a history of heart problems;
- you are worried about your heart palpitations.
The specialist will discuss your symptoms with you and decide whether an ECG is needed to assess your heart rate and rhythm.
However, the initial symptom of dysrhythmia is often palpitations, a feeling that the heart is beating too fast or slow, irregular, or skipping rhythm. The fluttering may be intermittent and will require medical intervention to resolve. Abnormal heart rhythm causes other symptoms of decreased cardiac output (the amount of blood the heart pumps out to meet the body's need for oxygen and energy). The patient may complain of dizziness, weakness, nausea and vomiting, chest pain and shortness of breath.
In critical situations, the patient may fall to the ground or lose consciousness. This may be due to a life-threatening pathology (ventricular fibrillation or ventricular tachycardia), due to rapid heart contractions (there is not enough blood pressure to supply the brain with oxygen). The same result can occur if the heart beats too slowly and insufficient blood pressure is generated.
Fast heart rhythms occur due to environmental problems that affect the heart. They may be intrinsic to the body, such as anemia, abnormal electrolyte or thyroid hormone levels, triggered by reactions to external stimuli (caffeine, alcohol, over-the-counter cold remedies, or stimulants such as amphetamines). For the heart muscle cell, all drugs look like adrenaline substances, which cause irritation of the cells.
Your doctor may recommend an ECG, echocardiogram, or electrophysiology test to help diagnose an abnormal heart rhythm. Depending on its type, the specialist will prescribe the use of the medicine to stop, prevent or control. If necessary, they may suggest a procedure such as cardioversion or catheter ablation, or surgery to insert an implantable cardioverter defibrillator or pacemaker.
When to see a doctor
If your heart rate and rhythm become irregular or cause alarming symptoms, it is important to seek medical help. Even if there is no danger, your doctor can help reduce the risk of complications. If you notice the following symptoms, you should call emergency help:
- chest pain
- dyspnea
- dizziness
- feeling of impending doom
- pain in the following places: neck
- one or both hands
- jaw
- stomach area