It branches like a tree, first into large branches (trunks), then into smaller branches and twigs, and is conventionally divided into several parts or sections:
- 1. The ascending aorta is the area from the aortic valve to the brachiocephalic trunk.
- 2. The aortic arch is a short section from which all the vessels supplying the arms and head (brachiocephalic arteries) depart. They anatomically form an arch connecting the ascending and descending aorta.
- 3. The descending (thoracic) aorta begins from the mouth of the left subclavian artery and continues to the diaphragm.
- 4. Below the diaphragm and before the bifurcation of the aorta (bifurcation) is the abdominal aorta.
Dividing the aorta into sections is very important for assessing risk and choosing optimal treatment tactics in patients with aortic aneurysms.
An aortic aneurysm is an area of local expansion.
Which method of diagnosing aortic anomalies to choose: MRI, CT, ECHO-CG, angiography
Selection Methods
- ECHO CG in young children,
- MRI examination in adults.
What will a chest x-ray show?
Double aortic arch:
- Soft tissue compaction on both sides of the trachea
- Bilateral narrowing of the trachea.
Retroesophageal right aortic arch:
- Soft tissue compaction to the right of the trachea
- Narrowing of the trachea or displacement of the trachea on the right side.
What will fluoroscopy with barium show in case of anomaly of the aortic arch?
- Anterior view demonstrates bilateral esophageal narrowing at various levels
- The lateral view demonstrates marked posterior narrowing of the esophagus.
Why is ultrasound of the heart and aorta performed for arch abnormalities?
- Two separate aortic arches, each giving rise to the carotid and subclavian arteries.
What MRI and MSCT images of the heart and aorta will show
- May demonstrate double or right aortic arch
- The right arch is often larger (75%)
- The right duta is often located posteriorly and superiorly and often passes behind the esophagus.
Diagrammatic representation of a double aortic arch with a predominance of the right arch.
The right aortic arch (arrow) in a 36-year-old man. A chest x-ray demonstrates displacement of the trachea to the left side.
How to recognize a vice?
Diagnosis of the defect is not difficult even during pregnancy. This is especially true in cases where the right aortic arch is combined with other, more severe anomalies of heart development. However, to confirm the diagnosis, a pregnant woman is repeatedly examined, including with expert-class ultrasound machines, and a council of geneticists, cardiologists and cardiac surgeons is assembled to make a decision on the prognosis and the possibility of delivery in a specialized perinatal center. This is due to the fact that with some types of defects combined with the right aortic arch, the newborn baby may require heart surgery immediately after delivery.
Regarding the clinical manifestations of the right aortic arch, it should be mentioned that an isolated defect may not manifest itself at all, only sometimes accompanied by frequent obsessive hiccups in a child. In the case of a combination with tetralogy of Fallot, which accompanies the defect in some cases, the clinical manifestations are pronounced and appear in the first days after birth, such as increasing pulmonary heart failure with severe cyanosis (blue discoloration of the skin) in the baby. That is why tetralogy of Fallot is classified as a “blue” heart defect.
What screening shows a defect in pregnant women?
The diagnosis of a right-sided aortic arch can be made already at the first screening, that is, at 12-13 weeks of pregnancy. More accurate information about the condition of the fetal heart can be obtained at the second and third screening ultrasound examinations (20 and 30 weeks of pregnancy).
An analysis of fetal DNA can further clarify the absence of a connection between the formation of a right-sided aorta and severe genetic mutations. In this case, chorionic villus material or amniotic fluid is usually collected through a puncture. First of all, DiGeorge syndrome is excluded.
Two techniques
Aortic rupture can be prevented with surgery. Until 1995, in Russia they were made only in one way: they opened the peritoneum, cut out the deformed section of the aorta, and replaced it with a prosthesis made of durable synthetic material the size of a healthy aorta. The full course of recovery after such an operation takes 2-3 months. The success rate of treatment is 90%. Since 1991, it has become possible to perform operations using the endovascular method, that is, intravascularly. What does it look like? Incisions are made in the femoral arteries, through which surgeons insert the components of the prosthesis, packaged in a delivery device with a diameter of 7-8 mm (and the normal width of the aorta is 2 cm), and pull these parts along a path 30-40 cm long to the desired section of the abdominal aorta. And already there, inside the aorta, the prosthesis is assembled. The endoprosthesis consists of a mesh frame that supports the diameter of the vessel and a thin synthetic material that does not allow blood to pass through. All these manipulations are carried out under fluoroscopy control. Fantastic? Surgeons say: “The technique is simple.” True, endoprostheses are not produced in Russia, and they are not cheap; they are made to individual standards in the West. But there are no quotas for such gentle, non-traumatic, modern operations; the state does not pay for them. Therefore, up to 90% of operations for aortic anervism are still performed in our country using an open surgical method.
Chance find
Ultrasound of the abdominal organs
- Cost: 3,800 rub.
More details
The difficulty of diagnosing this disease is that at the first stage there are no signs of ill health. The only symptom you can pay attention to is pulsation in the abdomen. It's like there's a heart beating there. Aortic rupture often occurs suddenly, without any warning signs, and is fatal in half of the cases. An aortic aneurysm usually turns out to be an “accidental finding” - during an ultrasound of the abdominal cavity, a study related to some other problem, the doctor sees that the aorta in the abdominal region is dilated. Nowadays, the majority of patients with this diagnosis are military personnel. All of them, both those who are still serving and those who are already retired, undergo regular medical examinations. During such preventive examinations the disease is discovered. It is a pity that our medical examination does not apply to all citizens. Then there would be fewer sudden deaths from aneurysms.
Aortic aneurysm
The aorta is the largest, most powerful blood vessel in the human body. Powerful, therefore, it seemed that nothing “took” him. However, aortic aneurysm is the scourge of modern cardiovascular surgery. In normal conditions, in adult women and men, the diameter of the lumen of the ascending aorta is about 3 cm, the descending part is 2.5 cm, the abdominal segment of this large vessel is even smaller - 2 cm. The diagnosis of an aneurysm is announced only if the diameter of the affected aorta increases by 2 or more times compared to the norm.
An aneurysm is an abnormal bulge that occurs in the walls of an artery. The walls of the arteries are quite thick and strong, the muscle fibers of which they are composed allow them to withstand intense blood pressure. However, if there is a weak area in the artery wall, the pressure causes the area to bulge, thereby forming an aneurysm.
An aortic aneurysm can develop in two parts of this artery:
- the abdominal part passing through the lower part of the abdominal cavity is an abdominal aortic aneurysm;
- A thoracic aortic aneurysm developing in the chest cavity. This type of aneurysm is less common, but both types are equally dangerous to human health and life.
Depending on the appearance, the aneurysm can be: 1. fusiform 2. saccular.
Small aneurysms usually pose no threat. However, they can increase the risk of: the formation of atherosclerotic plaques at the site of the aneurysm, which cause further weakening of the artery walls; formation and separation of a blood clot, therefore increasing the risk of stroke; an increase in the size of the aneurysm, which means compression of nearby organs, which causes pain; aneurysm rupture. The main complication of aneurysms of any location is their dissection followed by possible rupture (mortality rate - 90%).
Causes and risk factors
The main causes of aneurysm are diseases and conditions that reduce the strength and elasticity of the vascular wall:
- atherosclerosis of the aortic wall (according to various sources, from 70 to 90%); inflammation of the aorta (aortitis) of a syphilitic, giant cell, mycotic nature;
- traumatic injury;
- congenital systemic connective tissue diseases (for example, Marfan or Ehlers-Danlos syndrome);
- autoimmune diseases (nonspecific aortoarteritis);
- iatrogenic causes caused by medical manipulations (reconstructive operations on the aorta and its branches, cardiac catheterization, aortography).
Risk factors for the development of atherosclerosis and aneurysm formation:
- male gender (the incidence of aneurysms in men is 2–14 times higher than in women);
- smoking (during screening diagnostics of 455 people aged 50 to 89 years in the Department of Vascular Surgery of the Moscow Regional Research Clinical Institute, it was revealed that 100% of patients with abdominal aortic aneurysms had a smoking history of more than 25 years, and as a result of the Whitehall study it was proven that life-threatening complications of aneurysms occur 4 times more often in smokers than in non-smokers);
- age over 55 years;
- family history;
- long-term arterial hypertension (blood pressure above 140/90 mm Hg);
- physical inactivity;
- excess body weight;
- increased blood cholesterol levels.
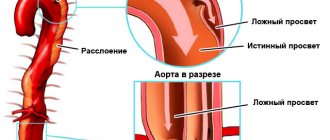
They also talk about a dissecting aneurysm, which is formed as a result of rupture of the inner membrane with its subsequent dissection and the formation of a second false channel for blood flow.
Depending on the location and extent of the dissection, 3 types of pathology are distinguished: 1. Dissection begins in the ascending aorta and moves along the arch (50%). 2. Dissection occurs only in the ascending aorta (35%). 3. Dissection begins in the descending aorta and moves down (more often) or up (less often) along the arch (15%). Depending on the duration of the process, a dissecting aneurysm can be: acute (1–2 days from the appearance of the endothelial defect); subacute (2–4 weeks); chronic (4–8 weeks or more, up to several years).
SYMPTOMS OF AN AORTIC ANEURYSM
Aortic aneurysm manifests itself in different ways - it mainly depends on the size of the aneurysmal sac and its location (below is a visual clinical picture using the example of an aneurysm of the sinus of Valsalva). In some cases, no symptoms are observed at all (in particular, before the aneurysm ruptures, but this will be a different diagnosis), which makes early diagnosis difficult. The most common complaints from patients with an aneurysm of the ascending aorta: pain in the chest (in the area of the heart or behind the sternum) - due to the fact that the aneurysmal protrusion presses on nearby organs and tissues, as well as due to the pressure of the blood flow on thinned and weak wall; shortness of breath, increasing over time; feeling of palpitations (“As if something is pounding in the chest” - a comment from patients); dizziness; with large aneurysms, attacks of headaches, swelling of the soft tissues of the face and upper half of the body are disturbing - due to the development of the so-called superior vena cava syndrome (because the aneurysm presses on the superior vena cava).
An aortic arch aneurysm is characterized by:
- difficulty swallowing (due to pressure on the esophagus);
- hoarseness of the voice, sometimes coughing - if the aneurysm puts pressure on the recurrent nerve, which is “responsible” for the voice;
- suddenly increased salivation and slow pulse - if pressure spreads to the vagus nerve, which controls salivation and pulse rate;
- strained breathing, and later shortness of breath if the trachea and bronchi are compressed by a huge aneurysm;
- unilateral pneumonia - if an aneurysm, pressing on the root of the lung, interferes with its normal ventilation, then, as a result, congestion occurs in the lungs, which, when an infection occurs, develops into pneumonia.
With an aneurysm of the descending aorta, the following appear:
- pain in the left hand (sometimes up to the fingers) and shoulder blade;
- with pressure on the intercostal arteries, a lack of oxygen supply to the spinal cord may develop, which is why paresis and paralysis are inevitable;
- in case of constant long-term pressure of a large aneurysm on the vertebrae, they may even be displaced;
- in milder cases, due to pressure on the intercostal nerves and arteries - pain, as with radiculitis or neuralgia.
The most common complaints with an aneurysm of the abdominal aorta:
- a feeling of fullness in the stomach and heaviness in the epigastrium (upper floor of the abdomen), which the patient initially tries to explain by overeating or stomach pathology;
- belching;
- in some cases, reflex vomiting (appears as a reaction to the pressure of the aortic aneurysm on nearby organs and tissues);
- When palpated, a tense, tumor-like pulsating formation is felt. Sometimes patients can independently detect this pulsation.
DIAGNOSIS OF AORTIC ANEURYSMS AND ITS COMPLICATIONS
An aortic aneurysm in the period before rupture has rather meager clinical manifestations: murmurs that are heard on auscultation; the doctor listens not only to the chest, but also to the abdominal cavity; a tumor-like pulsating formation, which is found with deep but careful palpation (sometimes it is actually regarded as a tumor, since it is quite dense to the touch); incomprehensible discomfort at the site of aneurysmal protrusion formation. Therefore, to clarify the pathology before it “gives birth” to dangerous complications, instrumental diagnostic methods are used: fluoroscopy and radiography of the chest and abdominal cavity - they visualize a tumor-like formation (its pulsation is visible during fluoroscopy); echocardiography - if an aneurysm of the ascending aorta is suspected; Doppler ultrasound (USDG) - for signs of aneurysm in other parts of the aorta; CT and MRI.
TREATMENT AND SURGERY FOR AORTIC ANEURYSM
If an aneurysm is diagnosed, but its progression is not observed, doctors adopt conservative tactics: further careful observation by a vascular surgeon and cardiologist - monitoring the general condition, blood pressure, pulse, repeated electrocardiography and other more informative methods to monitor the possible progression of the aneurysm and notice in time the prerequisites for complications of an aneurysm; antihypertensive therapy - in order to reduce blood pressure on the thinned wall of the aneurysm; anticoagulant treatment - to prevent the formation of blood clots and possible subsequent thromboembolism of medium and small vessels; reducing the amount of cholesterol in the blood (using both drug therapy and diet). Surgical intervention is resorted to in the following cases: large aneurysms (at least 4 cm in diameter) or with a rapid increase in size (by half a centimeter in six months); complications that threaten the patient’s life - aneurysm rupture and others; complications that, although not critical from the point of view of death, sharply reduce the patient’s quality of life - for example, pressure on nearby organs and tissues, which causes pain, shortness of breath, vomiting, belching and similar symptoms.
PROGNOSIS FOR AORTIC ANEURYSM
Aortic aneurysm is a nosology that should be constantly under close monitoring by doctors. The reason is possible complications, which in most cases threaten human life. Over time, the aneurysm progresses morphologically (the altered wall becomes thinner and thinner, the protrusion increases). The life and health of a patient can be saved only through careful monitoring of the course of the disease and, if necessary, immediate surgical intervention.
PREVENTIVE MEASURES
Prevention, thanks to which it is possible to prevent the occurrence of aortic aneurysm in healthy people, is nonspecific (that is, effective not only in the case of this pathology) and includes: complete cessation of smoking; reducing alcohol standards to the level of “only for holidays”, or better yet, a complete refusal; physical education and sports; elimination of factors that cause a rise in blood pressure (stress, kidney disease); treatment and prevention of pathology that contributes to the formation of aortic aneurysm (atherosclerosis); immediate alertness in the event of a sudden, at first glance inexplicable appearance of interruptions in the functioning of the heart, gastrointestinal tract and respiratory system and immediate examination by specialized specialists to exclude an aortic aneurysm; regular, high-quality, not just for show, medical examinations with a vascular surgeon and cardiologist. If an aortic aneurysm is already present, preventive measures are indicated in order to prevent complications of this disease: well-chosen anticoagulant therapy to prevent the formation of blood clots in the lumen of the aneurysm; a significant reduction in physical activity - otherwise they can cause overstrain of the thinned wall of the aneurysm, which will result in its rupture; sometimes a complete refusal of physical activity is necessary until the doctor clarifies the diagnosis and assesses the risk; antihypertensive treatment - thanks to it, it is possible to avoid an increase in the pressure of the blood flow on the thinned wall of the aneurysm, which can rupture at any moment; careful psychological control - in some patients, even minor stressful situations pushed the aortic aneurysm to rupture.
Translated from Greek
The diagnosis is called abdominal aortic aneurysm
. Aneurysm in Greek means “dilation.” Blood running through the aorta creates pulsating pressure on the walls and, if the walls have lost their elasticity, they stretch in some places, the aorta expands, and “bags” can form on one of its sides, which sometimes break through. This happens much more often in the abdominal aorta than in any other part. The cause of an aneurysm may be congenital weakness of connective tissue. Hypertension affects the stretching of the walls, when the pressure in the vessels exceeds the norm. Atherosclerosis complicates the situation; in one of its types, the walls of blood vessels degrade, and the vessels themselves dilate. Aneurysm develops with age and is more often found in people over 60 years of age, mainly in men. Women suffer from this disease less often because they are less likely to suffer from atherosclerosis, and hormones protect them from it.
Introduction
Congenital obstruction of the aortic arch or its interruption diagnosed in the neonatal period most often requires urgent surgical correction [1]. At the present stage of development of cardiac surgery, the accumulated data allows us to talk about significant progress both in the performance of reconstructive operations themselves for congenital diseases of the aortic arch, and in their postoperative results. Currently, all attention should be directed to improving long-term treatment outcomes, because these treatment outcomes are not completely satisfactory. For example, in one quarter of all operated patients, arterial hypertension develops in the later stages of observation against the background of systemic vascular dysfunction, although they do not have signs of anatomical obstruction of the aortic arch [2, 3]. Data have been obtained allowing us to conclude that it is in this cohort of patients that functional, structural and macroanatomical disorders of the heart and great vessels are most often diagnosed [4–6]. Due to a complex of disorders affecting the structure of the vascular wall, cellular activation mechanisms are triggered, which ultimately leads to the early manifestation of signs of atherosclerosis of large vessels (aorta, coronary arteries), the formation of aortic aneurysms and peripheral arteries, and in almost 20% of operated patients, death occurs in young and middle age (30-35 years) [7].
Causes of aortic aneurysm in the abdominal region
Experts identify several reasons for the formation of an abdominal aortic aneurysm:
- heredity (it is worth undergoing additional examinations if one of your close relatives had such a diagnosis);
- trauma or surgery on the aorta;
- atherosclerosis (approx. link to article);
There are also risk factors for aneurysm formation:
- smoking,
- excess weight,
- high blood pressure,
- The disease is most often encountered by men over 50 years of age.
Quitting smoking and maintaining a normal weight remain factors that you can get rid of, protecting yourself from the risk of not only an aneurysm, but also other serious diseases.