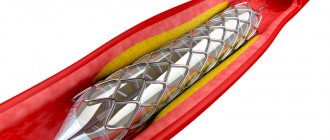
“High cholesterol” does not hurt, but it can lead to the development of atherosclerosis. Atherosclerosis affects the cardiovascular system, leading to the formation of atherosclerotic plaques and blood supply disorders. This often ends in heart attacks and strokes.
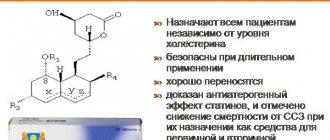
Today there are many drugs from the statin group. They have been shown to be effective in reducing mortality from cardiovascular disease, but debate continues about their safety. To achieve and maintain the desired levels of lipid metabolism, long-term use of drugs is required, but many patients do not follow the recommendations, causing the effectiveness of treatment to sharply decrease. What to say about patients when doctors have different opinions on this matter.
What are statins
Statins are a group of lipid-lowering drugs. They slow down the work of one of the main enzymes involved in the synthesis of cholesterol - HMC-CoA reductase. This leads to a decrease in cholesterol synthesis in the liver.
A decrease in cholesterol synthesis in hepatocytes increases the number of receptors for low-density lipoproteins (LDL-C) and their subsequent uptake from the bloodstream. In addition, there may be some reduction in the formation of LDL due to inhibition of the synthesis in the liver of their precursor, very low density lipoproteins (VLDL). Thus, statins help reduce total cholesterol, LDL cholesterol and VLDL cholesterol in the blood plasma. At the same time, drugs in this group can reduce the level of TG and slightly increase the level of “good cholesterol” (high-density lipoproteins). The effectiveness of lowering blood cholesterol levels depends on the dose of the drug. To obtain the desired level of reduction, fairly high doses are required.
Their numerous additional properties also contribute to the benefit of statins:
- improving the functional activity of the endothelium;
- stabilization of atheroma (atherosclerotic plaque);
- anti-inflammatory, immunomodulatory and antithrombotic effects;
- positive effect on bone metabolism.
The effect of statins on the body
- Statins are also called HMG-CoA reductase inhibitors. The second name reflects their operating principle. The drugs have the ability to block one of the enzymes, without which the chemical compound of cholesterol is impossible.
- Sterol gets a bad rap, but the human body needs it. It is an essential component of cell membranes, the main material for the synthesis of vitamin D and steroid hormones.
- To prevent a deficiency of this substance, the body finds reserve sources of cholesterol. For example, statins increase the confluence of lipoproteins with a high density of HDL, which helps improve the walls of blood vessels and prevents the formation of blood clots.
Action
Indications
Drugs in this group are prescribed only by a doctor and he selects which active ingredient is suitable and its dosage. Usually, for this purpose, the risk of cardiovascular events is determined using a special scale, questionnaire, and tests are taken to determine the lipid spectrum and biochemical blood parameters. Today, statins are prescribed not only after heart attacks and strokes as secondary prevention. Under certain high-risk conditions, a doctor may use statins in the primary prevention of cardiovascular disease.
Use of atorvastatin in patients with coronary heart disease and acute coronary syndrome
The randomized GREACE trial in patients with documented coronary artery disease demonstrated the ability of escalating doses of atorvastatin (from 10 to 80 mg, mean dose 24 mg) to reduce overall and cardiovascular mortality by 43% (p = 0.002) and 47% (p = 0.00). 0017) respectively. Taking atorvastatin was accompanied by a reduction in the incidence of cardiovascular events (MI, unstable angina, repeated myocardial revascularization) by 54% (p<0.0001) and cerebral strokes by 47% (p=0.034) [5].
The double-blind, randomized TNT (Treating to New Target) study in patients with documented coronary artery disease (n=10,001) assessed the effectiveness of different doses of atorvastatin (10 and 80 mg). Thus, on therapy with atorvastatin 80 mg, the primary endpoint (cardiovascular death, non-fatal MI, cardiac arrest with resuscitation, stroke) was identified in 8.7% of patients, and on therapy with atorvastatin 10 mg - in 10.9%. In summary, patients receiving atorvastatin 80 mg had a 22% lower risk of major events than patients receiving atorvastatin 10 mg (odds ratio (OR) 0.78, 95% confidence interval (CI) 0.69–0 .89, p<0.001) [6, 13].
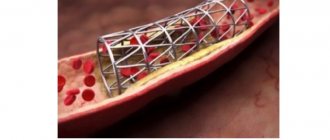
The ability of high doses of atorvastatin 80 mg to reduce the incidence of ischemic events compared with endovascular treatment was demonstrated in the AVERT (Atorvastatin Versus Revasculatization Treatment) study in 341 patients with stable CAD. Patients treated with atorvastatin 80 mg for 18 months had a 36% lower incidence of ischemic events than patients on standard therapy who underwent percutaneous coronary intervention (PCI) (p=0.048). Thus, aggressive statin therapy may be as effective as endovascular treatment in reducing the incidence of ischemic events in patients with CAD [8].
The effectiveness of the original atorvastatin at a dose of 80 mg as secondary prevention of CVD was also assessed in patients with acute coronary syndrome (ACS). Thus, in the randomized, double-blind MIRACL (Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering) study of 3086 patients with ACS (unstable angina or acute non-ST segment elevation MI), the primary endpoint (death, non-fatal MI, cardiac arrest with resuscitation, or resumption of episodes of myocardial ischemia requiring readmission) was achieved in 228 patients (14.8%) in the atorvastatin group and 269 patients (17.4%) in the placebo group (RR 0.84, 95% CI 0.70–1.00 , p=0.048). There was also a lower incidence of symptomatic myocardial ischemia requiring emergency readmission in the atorvastatin group compared with placebo (6.2% vs. 8.4%, p=0.02) [7]. In 171 patients with ACS in the ARMYDA-ACS (Atorvastatin Pretreatment Improves Outcomes in Patients With Acute Coronary Syndromes Undergoing Early Percutaneous Coronary Intervention) study, atorvastatin reduced the risk of 30-day cardiovascular events after endovascular treatment by 88% compared with the group placebo (in the case of atorvastatin therapy 12 hours before endovascular intervention with 40 mg perioperatively) (OR 0.12, 95% CI 0.05–0.50, p = 0.004) [14].
Another study, PROVE IT-TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy Thrombolysis in Myocardial Infarction 22 Investigators), assessed the effectiveness of atorvastatin 80 mg and pravastatin 40 mg in 4162 patients undergoing PCI due to the development of ACS. Compared with pravastatin 40 mg, atorvastatin 80 mg was associated with a reduction in the composite endpoint of death, MI, stroke, unstable angina leading to hospitalization, and revascularization within 30 days of endovascular treatment (21.5% vs. 26.5%, OR 0.78, 95% CI 0.67–0.91, p=0.002), as well as rates of infarction-related revascularization (11.4% vs. 15.4%, p=0.001) and non-infarction -connected arteries (8.0% vs. 10.5%, p=0.017) [15]. Based on this study, it was concluded that atorvastatin therapy reduces the incidence of major adverse cardiovascular events in patients with ACS undergoing PCI.
Minuses
But there are also unresolved issues in statin treatment. Thus, from 40 to 75% of patients stop taking statins within 1-2 years after starting treatment. Patients name the reasons for this: fear of developing undesirable effects from the instructions for the drug (46%), disbelief that the medicine prolongs life (29.4%), taking a large number of other pills (27.6%), forgetfulness (26.5 %), poor control of blood cholesterol levels while taking medication (18.8%), drug withdrawal by a non-attending physician (13.5%). At the same time, the actual development of undesirable effects on statin therapy was observed only in 11.7% of patients, and their manifestations were mild and moderate in severity.
Muscle symptoms
The incidence of symptoms of muscle damage is 7-29%, according to various sources. These include:
- muscle pain;
- muscle weakness;
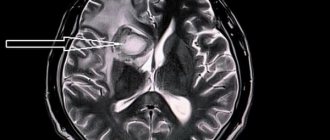
- muscle inflammation, determined based on examination of a sample of muscle tissue and/or magnetic resonance imaging (MRI);
- myonecrosis - muscle damage, determined by a significant increase in serum creatine kinase (CK) levels;
- rhabdomyolysis - destruction of muscle tissue with acute kidney damage with an increase in serum creatinine;
- autoimmune myopathy is a rare complication accompanied by severe muscle damage even after discontinuation of the drug;
The reasons for this are not well understood. According to one version, there is a decrease in coenzyme Q10 in muscle tissue and a decrease in the level of vitamin D. The work of mitochondria is affected.
Muscle symptoms occur in 7-29%.
Symptoms usually appear in both arms or legs. The period of appearance is about 4-6 weeks after starting to take statins. Sometimes, with diseases of the joints and ligaments, pain increases. This may be due to muscle weakness. Unusually, physically active people are more likely to suffer from muscle symptoms. One study found that athletes were less tolerant of lipid-lowering therapy.
According to research, these symptoms are rare. But the studies themselves often exclude older patients, those with impaired liver and kidney function, and those taking certain medications, that is, it cannot be said that this is an ordinary elderly person with a “bouquet of diseases.”
Diabetes mellitus and insulin resistance
It has been established that long-term use of statins under certain factors can contribute to the development of insulin resistance and diabetes mellitus. This is evidenced not only by research data, but also by national recommendations of some countries.
Risk factors for developing diabetes when taking lipid-lowering drugs may include:
- high body mass index (BMI);
- elderly age;
- heart failure;
- myocardial infarction in the last six months and high cardiovascular risk;
- family predisposition to type 2 diabetes;
- Asian race;
- smoking, alcohol abuse.
Effects on the liver
When taking statins to reduce the negative effect on the liver, you must avoid taking:
- alcohol;
- drugs that are metabolized in the liver along the same pathways (for example, amiodarone, sulfonamides, methyldopa, cyclosporine).
Statins can negatively affect a damaged liver.
They should not be prescribed for active viral hepatitis until liver parameters return to normal.
Drug interactions
Statins have multiple effects. This is due to the fact that they do not act in isolation, but affect many chemical reactions in the body. This is especially important in patients taking multiple medications for cardiovascular diseases.
How to take statins: before or after meals?
- Food does not have any significant effect on the absorption of satins. Diet plays a big role. The effectiveness of statins can be easily negated by food. To do this, it is enough to add foods high in cholesterol, trans fats, saturated fats, and sugar to the menu.
- The products do not affect the absorption of dietary sterol. A large amount of cholesterol in the body compensates for the lack of synthesis through food. And as a result, the sterol level does not decrease.
- A prerequisite is the exclusion from the diet of alcoholic beverages , which cause a strong blow to the liver. Added to this is the medication burden. Smoking also has a negative effect on lowering cholesterol because nicotine damages the vascular system.
- While taking statins of the 1st-3rd generation, drinking grapefruit juice . It contains substances that block the transport enzyme needed to remove the drug from the body. The amount of medication in the blood increases, which causes side effects.
- An exception is the drug lovastatin. It is taken during dinner.
Safety of atorvastatin use
However, despite irrefutable evidence of the benefits of statins, many patients, especially those with high and very high cardiovascular risk, do not achieve target LDL cholesterol levels, do not prescribe combined lipid-lowering regimens, or use a course of drugs due to the development of possible complications of statin therapy.
Currently, there are a large number of studies in which the original atorvastatin convincingly demonstrates safety and good tolerability in doses from 10 to 80 mg.
In the SPARCL trial, which assessed the safety of atorvastatin 80 mg with a median follow-up of 4.9 years, the incidence of adverse events in the statin group was comparable to that in the placebo group. In the atorvastatin group, serious side effects were detected in 17.5% of patients, in the placebo group - in 14.5%. The incidence of myalgias, myopathies and rhabdomyolysis was also comparable to the placebo group (5.5% versus 6.0%, 0.3% versus 0.3%, 0.1% versus 0.1%, respectively). During atorvastatin therapy, increased levels of liver transaminases were more often recorded (2.2% in the atorvastatin group and 0.5% in the placebo group) [24]. In the TNT study, the incidence of transaminase elevations was higher in the atorvastatin 80 mg group than in the atorvastatin 10 mg group (1.2% vs. 0.2%, p < 0.001) [6]. The safety of long-term use of atorvastatin was further demonstrated in a meta-analysis by Newman et al. (2006), based on 49 completed studies involving 14,236 patients who received treatment for an average of 2 weeks. up to 52 months [26]. The safety of atorvastatin 10 mg (n=7258), atorvastatin 80 mg (n=4798) and placebo (n=2180) was assessed. The study also analyzed the incidence of side effects, the incidence of CK elevations above 10 upper limit of normal (ULN) and liver transaminases above 3 ULN. The incidence of side effects was comparable in all 3 groups. Discontinuation of the drug due to the development of side effects was observed in 2.4, 1.8 and 1.2% of patients in the atorvastatin 10 mg, atorvastatin 80 mg and placebo groups, respectively. Serious adverse events were rare and infrequently led to discontinuation of treatment at any dose. Skeletal muscle side effects with atorvastatin, such as myalgia, were observed in 1.4, 1.5 and 0.7% of patients in the groups, respectively. There were no cases of rhabdomyolysis in the groups. Hepatic transaminases were increased more than 3-fold in 0.1, 0.6 and 0.2% of patients in the study groups, respectively [26]. The clinician should be aware of the possible interactions of atorvastatin with drugs that are metabolized by CYP450 [27].
Statins for cardiovascular diseases
WOSCOP (West of Scotland Coronary Prevention Study). The West of Scotland study was the first randomized placebo-controlled trial of primary prevention of coronary artery disease in middle-aged men at high risk of coronary atherosclerosis and with hypercholesterolemia (LDL cholesterol ≥5 mmol/l). Pravastatin 40 mg/day was compared with placebo. The study lasted 5 years and included 6595 people. During the study, in the group taking pravastatin, LDL cholesterol levels were reduced by 26%, the incidence of deaths and non-fatal MI decreased by 31%, the need for coronary artery bypass grafting decreased by 37%, and mortality from all causes decreased by 22%. Long-term follow-up of study participants showed that the effect of treatment persisted after 5 and 10 years, despite the fact that after the end of the study, the treatment of participants in the main and control groups did not differ [].
According to the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS), lovastatin was shown to reduce the likelihood of a first coronary attack (unstable angina, fatal and non-fatal myocardial infarction, sudden cardiac death) in patients of both sexes with low risk, without clinical signs of cardiovascular disease and close to average LDL levels of 3.9 (3.4 - 4.9) mmol/l. For every 1000 patients treated with lovastatin for 5 years, 12 myocardial infarctions and 17 coronary revascularization procedures were prevented. The drug had no effect on overall mortality.
Similar results were obtained in the ASCOT-LLA study, which examined the effects of simvastatin (10 mg) in a group of men and women with relatively normal serum cholesterol levels who had hypertension and at least three additional CVD risk factors.
The JUPITER study examined the use of rosuvastatin at a dose of 20 mg per day in healthy young patients of both sexes with elevated C-reactive protein levels and LDL levels below 3.4 mmol/l and showed a significant reduction in the primary endpoints: cardiovascular complications (acute myocardial infarction, unstable angina , sudden cardiac death) and death from all causes (hazard ratios 0.56 and 0.80, respectively).