Causes of plaques in the carotid arteries
The formation of cholesterol plaques in the carotid arteries is one of the forms of systemic atherosclerosis, rarely occurring in isolation.
As a rule, atherosclerosis of the brachiocephalic arteries (brachio - shoulder, cephalis - head (Greek)), which includes the carotid arteries, is combined with atherosclerosis of the aorta, coronary arteries, and arteries of the lower extremities. Atherosclerosis
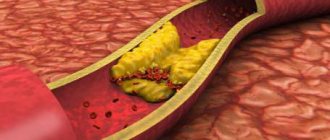
- a chronic disease of arteries of the elastic and muscular-elastic type, arising as a result of lipid metabolism disorders and accompanied by the deposition of cholesterol and some fractions of lipoproteins in the intima of blood vessels. Deposits form in the form of atheromatous plaques. The subsequent proliferation of connective tissue in them (sclerosis), and calcification of the vessel wall lead to deformation and narrowing of the lumen up to obliteration (blockage). It is impossible to name one single reason leading to atherosclerotic restructuring of the artery wall and the formation of atherosclerotic plaques.
Most researchers agree with the fact that atherosclerosis is based on a violation of fat metabolism (more precisely, cholesterol esters) at the level of genetic predisposition. Familial hypercholesterolemia (FH) is a known disease. This is a disease caused by a decrease in the rate of removal of low-density lipoprotein (LDL) from the bloodstream due to mutations in the specific LDL receptor gene. Familial hypercholesterolemia is the most common genetic disease due to a single gene mutation (monogenic disease). The modern medical scientific community, based on numerous studies, considers risk factors to be the main triggers for the progression of atherosclerosis (an increase in the size and number of plaques).
Atherosclerosis. Episode I: The Hidden Menace of Plaques
“O pessimum periculum quod opertum latet. The most terrible danger is the hidden danger.” Publilius Syrus
Atherosclerosis is a chronic vascular pathology that is the cause of most ischemic damage to the cardiovascular system. The term “atherosclerosis” was introduced in 1904 by Marchand and substantiated by the experimental studies of N. N. Anichkov, therefore it is also called Marchant-Anichkov disease. The “victims” are mainly arteries of the elastic and muscular-elastic type. The evolution of the pathological cascade includes the formation of endothelial dysfunction, massive deposition of lipids in the intima, exacerbation of innate and adaptive immune responses, proliferation of smooth myocytes of the vascular wall and remodeling of the extracellular matrix. These processes lead to the formation of atherosclerotic plaque (ASP), the morphological substrate of atherosclerosis (Fig. 1) [1]. .
Figure 1 | Scheme of etiopathogenesis of atherosclerosis
Exposure to cardiovascular disease risk factors (CVD risk factors) causes endothelial dysfunction and increases the permeability of the vascular wall, allowing the invasion of atherogenic lipid fractions (low density lipoproteins (LDL) and very low density lipoproteins (VLDL)). Endotheliopathy also promotes monocyte recruitment, migration, and adhesion. Once in the intima, monocytes differentiate into macrophages and absorb modified lipids, turning into foam cells. Simultaneously, in this first stage of the disease, smooth muscle cells (SMCs) migrate into the intima, where they synthesize elements of the extracellular matrix (ECM) and contribute to the formation of the fibrous capsule. As atherosclerotic plaque (ASP) grows, the number of SMCs decreases and the foam cells undergo apoptosis, releasing active metalloproteinases that destroy the fibrous membrane, increasing the susceptibility of the plaque to rupture. There is a change from a stable ASB subtype to an unstable one. The immune system (innate and acquired immunity) is actively involved in this process and plays a key role in plaque vulnerability [1].
It contains a lipid, or, to be more precise, atheromatous (Greek athḗra, “gruel”) core, built from modified lipids, proteins, their breakdown products, cholesterol crystals, fragments of macrophages and smooth muscle cells with connective tissue growing around it ( sklḗrōsis, “hardening”) - fibrous cap [2].
During the atherosclerotic process, stages are revealed, with characteristic pathomorphological manifestations (Table 1) [2].
Table 1 | Pathomorphological classification of atherosclerotic lesions. Comparison of macro- and microscopic stages of the process [2]
The morphological features of the plaque determine the degree of its “danger” to the body. Violation of the integrity of the ASP leads to thrombogenic damage. In order to predict and determine the correct treatment strategy, formed ASPs are divided into stable and unstable (Fig. 2, 3). The main characteristics for classification are the structure of the fibrous cap and the size of the lipid core [3]. .
Figure 2 | Sections of a coronary artery with damaged, unstable and stable atherosclerotic plaques
Left: rupture of the fibrous cap of the plaque (red arrow) with superimposition of atheromatous masses and thrombus formation (Tp). In the center: atherosclerotic plaque (ASP) with a thin fibrous cap - an unstable subtype. Inside the plaque there is a large atheromatous core (AN) with hemorrhages (hemorrhages). White arrows indicate the thinnest part of the fibrous cap. Right: stable ASP, the tegmentum is mainly composed of fibrous tissue with partial calcification (black arrows) [3].
Figure 3 | Microphotographs of the lumen of a coronary artery with varying degrees of stenosis severity
A-C: atherosclerotic plaque (ASP) with cap rupture in mild, moderate and severe stenosis, respectively (the severity of stenosis was calculated by the diameter of the lumen (luminal stenosis)). A: non-occlusive thrombus. B and C: occlusive thrombus. D–F: unstable ASP with mild, moderate and severe stenosis, respectively. The atheromatous core (AN) is covered with a thin fibrous cap; blood clots are not detected in the lumen. GI: stable ASP with mild, moderate and severe stenosis, respectively. The AG is absent or small in size, and calcification (Ca++) is often observed [3].
Stable plaques have a well-defined dense fibrous cap without thinning throughout, as well as a small atheromatous core. Some plaques, instead of an atheromatous core, have deposits of calcium salts (petrificates) at their base. The thickened fibrous cover of the plaque indicates a good reparative function of the intimal smooth muscle elements. The cover of stable plaques is mainly represented by dense connective tissue with compactly located collagen fibers, with a meager amount of lipids and cellular elements [4].
Activated macrophages located in the ASP secrete destructive metalloproteinases that break down the collagen and elastin of the fibrous cap of the plaque. The predominance of this function aggravates the destructive processes in the plaque core. This is how a vulnerable unstable plaque (vulnerable unstable plaque) is formed (Fig. 4) [5]. In such a plaque there is a high probability of the formation of a thrombogenic site. Criteria for an unstable vulnerable plaque: the presence of a thin fibrous cap (less than 65 µm) with pronounced infiltration by inflammatory cells (T-lymphocytes and macrophages), a large lipid core occupying more than 30% of the total area of the plaque, massive neovascularization, with the occurrence of hemorrhages from pathologically formed neovessels, abundant infiltration of foam cells. It has also been suggested that the presence of multiple areas of microcalcification (as opposed to large homogeneous foci of calcification) in the fibrous cap may increase the risk of rupture. .
Figure 4 | "Virtual histology" - data from optical coherence tomography
A: Thin capsular fibroatheroma (yellow arrows) is an atherosclerotic plaque with a fibrous cap <65 µm overlying a prominent lipid core. B: Damaged plaque - with rupture of the fibrous cap (red arrows) and formation of a cavity (red asterisk) within the plaque. C: Microchannels (white arrows). D: Clusters of macrophages appear as bright spots with high signal dispersion (yellow arrows). E: Cholesterol crystals are thin linear areas of high signal intensity within the plaque (red arrows). F: Thrombus is an unformed mass protruding into the lumen of the vessel, size ≥ 250 µm (white arrows) [5].
Vulnerable unstable plaques vary in their “weak link.” There are fibroatheroma with a thin fibrous cap (lipid type), plaques with a high proteoglycan content and a pronounced inflammatory reaction, which leads to erosion and thrombosis (inflammatory-erosive type) and plaques with necrosis/calcinosis (dystrophic-necrotic type) [6].
Timely visual examination of the structure of ASP allows us to move away from the concept of “symptomatic” and “asymptomatic” plaques, forming an idea of the potential of a particular plaque before the development of a critical situation. It is most important to find out the state of the fibrous cap and the level of activity of necrotic processes in the core of the plaque. Predictors of the highest risk of ischemic complications are the presence of hemorrhages, ulcerations and thinning of the ASP cap, blood clots and other embologenic material (sometimes these can be fragments of calcifications) on the lumenal (facing the lumen of the vessel) surface of the plaque.
Sources:
- Badimon L., Vilahur G. Thrombosis formation on atherosclerotic lesions and plaque rupture. J Intern Med. 2014;276(6):618-32.
- Simionescu M., Sima AV Morphology of Atherosclerotic Lesions. In: Wick G, Grundtman C (eds) Inflammation and Atherosclerosis. Springer, Vienna.2012:19-37.
- Tian J. Distinct morphological features of ruptured culprit plaque for acute coronary events compared to those with silent rupture and thin-cap fibroatheroma: a combined optical coherence tomography and intravascular ultrasound study. J Am Coll Cardiol. 2014;63(21):2209-16.
- Rognoni A. et al. Pathophysiology of Atherosclerotic Plaque Development. Cardiovasc Hematol Agents Med Chem. 2015;13(1):10-3.
- Narula J. et al. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol. 2013;61(10):1041–1051.
- Lee KY, Chang K. Understanding Vulnerable Plaques: Current Status and Future Directions. Korean Circ J 2019;49(12):1115-1122.
Risk factors
- smoking (the most dangerous factor);
- hyperlipoproteinemia (total cholesterol > 5 mmol/l, LDL > 3 mmol/l, Lp(a) > 50 mg/dl);
- arterial hypertension (high blood pressure) (systolic blood pressure > 140 mm Hg; diastolic blood pressure > 90 mm Hg);
- diabetes;
- obesity;
- physical inactivity (sedentary lifestyle).
Without correction of risk factors, in the presence of a predisposition to atherosclerosis, cholesterol deposits gradually increase in the walls of the arteries. For clinical manifestations of atherosclerosis, a narrowing of any large artery by more than 50% is necessary. It is at this stage that patients most often seek medical help. Plaques in the carotid arteries are most often located in the cervical segment of the artery, over a short distance. The key point in determining the severity of damage to the internal carotid artery is the percentage of narrowing (stenosis) of its lumen, in relation to the normal lumen located behind the plaque. Numerous studies have proven that stenosis of the internal carotid artery by more than 70% increases the risk of ischemic stroke by 5 times, compared with a lesser degree of stenosis. The brain receives its main blood supply from two internal carotid and two vertebral arteries. Stenosis of the artery by more than 70% leads to a change in the local parameters of the blood flow - they can be compared with the flow of river water in places where the channel narrows - seething, turbulence, chaotic impacts of blood into the vessel wall lead to microthrombosis, trauma to the vessel wall, destruction of unstable plaques and its detachment particles. Particles of plaques and blood clots freely located in the bloodstream are called emboli. Following the bloodstream, the embolus gets stuck in smaller branches located in the brain, causing ischemia of areas of the brain and leading to its death.
Symptoms of atherosclerotic plaques in the carotid artery
The presence of atherosclerotic plaques in the vessels supplying the brain is often difficult to suspect, because complaints are varied and inconsistent. In addition, for clear symptoms to appear, there must be pronounced narrowing of the arteries. It is necessary to suspect the presence of atherosclerosis of the carotid arteries in the presence of risk factors, as well as diseases of the heart and blood vessels of the lower extremities. Currently, the main symptoms are considered to be the presence of small and large ischemic strokes, as well as general cerebral symptoms.
- Transient ischemic attacks (TIA)
occur when small fragments of an atherosclerotic plaque break off and enter small vessels of the brain, causing brain death in a small area. In this case, transient paralysis of the arms and/or legs (from several minutes to several hours), speech impairment, transient or sudden blindness in one eye, memory loss, dizziness, and fainting are possible. The presence of a TIA is a serious sign of a high risk of developing a severe stroke in the near future and requires immediate medical attention.
- Acute ischemic cerebrovascular accident (ACVA)
– a consequence of acute blockage of a large branch of the internal carotid artery, which led to the death of neurons and loss of some functions in the brain. In a third of all cases, a stroke leads to death. In most all cases, severe disability after a stroke forever changes the life of a person and his relatives.
- Chronic cerebrovascular insufficiency
– a decrease in blood flow to the brain due to narrowing of the arteries, forcing brain cells to be in constant tension of all intracellular systems and intercellular connections. Symptoms are non-specific, they can be noise in the head, dizziness, flashing “spots” before the eyes, unsteadiness when walking, etc.
Surgery to remove plaque from the internal carotid artery (eversion carotid endarterectomy)
Unfortunately, there are no drugs yet that can “dissolve” or eliminate plaques in blood vessels. Modern drugs can only stop the growth of atherosclerotic plaques and reduce the likelihood of blood clots. The main and only effective treatment for narrowing of the arteries is surgery. Numerous studies involving many countries have indisputably proven the effectiveness of preventive surgical methods in preventing stroke. It is important to understand that surgical intervention is performed if there are strict indications for surgery, and does not replace the treatment of systemic atherosclerosis.
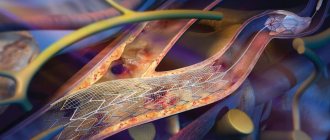
One of the ways to eliminate stenosis of the internal carotid artery is the operation of eversion carotid endarterectomy.
- Under the safest anesthesia (usually a local anesthetic), a small incision (4-6 cm) is made in the neck in the area of the carotid artery.
- Under threefold magnification, with the help of special instruments, the arteries are separated from the surrounding structures (nerves, veins).
- The resistance of the brain to temporary compression of the carotid artery is checked using several techniques. If there is the slightest suspicion that the brain will not be able to withstand clamping of the carotid artery, a special temporary shunt is installed to ensure blood supply to the area of the operated artery. The arteries are pinched.
- The internal carotid artery is dissected transversely and the outer layer of the artery is everted from the plaque like removing a stocking from a leg, after which the atherosclerotic plaque is removed from the vessel along with the inner layer.
- All plaque remnants freely lying in the lumen of the vessel are carefully removed and the outer layer of the artery is returned to its previous position.
- The integrity of the vessel is restored with a continuous suture. The threads used for sutures are thinner than 1/10 mm and are non-absorbable.
- Once the suture is completed, air is released from the artery and blood flow is restored. After checking the sutures for tightness and the absence of sources of bleeding, the wound is sutured layer-by-layer with a cosmetic suture.
Throughout the operation, the patient remains conscious, and verbal and eye contact is always maintained. The duration of the entire operation is 1-2 hours; in the postoperative period, long-term observation and treatment in the intensive care unit is not required. The perioperative protocol at our institution allows patients to be discharged the next day after surgery, which has a beneficial effect on early rehabilitation and prevents the occurrence of infectious complications.
Stroke
Stroke is the main cause of disability in the population. Only about 20% of surviving patients can return to their previous jobs. At the same time, a stroke imposes special obligations on the patient’s family members and places a heavy socio-economic burden on society.
Ischemic stroke
- This is the death of parts of the brain due to insufficient blood supply to them through the arteries. The brain receives nutrition from two carotid and two vertebral arteries. About 80% of ischemic strokes occur due to damage to the carotid or vertebral arteries in the neck. The vast majority of narrowings of the arteries arise due to the deposition of atherosclerotic plaques in the vessel wall, which not only cause insufficient blood flow to the brain, but are also destroyed with the formation of small or massive blood clots, causing either an extensive stroke or many small ones, leading to a significant decrease in intelligence and dementia.
The presence of atherosclerotic plaques in the vessels supplying the brain is often difficult to suspect, since the complaints are varied and inconsistent. The main precursors to the development of a major stroke are the so-called transient ischemic attacks (TIA), which occur when small fragments of an atherosclerotic plaque tear off and enter small vessels of the brain, causing brain death in a small area. In this case, transient paralysis of the arms and/or legs (from several minutes to several hours), speech impairment, transient or sudden blindness in one eye, memory loss, dizziness, and fainting are possible.
Presence of TIA
- This is an alarming warning signal that your brain is in serious danger and you need to undergo examination and begin treatment as soon as possible.
Modern capabilities of cardiovascular surgery make it possible to save life and improve its quality for most patients and to prevent ischemic disorders of cerebral circulation. The clinic's cardiovascular surgeons have modern equipment, unique plastic materials and surgical treatment technologies in their arsenal. In some cases, intravascular elimination of narrowing of the carotid artery is possible without anesthesia and an incision through a puncture of the artery and the introduction of a special instrument into its lumen under X-ray control.
How to get an eversion carotid endarterectomy service (removal of carotid artery plaques)
Indications for surgical treatment of atherosclerosis of the internal carotid arteries are determined by a cardiovascular surgeon; however, to successfully perform the operation and minimize the risk of complications, coordinated interaction between a neurologist, cardiologist, and anesthesiologist is necessary. Our institution employs just such a team of professionals who are ready to help every patient in the fight against cardiovascular diseases. By making an appointment with a cardiovascular surgeon at the clinic, you will receive comprehensive information about the methods of modern diagnosis and treatment of diseases of the carotid arteries, determine the need and timing of surgical intervention. The modern technologies used and the experience of our specialists will help in getting rid of narrowing of the carotid arteries, preventing strokes and maintaining an active and fulfilling life.
Diagnosis of carotid artery stenosis
To determine whether you have stenotic lesions of the carotid arteries or not, your doctor will examine you.
Even if you have no symptoms, your doctor may hear a murmur over your carotid arteries caused by blood flowing through the stenotic area.
If necessary, you will be prescribed Doppler ultrasound of the main arteries of the head (USDG MAG), electroencephalography of the brain (EEG) or computed tomography (CT).
For a more detailed assessment of the condition of the carotid arteries, your doctor may recommend an angiography (x-ray examination of blood vessels).
This study is performed by catheterization, usually of the femoral artery, under local anesthesia in a special operating room equipped with an angiography unit.
After the examination, the doctor will determine the presence of a lesion and choose the optimal treatment method for you.
Basic methods of treating atherosclerosis of the brachiocephalic arteries
Unfortunately, there are no drugs yet that can “dissolve” or eliminate plaques in blood vessels. Some drugs, such as aspirin and cholesterol-lowering drugs, can only stop the growth of atherosclerotic plaques and reduce the likelihood of blood clots. The main and only effective method of treating narrowing and occlusion of the carotid, vertebral, and subclavian arteries is surgery. Numerous studies by scientists from various countries have indisputably proven the effectiveness of preventive surgical methods in preventing stroke.
Open operations can be as follows:
- classic carotid endarterectomy with artery patch plasty,
- eversion carotid endarterectomy,
- internal carotid artery replacement,
- carotid-subclavian shunting.
Minimally invasive methods:
- carotid angioplasty with stenting,
- stenting of the subclavian artery,
- vertebral artery stenting.
The choice of treatment method is based on a comprehensive examination of the patient and is prescribed based on many factors, according to strict indications based on Russian national recommendations for the management of patients with vascular arterial pathology.