Leukocytes are white nucleated blood cells that are the main components of the immune system.
They are formed in the red bone marrow. Their main task is to protect the body from foreign particles that lead to infections, inflammation and allergies.
The reference (acceptable) values of leukocyte content for adults are 4.0 – 9.0 x 109 U/l. In children, the norm depends on age.
An increase in the number of leukocytes in the blood above acceptable values is called leukocytosis.
Leukocytosis can be of two types: physiological (normal) and pathological. They differ in the reason for their occurrence, the mechanism of development, the duration of preservation and their significance for the body. Let's look at each separately.
Read more about blood tests in our article
“Hematological tests: norms and interpretation of results.”
What are leukocytes needed for? General description and main functions
Leukocytes, called white cells, are a whole group of human blood cells. By the way, it is not by chance that they are called white - they do not have their own coloring.
The main function of these structures is protection. Leukocytes are capable of movement and can penetrate into the intercellular space through the capillary wall. These cells absorb foreign particles (including pathogenic structures), neutralizing and digesting them.
Normally, the level of leukocytes in the blood of an adult woman ranges from 4-9·109/l. If after childbirth this indicator changes, this may indicate an inflammatory process.
How the research works
The study is carried out in laboratory conditions. The biological fluid is studied in detail under a microscope and using special test strips. All data is recorded on a special form. On average, the duration of the study does not exceed a day. In case of high urgency (when the doctor needs to establish a diagnosis as quickly as possible), the laboratory works out of turn and conducts the study as quickly as possible - within several hours.
The general analysis is assessed by a specialist according to several criteria - physical and chemical.
Physical parameters include liquid color, presence/absence of sediment, density.
Chemical parameters include a more detailed study of the biomaterial using almost twenty indicators, including a specialist determining acidity, concentration, and foreign inclusions.
Why are leukocytes in the blood elevated after childbirth? List of physiological reasons
Elevated leukocytes in the blood after childbirth do not always indicate the presence of some kind of pathology. The reasons may be completely natural, physiological in nature.
In order to bear and give birth to a child, a woman’s body adapts: changes in hormonal levels are observed, an increase in blood volume, etc. Immediately before childbirth, leukocytes begin to accumulate in the area of the uterus, stimulating the contraction of its muscles and preventing the penetration of infection. This is why the number of white blood cells increases by about 20-30%.
Childbirth is associated with tissue damage to one degree or another. That is why elevated leukocytes in the blood after childbirth (especially if the child was born via cesarean section) are considered quite normal. This helps speed up the tissue healing process, prevent infection and the development of further complications. In most cases, the number of white blood cells in the mother's body returns to normal 3-6 days after the birth of the baby.
Physiological leukocytosis
Associated with the redistribution of leukocytes, they move from the parietal pool (reserve) into the general bloodstream.
Physiological types of leukocytosis include:
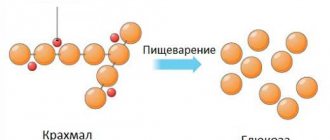
- Digestive. 2-3 hours after eating, leukocytes are released from the depot into the blood, and it flows to the gastrointestinal tract for better digestion. Immune cells are necessary for the submucosal layer of the stomach and intestines for protection, since microorganisms contained in the air, water and on products enter the body with food.
- Myogenic (muscular). Intense muscle work triggers a cascade of reactions, stimulating the work of all organs, tissues and cells. During and after physical activity, the number of white blood cells can be 3-5 times higher than normal.
- Elevated leukocytes during pregnancy are a necessary measure to protect the mother’s body from infection entering the blood. If in the first trimester leukocytosis is relative, but by the third trimester the leukocytes exceed the norm by 2 times and this is not considered a pathology. In addition, leukocytes are involved in stimulating uterine contractions during childbirth.
- In the first 2-3 days of life, elevated leukocytes in a child are the norm. During pregnancy, the mother's immune system protects the fetus. After birth, all formed elements are actively released into his blood from the depot. Leukocytes are necessary to protect the child’s body from an aggressive external environment.
- Painful. When pain receptors are irritated, blood vessels constrict, blood pressure and adrenaline levels increase. This is a stress reaction, in response to which leukocytes are redistributed and released from the parietal reserve into the blood, leading to short-term leukocytosis.
- Stress. Emotional outbursts cause changes in blood vessels, hormonal surges, increased blood pressure and heart rate. In response to this, the number of leukocytes in the blood increases, as during painful stimulation.
With physiological leukocytosis, there is a slight increase in the number of leukocytes without changes in the leukocyte formula (the ratios of all 5 fractions of leukocytes). This phenomenon is short-term and harmless.
Elevated leukocytes in the blood after childbirth
The reasons for this phenomenon, as already mentioned, may be different. If changes in the blood count are observed a week after the birth of the child, then this is no longer considered normal and requires additional diagnostic measures. Why are leukocytes in the blood elevated after childbirth? The cause in this case is an inflammatory process, the focus of which can be located in any part of the woman’s body.
If the number of white blood cells exceeds 4-9·109/l, then this may indicate the presence of problems such as:
- inflammation of the endometrium lining the uterine cavity (endometritis is considered a very common postpartum complication);
- mastitis (inflammation of breast tissue) is also a very common complication after childbirth;
- postpartum ulcers that develop in the presence of tears and cracks;
- lactostasis (stagnation of milk in the mammary glands leads to inflammation if it is not eliminated in time);
- inflammation of the bladder (cases of postpartum cystitis are often recorded in medical practice).
In the most severe cases, an increase in white blood cell levels indicates the development of sepsis. This is a very serious, rapidly progressing disease that often leads to death.
Gestational glomerulonephritis after childbirth
Gestational glomerulonephritis after childbirth
Glomerulonephritis during pregnancy is an acute or chronic immunoinflammatory disease with damage to the glomerular apparatus of the kidneys (glomeruli), as well as involving the tubules and interstitial tissue, which occurs before or during pregnancy.
More than half of the cases are asymptomatic. It may be manifested by a change in the color of urine to pink, reddish or brown, swelling of the face, limbs and body, increased blood pressure with dizziness, headaches, and weakness. Chronic glomerulonephritis is a group of morphologically heterogeneous renal pathologies, and can be both independent diseases and secondary to many systemic diseases, such as systemic lupus erythematosus, systemic vasculitis, hemorrhagic vasculitis, etc. The severity of the prognosis for this pathology is determined by the progression of the disease with the development of nephrosclerosis and terminal chronic renal failure. During pregnancy, both activation and manifestation of chronic glomerulonephritis can be observed. The most severe category is patients with chronic glomerulonephritis (primary or secondary) with a clinical and laboratory picture of nephrotic syndrome. The main symptom of damage to the glomeruli of the kidneys is proteinuria. Nephrotic syndrome is characterized by severe proteinuria (>3.5 g/day), hypoalbuminemia (serum albumin <25 g/l), hyperlipidemia and edema. Massive loss of protein in the urine leads to a decrease in the oncotic pressure of the blood plasma and the movement of the liquid part of the blood into the interstitial space. Edema develops, which varies in severity from pastiness of the face and feet to anasarca with the presence of fluid in the abdominal and pleural cavities. Edema is usually combined with oliguria and even anuria with weight gain. Nephrotic syndrome is always a reflection of severe kidney damage.
Patient K., 34 years old, was admitted to the nephrology department No. 1 of city clinical hospital No. 52 on July 4, 2019, with complaints of a sharp decrease in the amount of urine, severe swelling of the torso, legs, and arms.
From the anamnesis it is known: until 2021, she did not notice any health problems. In 2021, episodes of palpitations began to bother me; upon examination, an atrial septal defect, pulmonary hypertension (MPAP 32 mm Hg), and extrasystole were diagnosed. Metoprolol 12.5 mg was prescribed.
In December 2021, pregnancy occurred. In the 1st trimester, the course of pregnancy was complicated by the threat of miscarriage; she underwent inpatient treatment in a hospital in the Moscow region. The pregnancy was saved.
At the end of May 2021, the patient noted darkening of urine and decreased urine output. June 13, 2021 hospitalized in a Moscow city hospital.
Diagnosis on admission: Pregnancy 28 weeks, threat of premature birth. Gestational pyelonephritis.
Urine tests revealed for the first time severe proteinuria of the nephrotic level: an increase in protein content in the urine to 3.0 g/l (with the norm being up to 0.03). Antibacterial (with a diagnosis of gestational pyelonephritis), magnesium and antispasmodic therapy was carried out.
After discharge from the hospital, swelling of the torso, legs and arms began to increase, and she gained 14 kg in weight. Due to severe edematous syndrome, June 28, 2021. hospitalized by ambulance to the perinatal department of the Moscow city hospital.
Diagnosis on admission: Pregnancy 30 weeks. Head presentation. Moderate preeclampsia. Gestational pyelonephritis. Regional State Administration. Uterine fibroids. NMPC 1A art.
Upon admission, attention was drawn to pronounced nephrotic syndrome (total protein 48.7 g/l, albumin 23.2 g/l, proteinuria 3.4 g/l) with unchanged urinary sediment (leukocyturia 0-1 in the subcutaneous area, erythrocyturia 2-3 in p/z). Mild anemia was noted (hemoglobin 114 g/l). At the same time, blood pressure was normal, renal function was satisfactory (creatinine 62 µmol/l, urea 6.6 mmol/l), there was no liver damage (bilirubin 3.6 µmol/l, AST 20.4 units, ALT 18 units), platelet level within normal limits (platelets 277×109/l.).
The question of early (i.e., up to 36 weeks inclusive) delivery in patients with CGN most often arises in the case of unresolved gestational exacerbation or rapid progression of glomerulonephritis with a decrease in renal function - in each subsequent analysis, an increasingly higher level of protein in the urine is revealed.
A pregnancy of 29-30 weeks, moderately severe preeclampsia, and polyhydramnios was diagnosed. Due to the lack of effect from the therapy, taking into account severe proteinuria, oliguria, June 29, 2021. Emergency delivery was performed by cesarean section and myomectomy. A live premature boy was born, 1400 g, Apgar scores 5-6-7). Antibacterial and anticoagulant therapy and albumin transfusions were carried out. Severe nephrotic syndrome persisted, with proteinuria increasing to 18.6 g/l. Due to severe nephrotic syndrome, hyperhydration before anasarca, lack of positive dynamics after delivery, for further treatment July 4, 2021. the patient was hospitalized in the nephrology department No. 1 of City Clinical Hospital No. 52 and, due to the severity of her condition, was transferred to ICU No. 2 (resuscitation and intensive care unit for nephrological patients).
Diagnosis upon admission to the nephrology department No. 1 of City Clinical Hospital No. 52: Nephropathy in pregnant women. Nephrotic syndrome. Condition after delivery on June 12, 2019.
Upon admission to the ICU, proteinuria reached 44.31 g/day. Against the background of worsening nephrotic syndrome, there was a progressive critical decrease in total protein in the blood serum to 33.5 g/l, albumin to 17.5 g/l, and an increase in cholesterol to 11.8 mmol/l. This condition was complicated by the development of renal failure with oligoanuria and an increase in blood creatinine to 140 µmol/l.
When analyzing the clinical and laboratory picture, a differential diagnosis of the genesis of nephrotic syndrome was made. Obviously, this pathology could not be explained by preeclampsia. Firstly, the severity of nephrotic syndrome did not correlate with clinical and laboratory manifestations of preeclampsia (absence of arterial hypertension, normal platelet levels, LDH, absence of extrarenal manifestations). Secondly, after delivery, the pathological process did not regress (which would be expected with preeclampsia), but, on the contrary, continued to worsen.
The manifestation of chronic glomerulonephritis, nephrotic type, was diagnosed. Secondary chronic glomerulonephritis was excluded. Markers of systemic diseases were studied; antiphospholipid syndrome was not identified. To exclude primary membranous nephropathy, a blood test was taken for antibodies to phospholipase A2 receptors - the result was negative.
Thus, the most likely morphological variant of chronic glomerulonephritis in the patient was minimal change disease or focal segmental glomerulosclerosis. However, performing a kidney biopsy, necessary to clarify the morphological picture of nephritis, was not possible (taking into account coagulopathy in conditions of recent delivery, pronounced nephrotic syndrome, severity of the condition) due to the extreme risk of hemorrhagic complications.
The differential diagnosis of GN during pregnancy is very difficult due to the fact that preeclampsia can occur with a similar clinical and laboratory picture.
One of the most important differential diagnostic criteria for CGN is the timing of the onset of clinical symptoms—the threshold is considered to be 20 weeks of gestation. Thus, proteinuria, detected up to 20 weeks. pregnancy, indicates the presence of background or de novo kidney disease;
Also, the difficulties in diagnosing CGN during pregnancy are determined by the impossibility in most cases of carrying out morphological verification of the diagnosis. Kidney biopsy is rarely performed and, due to the high risks of complications, is limited to very strict indications.
Our patient was hospitalized in extremely serious condition with massive edema leading to anasarca, virtually no diuresis and progression of renal failure, which could require transfer to hemodialysis. In ICU No. 2, intensive therapy was carried out aimed at maintaining vital functions. Pathogenetic therapy was initiated, which included ultra-high doses of corticosteroids (pulse therapy with metipred followed by oral prednisolone, cyclosporine). This therapy is aggressive and carries risks of complications, but is absolutely necessary to save the patient’s life and restore normal function of the kidneys and other organs and systems. Taking into account the severity of the disease and the seriousness of the prognosis, every day, during 40 days of inpatient treatment, there was a struggle for the life of the young mother.
Thanks to timely, active treatment tactics, almost complete remission of severe nephrotic syndrome and restoration of kidney function were achieved. During treatment, renal function indicators completely normalized (creatinine 78 µmol/l), proteinuria decreased from 44 g/day to 1.1 g/day. The level of total protein gradually recovered - 50 g/l and albumin - 28 g/l. The young mother was able to return home to her baby. In the future, doctors from the consultative and diagnostic nephrology department of City Clinical Hospital No. 52 will monitor her health.
Diagnosis at discharge: Main: Chronic glomerulonephritis. Background: I premature surgical birth at 29-30 weeks, myomectomy dated June 29, 2019. Severe preeclampsia. Complications: Nephrotic syndrome. Status on pathogenetic therapy (corticosteroids, cyclosporine). Acute kidney injury is in the process of resolution. CKD stage 2 (GFR 86 ml/min by CKD-EPI). Anemia. Bilateral lower lobe pneumonia is in the process of resolution. Steroid acne. Chronic gestational pyelonephritis. Associated: Congenital heart defect: patent foramen ovale. Pulmonary hypertension. Superficial gastritis. Duodeno-gastric reflux. OU Retinal angiopathy.
Management of pregnancy in patients with kidney diseases requires careful monitoring of clinical and laboratory parameters and, if necessary, active and timely etiotropic or pathogenetic therapy. Kidney diseases are an aggravating background that predisposes to the development of severe pathologies directly associated with pregnancy, such as preeclampsia, eclampsia, and HELLP syndrome. The polymorphism of nephrological diseases dictates the need for careful monitoring of the course of pregnancy, differential diagnosis of various types of kidney damage and timely correction of therapy.
Participated in the management of the patient
Artyukhina Lyudmila Yurievna, head of the nephrology department No. 1 Ekaterina Sergeevna Ivanova, nephrologist of the nephrology department No. 1 Karina Eduardovna Loss, nephrologist of the ICU No. 2 Olga Lvovna Podkorytova, head of the ICU No. 2 Nadiya Fyaatovna Frolova, deputy chief physician for nephrological care Vasily Mikhailo Grabovsky hiv , Deputy Chief Physician for Obstetrics and Gynecology Care.
Risk factors
As you know, inflammation is the result of the activity of bacterial microorganisms. As a rule, these are opportunistic bacteria, in particular, staphylococci, streptococci, E. coli, etc. They are always present in the body, but their reproduction processes are activated against the background of stress, which is the birth process, as well as when the immune system is weakened. Risk factors include:
- loss of blood, which, alas, is inevitable during childbirth;
- vitamin deficiencies;
- anemia (decreased number of red blood cells);
- disturbances in blood clotting processes (fraught with additional blood loss);
- the presence of remnants of membranes and/or placental tissue in the uterus;
- cracks in the nipple area;
- surgical interventions during childbirth;
- severe pregnancy;
- birth process with complications;
- Constant stress, overwork and lack of sleep also affect hormonal levels and the immune system, weakening the body.
What symptoms should you pay attention to?
Many mothers face the problem of elevated leukocytes in the blood after childbirth. Reviews from doctors indicate that in most cases, such changes in the blood count are associated with stagnation of milk or infection of the ruptures.
In itself, an increase in the number of white cells in the blood only indicates inflammation. But the accompanying symptoms can clarify the picture:
- The inflammatory process is inevitably accompanied by an increase in body temperature, sometimes up to 40 degrees or more.
- Bloody and sometimes purulent discharge from the vagina may appear. Sometimes they turn into full-blown bleeding.
- The presence of pain and burning during urination, as well as nagging pain in the lower back. All this is typical for various diseases of the excretory system (in particular, the bladder and kidneys).
- Headaches, severe weakness, chills, body aches, nausea, and vomiting may occur.
If you notice such symptoms, you need to contact your gynecologist as soon as possible.
Possible complications and diseases of the postpartum period
Immediately after giving birth, for one to two months, your body’s organs will begin to recover from pregnancy, during which time you may notice some complications. Firstly, significant discomfort can be caused by uterine contractions, which are necessary for its restoration. You may feel pain in the lower abdomen, which will become more intense as you breastfeed. As a rule, these sensations disappear a few days after birth.
If during the process of delivery the uterus was greatly distended, and your body lacks the hormone oxytocin, which is responsible for its contraction, then the cavity of this organ will not be fully cleansed. This is fraught with the development of such a common postpartum complication as endometritis, characterized by inflammation of the uterine mucosa. This condition is usually accompanied by severe pain, increased body temperature, and copious discharge from the genital tract with an unpleasant odor.
Another common problem is genital injuries, which can occur directly during childbirth. After childbirth, the doctor places stitches, which either dissolve on their own, or the doctor will remove them before discharge from the hospital on the 6th day. A scar in the vestibule of the vagina or in the vagina may cause discomfort during sexual intercourse, but as the tissue heals, these sensations will pass.
After discharge from the maternity hospital, be sure to visit your obstetrician-gynecologist, who will examine the cervix, rule out pathology in the uterus and evaluate its condition.
In addition to the conditions described above, the body of a woman who has just given birth may be exposed to other risks. Diseases that often occur during the postpartum period include:
- varicose veins, the formation of spider veins - as a rule, the disease goes away on its own, but if this does not happen, medical attention may be required;
- hemorrhoids are a common disease that often appears during pregnancy due to the pressure of the enlarged uterus on the abdominal cavity. Pushing during childbirth can also lead to hemorrhoids;
- diseases of the cardiovascular system most often occur in women who give birth after thirty-five years of age, although certain risks exist for very young mothers. Complications from the cardiovascular system arise due to the fact that after childbirth the volume of blood circulation sharply decreases, which sometimes adversely affects the heart and blood vessels;
- Bladder problems are another complication you may encounter after childbirth. It occurs due to a decrease in the tone of this organ, which leads to the fact that the woman simply does not feel the urge to urinate.
What to do if the level of leukocytes increases?
Under no circumstances should such a problem be ignored. If you notice the symptoms described above, you should definitely consult a doctor. The success of therapy largely depends on how quickly the disease is diagnosed.
The treatment regimen depends on the type and location of the inflammatory process and the nature of the pathogen. Treatment almost always involves taking antibiotics. During laboratory tests, it is possible to determine the sensitivity of the pathogen to a particular drug. In addition, patients are prescribed anti-inflammatory, antipyretic, antihistamine medications, vitamins, and other drugs.