Causes of arachnoiditis
Arachnoiditis occurs as a result of acute and chronic infections, inflammatory diseases of the paranasal sinuses, chronic intoxication (alcohol, lead, arsenic), injuries (usually in the residual period).
Arachnoiditis can also occur as a result of reactive inflammation with slowly growing tumors, encephalitis. In many cases, the cause of arachnoiditis remains unclear. Morphologically, arachnoiditis is characterized by clouding and thickening of the arachnoid membrane, accompanied in more severe cases by fibrinoid deposits. In the further course of arachnoiditis, adhesions occur between the arachnoid and choroid, leading to disruption of the circulation of cerebrospinal fluid and the formation of arachnoid cysts.
Arachnoiditis can occur due to acute or more often chronic purulent otitis media (as a result of low-virulent microbes or toxins), as well as complications of purulent otitis media - labyrinthitis, petrositis, sinus thrombosis, as a consequence of cured purulent meningitis or brain abscesses and, finally, can be combined with non-purulent otogenic encephalitis. Otogenic arachnoiditis in most cases is localized in the posterior cranial fossa and much less often in the middle. The course of arachnoiditis can be acute, subacute and chronic.
Arachnoiditis is divided into diffuse and limited. The latter are extremely rare. Essentially, we are talking about more severe local changes against the background of a diffuse process in arachnoiditis.
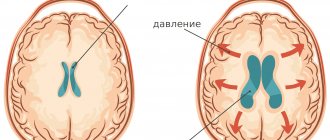
Disruption of the normal circulation of cerebrospinal fluid, leading to the occurrence of hydrocephalus, is based on two mechanisms in arachnoiditis:
- impaired outflow of fluid from the ventricular system (occlusive hydrocephalus)
- impaired absorption of fluid through the dura mater during a diffuse adhesive process (aresorptive hydrocephalus)
RESULTS
- RESPONSIBILITY.
- OPTIONAL CONDITIONS RESULTS Ñ Ð½ÐµÑвов.
- OPTIONAL CONDITION. RESULTS RESULTS .
- ROCK. оñ²² ñ ñµññññ ° ° ð¿¿ ° ° ñðð ððññ police ð½ °ð °ð¿ð¿ð¿¿¿½ police ð¶ð¸ð´len ð ²²¿¿ððð police °³ mill " ¾²ð½ices ð> · ð³ ð °.
- RESULTS. RESULTS, RESEARCH ½Ñе ÑаÑÑÑÑойÑва пÑиÑики), ÑÑойкое из менение лиÑноÑÑи.
- RESULTS. RESULTS Ð¿Ð»ÐµÐ½Ð¸Ñ Ð¶Ð¸Ð´ÐºÐ¾ÑÑи.
- RESPONSIBILITY. RESULTS µÐ½Ð¸Ñ. RESULTS. RESULTS ÑажÑн.
- ROSS. RESEARCH, RESEARCH ÑÑим ÑодеÑжимое.
- RESULTS. RESULTS ие, ÑодеÑжаÑие в Ñебе гной. RESULTS ¸Ð±Ð°ÐºÑеÑиалÑной ÑеÑап¸Ð¸.
Types of arachnoiditis
Arachnoiditis of the meninges (cerebral)
Cerebral arachnoiditis can be localized on the outer convex (convexital) surface of the brain, its base, in the postcranial fossa. The clinical picture of arachnoiditis consists of symptoms of local effects of meningeal lesions on the brain and disorders of liquor circulation.
A common manifestation of cerebral arachnoiditis is headaches of a hypertensive or meningeal nature.
Normal circulation of cerebrospinal fluid (CSF) through the cerebral ventricles may be disrupted by arachnoiditis of the meninges.
Arachnoiditis of the convexital surface of the brain
Arachnoiditis of the convexital surface of the brain is more common in the anterior parts of the cerebral hemispheres, in the area of the central gyri. Due to pressure on the motor and sensory centers, movement disorders (mono- or hemiparesis) and sensitivity may occur. Irritation, and in cases of cyst formation, compression of the cortex and underlying parts of the brain during arachnoiditis cause focal epileptic seizures.
In severe cases, generalized convulsive seizures may occur, leading to the development of status epilepticus. Electroencephalography and MRI of the brain are important for identifying the localization of the focus of arachnoiditis.
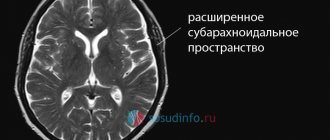
MRI of the brain in T2 mode demonstrates the accumulation of cerebrospinal fluid in the convexital space in cerebral arachnoiditis (indicated by arrows).
Optico-chiasmatic arachnoiditis
Arachnoiditis of the base of the brain is more common. The most common location is the chiasmatic region, which is the reason for the relative frequency of opto-chiasmatic arachnoiditis. The importance of studying this form of arachnoiditis is determined by the involvement of the optic nerves and the area of their decussation in the process, which often leads to irreversible loss of vision. Among the etiological factors for the occurrence of opticochiasmatic arachnoiditis, infectious lesions of the paranasal sinuses, tonsillitis, syphilis, malaria, as well as traumatic brain injury (concussion, brain contusion) are of particular importance.
In the area of the chiasm and intracranial part of the optic nerves, multiple adhesions and cysts form in arachnoiditis. In severe cases, a scar is created around the chiasm. As a rule, opticochiasmatic arachnoiditis is not strictly local: less intense changes are also found at a distance from the main focus. The optic nerves are affected by mechanical factors (compression), as well as the transition to them of the inflammatory process and circulatory disorders (ischemia).
The optic nerves in opticochiasmatic arachnoiditis are affected by mechanical factors (compression of adhesions), as well as the transition to their myelin sheath of the inflammatory process and circulatory disorders.
Opticochiasmatic arachnoiditis usually develops slowly. First, arachnoiditis affects one eye, then gradually (over several weeks or months) the other is also involved. The slow and often unilateral development of opticochiasmatic arachnoiditis helps differentiate the process from retrobulbar neuritis. The degree of vision loss in opticochiasmatic arachnoiditis can be different - from decreased vision to complete blindness. Often, at the onset of the disease with opticochiasmatic arachnoiditis, there is pain posterior to the eyeballs.
The most important aid in the diagnosis of opticochiasmatic arachnoiditis is the study of the visual fields (perimetry) and fundus (ophthalmoscopy). Fields of vision vary depending on the predominant localization of the process. The most typical are temporal hemianopsia (unilateral or bilateral), the presence of a central scotoma (often bilateral), and concentric narrowing of the visual field.
From the fundus of the eye, in 60–65% of cases, atrophy of the optic nerves (primary or secondary, complete or partial) is determined. In 10–13% of patients, swelling of the optic discs is detected. Manifestations from the hypothalamic region are usually absent. An image of the sella turcica also does not reveal pathology. In this form of arachnoiditis, the main symptoms are focal (visual) symptoms; hypertensive phenomena (intracranial hypertension) are usually moderately expressed.
Arachnoiditis of the meninges is a consequence of previous injuries or concomitant infectious diseases of the brain and paranasal sinuses.
Arachnoiditis of the posterior cranial fossa
Arachnoiditis of the posterior cranial fossa is the most common form among cerebral arachnoiditis. The clinical picture of arachnoiditis of the posterior cranial fossa resembles tumors of this location and consists of cerebellar and brainstem symptoms. Damage to the cranial nerves (VIII, V and VII pairs) is observed mainly when arachnoiditis is localized in the cerebellopontine angle. Cerebellar symptoms consist of ataxia, asynergy of adiadochokinesis. With this localization of arachnoiditis, disorders of the circulation of cerebrospinal fluid are expressed.
The symptoms of arachnoiditis in the posterior cranial fossa depend on the nature of the process (adhesions, cysts), localization, and also on the combination of arachnoiditis with hydrocephalus. An increase in intracranial pressure in arachnoiditis can be caused by the closure of the openings of the cerebral ventricles (Lushka, Magendie) due to adhesions, cysts or as a consequence of irritation of the soft meninges with hypersecretion of cerebrospinal fluid (primarily as a result of increased activity of the plexus chorioideus) and difficulty in its absorption. In the absence of a sharp increase in intracranial pressure, arachnoiditis can last for years, with long-term remissions. Arachnoiditis often occurs in the form of arachnoencephalitis due to concomitant inflammatory changes in brain tissue and pressure of adhesions and cysts on the brain.
The acute form of arachnoiditis is characterized mainly by symptoms of increased intracranial pressure (severe headache, mainly in the back of the head, nausea, vomiting, dizziness, often congestive optic discs, sometimes bradycardia), pyramidal and focal symptoms are often absent or mild and inconsistent.
In the subacute course in the neurological status, symptoms of damage to the posterior cranial fossa (most often the pontocerebellar space - the lateral cistern of the bridge) come to the fore. Symptoms of increased intracranial pressure, although they do occur, are less pronounced, and sometimes almost undetectable. Paresis of cranial nerves (V, VI, VII, VIII, less often IX and X and even less often III and IV), most often VIII pairs, is observed, and disturbances of vestibular function in combination with cerebellar symptoms predominate.
Along with instability in the Romberg position - deviation or fall towards the affected ear, unsteady gait, disturbances in index and finger-nose tests, adiadochokinesis, unstable spontaneous nystagmus (directed towards the affected ear or bilateral) - frequent disharmony of vestibular tests is noted (for example, loss of caloric reaction with preserved rotational reaction). Sometimes there is a change in the direction of nystagmus, positional nystagmus. Not all components of this vestibulo-cerebral syndrome are constant and clearly expressed. Homolateral pyramidal signs are rare and hemiparesis of the limbs is even more rare. In the cerebrospinal fluid, changes usually result in increased pressure, sometimes mild. Mild pleocytosis or increased protein content is rarely observed.
Arachnoiditis with other localizations in the posterior cranial fossa is very rare. This is an isolated lesion of the vestibulocochlear nerve in the internal auditory canal, without symptoms of hypertension, prepontine arachnoiditis and arachnoiditis of the cerebellar hemispheres with static disturbances and scanty cerebellar symptoms, with damage to the trigeminal nerve (prepontine form), precerebellar arachnoiditis (anterior surface of one of the cerebellar lobes) with partial cerebellar symptoms, labyrinthine phenomena, inexcitability during caloric and reduced excitability during the rotation test, laterobulbar arachnoiditis with hypertension, cerebellar syndrome and damage to the IX, X, XI cranial nerves (homolateral), arachnoiditis of the posterior lacerated foramen with damage to the IX, X and XI cranial nerves.
With otogenic hydrocephalus of the posterior cranial fossa, symptoms of increased intracranial pressure predominate; with normal cerebrospinal fluid or its “liquefaction” (poor protein) with occlusion of the foramina of Luschka and Magendie, hypertension is combined with mental disorders, vestibular disorders, and sometimes epileptiform seizures.
With general hydrocephalus with the accumulation of a large amount of cerebrospinal fluid, intracranial pressure quickly increases, congestive papillae of the optic nerves appear, and visual acuity decreases. Such crises gradually stabilize (despite ventricular and lumbar punctures) and, if the medulla oblongata is involved, the patient dies.
For differential diagnosis with brain abscess (cerebellum), brain tumor, the clinical course and data from cerebrospinal fluid examination are important. All types of pneumography with a pronounced increase in intracranial pressure are contraindicated.
With arachnoiditis of the posterior cranial fossa, a picture of occlusive hydrocephalus quickly develops, clinically manifested by headache, vomiting, and dizziness. In the fundus there are congestive papillae of the optic nerve. In the cerebrospinal fluid there is a picture of mild protein-cell dissociation. An x-ray of the skull with arachnoiditis of the posterior cranial fossa shows hypertensive phenomena.
A severe complication of arachnoiditis of the posterior cranial fossa is the occurrence of an attack of acute occlusion with wedging of the cerebellar tonsils into the foramen magnum, compressing the brain stem. Arachnoiditis of the posterior cranial fossa can be a cause and difficult to treat trigeminal neuralgia.
Arachnoiditis of the spinal cord membranes (spinal)
Spinal arachnoiditis, in addition to the above reasons, can occur with furunculosis, purulent abscesses of various locations. The clinical picture of cystic limited spinal arachnoiditis is very similar to the symptoms of an extramedullary tumor. There is a radicular syndrome at the level of the pathological process and conduction disorders (motor and sensory). Arachnoiditis is most often localized along the posterior surface of the spinal cord, at the level of the thoracic and lumbar segments, as well as in the cauda equina region. The process usually extends to several roots and is characterized by the variability of the lower limit of sensitivity disorders.
In the cerebrospinal fluid there is protein-cell dissociation. Pleocytosis is rare. Myelographic data are characteristic - the contrast agent is retained in the form of drops in the area of arachnoid cysts. Less common is diffuse spinal arachnoiditis, which involves a large number of roots in the process, but is less clearly manifested by conduction disorders. Spinal arachnoiditis is chronic.
Epidemiology[edit | edit wiki text]
The evolution of the clinical concept of the disease (identification of true clinically relevant arachnoiditis) forced us to reconsider previous ideas about its prevalence. Apparently, arachnoiditis accounts for about 3-5% of organic diseases of the nervous system (Lobzin V.S., 1983). It is twice as common in men. Young people (under 40 years old) clearly predominate. Overdiagnosis is the main reason for the unreasonably large number of patients with cerebral arachnoiditis examined by the medical and social examination bureau.[1]
Diagnosis of arachnoiditis
In the diagnosis of arachnoiditis, in addition to clinical and anamnestic data, additional research methods are used, especially contrast radiography and magnetic resonance imaging of the brain or spinal cord. With arachnoiditis of the convex surface, pneumoencephalography makes it possible to identify both areas of the subarachnoid space that are impassable for air and fluid, as well as expanded areas.
Magnetic resonance imaging (MRI) is performed if arachnoiditis of the arachnoid membrane of the brain is suspected.
Along with this, on the side affected by arachnoiditis, sometimes there is a tightening of the lateral ventricles to the cortex and, thus, asymmetry and deformation of the ventricular system.
- For arachnoiditis of the base of the brain, conventional craniography is of great importance, allowing in many cases to establish hypertensive manifestations (finger impressions, increased vascular pattern, change in the shape of the sella turcica, etc.).
- It is important to study the cerebrospinal fluid, which makes it possible to clarify the degree of hydrocephalus, as well as the presence of a liquorodynamic block in the subarachnoid space. Inflammatory changes (pleocytosis), as a rule, are not pronounced.
- Electroencephalography is important when the lesion is localized on the convex surface of the brain (with a focal cystic process, the electroencephalogram (EEG) pattern is close to that of tumors, but diffuse changes are more often recorded).
- It is difficult to overestimate the importance of examining the fundus and visual field in opticochiasmatic arachnoiditis and arachnoiditis of the postcranial fossa.
- Myelography is important for diagnosing spinal arachnoiditis. The greatest difficulty is distinguishing limited arachnoiditis from a tumor.
- For arachnoiditis, MRI of the brain or MRI of the spinal cord is performed in myelography mode to clarify the localization of the process and the degree of involvement of the brain tissue and cranial and spinal nerves.
When diagnosing arachnoiditis, it is necessary to take into account a history of acute and chronic infection, trauma, less common and less intense changes in the fundus and x-ray of the skull, and the course of the process (continuous and with remissions). With tumors in the chiasm area, pituitary-intermediate and other neurological symptoms are more pronounced than with arachnoiditis. With tumors of the posterior cranial fossa and spinal cord, there are more severe conduction disorders.
Enlarged lateral ventricles on MRI of the brain in hydrocephalus with arachnoiditis of the meninges.
Features[edit | edit wiki text]
Section source:
Fundamentals of Chinese medicine
[1]
From a clinical position, it is important to distinguish between two pathogenetic variants of cerebral arachnoiditis (Akimov G. A., Komandenko N., I., 1978; Lobzin V. S., 1983):
- True (actual) arachnoiditis: an active adhesive process of an autoimmune nature, occurring with the formation of antibodies to the membranes of the brain, productive changes in the form of arachnoid endothelial hyperplasia, leading to the death of cells and obliteration of the cerebrospinal fluid channels in the subarachnoid space. Characteristic is the diffuse nature of the damage to the membranes, involving the molecular layer of the cortex, sometimes the ventricular ependyma, and the choroid plexus. The course is chronically progressive and intermittent.
- A residual condition after neuroinfection or traumatic brain injury resulting in obliteration, fibrosis of the membranes (usually of limited extent), with the formation of adhesions and cysts at the site of necrosis. There is complete or partial regression of symptoms of the acute period (with the exception of epileptic seizures). Progression, as a rule, is absent.
Classification[edit | edit wiki text]
Section source:
Basics of Chinese medicine
[1]
Depending on the predominant localization, arachnoiditis is distinguished:
- convexital;
- basilar (in particular, opto-chiasmal, interpeduncular);
- posterior cranial fossa (in particular, the cerebellopontine angle, cisterna magna).
However, such rubrication is not always possible due to the diffuse nature of the adhesive process.
Taking into account the pathomorphological features, it is advisable to distinguish between adhesive and adhesive-cystic arachnoiditis.
Etiology and pathogenesis[edit | edit wiki text]
Section source:
Basics of Chinese medicine
[1]
The disease is multi-etiological. Main causes: influenza and other viral infections, chronic tonsillitis, rhinosinusitis, otitis media, traumatic brain injury. In general, infection is the cause of the disease in 55-60% of patients, closed craniocerebral injury - in 30%, in 10-15% it is difficult to definitely judge the etiological factor (Pil B.N., 1977; Lobzin V.S., 1983 ).
The most common cause of infectious arachnoiditis is influenza. Arachnoiditis develops within a period of 3-5 months to a year or more after influenza, which is explained by the time required for the autoimmune process to occur.
Rhinosinusogenic etiology is reliably established in 13% of all cerebral arachnoiditis (Gushchin A.N., 1995). The disease develops slowly, usually against the background of exacerbation of rhinosinusitis. After a closed craniocerebral injury, the light period is also long (usually from 6 months to 1.5-2 years). The severity of the injury does not play a decisive role, although more often the adhesive membrane process is formed after a brain contusion or traumatic subarachnoid hemorrhage. The main pathogenetic factor is the formation of antibodies to antigens of damaged membranes and brain tissue.
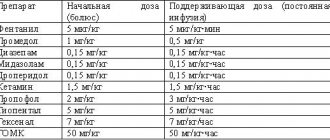
Principles of treatment[edit | edit wiki text]
Section source:
Basics of Chinese Medicine
[1]
- It should be carried out in a hospital after diagnosis using additional methods and a conclusion about true (actual) arachnoiditis.
- Determined by etiology (presence of a focus of infection), predominant localization and activity of the adhesive process.
- Repetition of courses and duration of drug therapy: glucocorticoids (prednisolone) at a dose of 60 mg per day for 2 weeks;
- absorbable (bioquinol, pyrogenal, rumalon, lidase, etc.);
- dehydration (with increased intracranial pressure);
- antihistamine, antiallergic;
- stimulating metabolic processes in the brain (nootropics, cerebrolysin, etc.);
- correcting concomitant mental disorders (tranquilizers, sedatives, antidepressants);
- antiepileptic drugs (taking into account the nature of epileptic seizures).