Consultation with a cardiologist – RUB 1,750.
- What is hypertension?
- Causes of arterial hypertension
- Symptoms of the disease
- Diagnostics
- Treatment and prevention of hypertension
Hypertension (arterial hypertension)
is one of the most common medical problems.
An increase in pressure in the blood vessels of the body is called hypertension (from the Greek word hyper - “over” and the Latin word tendere - “to pull”) or hypertension (from the Greek words hyper and tonus - “increased tension”). Thus, the words “hypertension” and “hypertension” are synonymous.
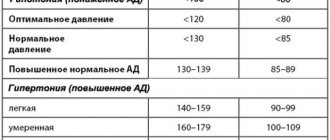
Arterial hypertension (hypertension) is understood as a persistent increase in blood pressure of more than 140/90 mmHg, recorded at different times with several measurements. Moreover, both blood pressure numbers do not have to be elevated at the same time. To make a diagnosis of arterial hypertension, a persistent increase in one of the blood pressure components is sufficient: either systolic or diastolic.
In 90-95% of cases, arterial hypertension is an independent disease - hypertension. In 5-10% of cases, arterial hypertension is a consequence of various diseases and conditions - this is the so-called secondary or symptomatic arterial hypertension. Only when all possible causes of secondary arterial hypertension are excluded are we talking about hypertension.
Where does the disease come from?
The cause of hypertension is still unknown. A number of people have a hereditary predisposition to hypertension.
In addition to unfavorable heredity, there are other factors for the development of arterial hypertension. These include excessive consumption of table salt, obesity, and stress.
The above factors contribute to a greater extent to the development of hypertension in persons with unfavorable heredity.
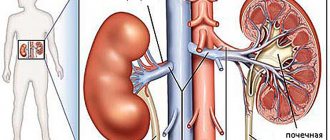
The main causes of secondary arterial hypertension are bilateral (less often unilateral) tissue damage. Diseases of a number of endocrine glands, such as the pituitary gland, adrenal glands and thyroid gland, can also lead to the development of secondary arterial hypertension.
Arterial hypertension is dangerous precisely because of its complications, which can often be fatal. If it did not cause such complications, then arterial hypertension itself would not arouse such interest. Indeed, of all the unpleasant sensations that are characteristic of high blood pressure, only a headache can be noted.
The presence of arterial hypertension causes the development of a number of changes in the body of its owner. As a rule, these changes develop gradually. In a stable course of arterial hypertension, the severity and reversibility of these changes are directly dependent on the duration of the disease, as well as on the level of persistent increase in blood pressure. First of all, long-term arterial hypertension (without appropriate treatment) leads to changes in the structure and properties of the arterial wall throughout the body.
As a result of a series of transformations, the vascular wall loses its inherent elasticity, becoming dense and brittle, facilitating hemorrhages. The arteries of the kidneys, brain, fundus and limbs suffer the most from a persistent increase in blood pressure. Arterial hypertension accelerates the processes of premature aging of the arterial wall (atherosclerosis) throughout the body, being a risk factor for the development and progression of coronary heart disease (CHD).
Thus, arterial hypertension is accompanied by various complications and concomitant diseases. Among them:
- Atherosclerosis
. Arterial hypertension can be a risk factor for atherosclerosis, a disease in which there is a high level of low- and very low-density lipoproteins (cholesterol) in the blood, as well as the formation of atheromatous plaques on the walls of blood vessels. And this, in turn, contributes to the further development of arterial hypertension. - Heart diseases
. Arterial hypertension increases the risk of myocardial infarction, as it is a risk factor for atherosclerosis, and also contributes to the narrowing of the coronary arteries that supply blood to the heart muscle. - Diseases of the central nervous system
. These include conditions such as stroke, chronic cerebrovascular accident, etc. - Kidney diseases
. Arterial hypertension is one of the main causes of kidney diseases, including renal failure, which is associated with impaired blood circulation in them. - Visual impairment.
Arterial hypertension is accompanied by impaired blood circulation in the retina, as well as the optic nerve (the nerve also receives nutrition from very small arterioles). - Diabetes.
Arterial hypertension is a risk factor for many complications of diabetes, for example, diabetic foot, retinopathy (retinal pathology), etc. - Preeclampsia
is a condition characteristic of pregnant women with symptoms of gestosis (toxicosis). Hypertension may be a sign of this serious complication. - Metabolic syndrome.
This is a group of conditions associated with obesity, increased blood pressure, increased blood sugar, and the risk of myocardial infarction and stroke. - Erectile disfunction.
The insidiousness of arterial hypertension (hypertension)
It also lies in the fact that it is often asymptomatic; even with high blood pressure (BP), the patient’s health can remain good. This is the reason for the negative attitude towards medical recommendations.
But feeling well with high levels of arterial hypertension (hypertension) does not protect the patient from the dangerous complications of this disease. Every patient suffering from arterial hypertension (hypertension) must understand that a long-term and sustainable decrease in blood pressure improves the quality of life and reduces the risk of developing vascular complications: by 45% - the number of strokes and by 38% - the number of myocardial infarctions.
What studies and tests should you undergo if you have high blood pressure?
Arterial hypertension is a condition that is often accompanied by changes in metabolism and disorders of internal organs. Therefore, simply monitoring blood pressure levels using a tonometer is not enough.
It is advisable for all hypertensive patients and people with a tendency to high blood pressure to undergo periodic examinations consisting of the following studies and tests:
- To begin with, you must undergo general clinical tests : a general blood test and a general urine test. They will help assess your health, identify inflammatory processes in the body, anemia, and metabolic disorders.
- Biochemical blood test with a targeted study of cholesterol . This test is recommended once a year for all people over 30 years of age. It is atherosclerosis, caused by increased cholesterol levels in the blood, that is the main cause of arterial hypertension in older age. Metabolism is disrupted, a large amount of “bad” cholesterol enters the bloodstream, and cholesterol plaques begin to grow in the lumen of blood vessels.
- Blood glucose test . This analysis is most relevant for people over 40 years of age. With excess body weight, poor nutrition, and a predominance of fatty and sweet foods, there is a very high load on the pancreas. The result may be type 2 diabetes. This disease is accompanied by an increase in blood glucose levels, does not manifest itself for a long time and contributes to the development of symptomatic hypertension.
- Study of blood electrolytes . High blood pressure is often accompanied by increased sodium in the blood.
- Blood clotting study . Often, increased blood pressure is accompanied by impaired blood flow and the formation of blood clots.
- Electrocardiography is a study that helps assess the functional state of the heart, identify disturbances in its functioning, and enlargement of the atria and ventricles.
- Ultrasound of the kidneys . The kidneys are an organ that greatly influences blood pressure levels. After all, they are the ones who filter the blood and turn it into urine.
Among medical specialists, it is advisable to periodically visit a therapist, cardiologist, endocrinologist, neurologist.
Those taking potassium-sparing drugs (veroshpiron, ACE inhibitors, sartans) are recommended to periodically check the level of potassium in the blood.
Cardiologist Nartova N. A
Diagnostics
The first step in diagnosing hypertension is to take several blood pressure measurements and analyze the medical history.
The second stage - laboratory and instrumental - includes:
- general urine analysis;
- general blood analysis;
- ECG;
- Ultrasound of the heart;
- Ultrasound of other organs (kidneys, adrenal glands, blood vessels);
- examination of the condition of the fundus by an ophthalmologist.
Assessment of overall cardiovascular risk
During the examination of patients with arterial hypertension, it is necessary to assess existing risk factors, identify concomitant clinical conditions and determine the degree of target organ damage. This stage of working with the patient is the most important, as it determines the treatment strategy. The amount of treatment that should be prescribed to a patient must correspond to the risk group to which the patient belongs. To determine the risk group for developing cardiovascular complications, risk stratification criteria are used.
In accordance with these criteria, all patients with arterial hypertension can be classified into one of four risk groups for developing cardiovascular accidents. Such differentiation into risk groups is necessary to select the optimal tactics for managing patients with arterial hypertension and measures to prevent further complications. These factors and your risk level can be determined after consulting a cardiologist.
Cushing's syndrome and disease.
An adrenal tumor or enlarged adrenal glands can secrete another type of hormone - cortisol. If too much of this hormone is produced, a condition called hypercortisolism develops. There are two possible variants of hypercortisolism:
* If the adrenal glands work autonomously, releasing cortisol into the blood regardless of the body's needs and regulation by the pituitary gland, then this disease is called Cushing's syndrome.
* If the adrenal glands are hyperfunctioning due to the fact that they are stimulated by a pituitary tumor, then Cushing's disease is diagnosed.
Outwardly, both of these diseases manifest themselves in the same way; they can only be distinguished through a series of laboratory tests.
Hypercortisolism is characterized by:
- increased blood pressure,
- slimming limbs,
- fat deposits in the abdomen, upper back, shoulders,
- muscle weakness,
- the face becomes round and red,
- the appearance of red-violet stretch marks (striae) on the skin of the abdomen, thighs, shoulders,
- formation of bruises, minor hemorrhages on the skin from minimal impacts,
- bone fractures due to minor trauma due to the development of osteoporosis,
- infrequent or absent menstruation,
- infertility,
- tests may reveal an increase in cholesterol, an increase in blood sugar, up to the development of diabetes mellitus.
Treatment and prevention of hypertension
Prevention of hypertension consists of lifestyle adjustments, preventive examinations to identify possible failures that are prerequisites for hypertension, and their surgical treatment.
Drug treatment includes taking several groups of medications. Can be assigned:
- ACE inhibitors;
- calcium antagonists;
- angiotensin 2 receptor antagonists;
- diuretics;
- beta-adrenergic antagonists;
- alpha-blockers;
- means of central action;
- combination drugs (combination of several substances in one drug).
At SM-Clinic you can undergo a preventive examination to timely identify possible problems with blood pressure and receive qualified treatment for any type of hypertension.
Causes of low blood pressure
The following circumstances may cause the symptom:
- heart diseases - bradycardia, heart valve pathologies, heart failure;
- pregnancy - hypotension occurs due to the fact that the volume of blood circulation in the body increases;
- endocrine disorders - hypothyroidism, hypoglycemia, diabetes mellitus;
- dehydration caused by intense physical activity, diarrhea, excessive use of diuretics;
- large blood loss due to injury or internal bleeding;
- anaphylactic shock and other severe allergic reactions.
Another reason could be starvation.
Symptoms of low blood pressure
In its acute form, the manifestation of arterial hypotension is accompanied by insufficient oxygen supply to the brain. The symptom is often accompanied by dizziness. Brief visual disturbances may occur. The gait becomes unsteady, the skin turns pale. Fainting is possible.
The chronic form of arterial hypotension manifests itself in the form of weakness, apathy, and drowsiness. The patient is often tired and may experience headaches. During attacks of hypotension, mood swings occur, memory is impaired, and body temperature changes. The symptom is accompanied by sweating of the palms and feet. Tachycardia occurs. In women, hypotension can cause menstrual irregularities, and in men - sexual dysfunction.
The pressure drops sharply due to a sudden change in body position (from horizontal to vertical). The symptom may cause lightheadedness. Arterial hypotension is often accompanied by vegetative crises of a vagoinsular nature with the following manifestations:
- release of insulin into the blood;
- a sharp drop in glucose levels;
- accumulation of excess heat in the body;
- profuse sweating;
- prostration;
- increased activity of the digestive system;
- bradycardia;
- fainting;
- difficulty breathing;
- vomit.
Physiological hypotension in most cases does not cause serious discomfort to a person, but may include some of the symptoms listed above.
What tests are taken during laser vision correction?
Laser vision correction is used when it is necessary to restore the focusing of the eye lens. Treatment of myopia, farsightedness, and astigmatism is carried out. The LASIK system has become the most popular due to the absence of open wounds, the speed of the procedure, and easy rehabilitation.
How is LASIK performed?
A fragment of the outer layer is removed using a laser. Afterwards, the shape of the eye lens is automatically adjusted according to personal parameters. The damaged shell returns to its original place. The laser is not accompanied by complications such as scars.
What preliminary preparation is necessary before the operation?
- Before your first visit, you need to stop wearing soft lenses for 7 days and hard ones for 1 month. Interval use of glasses is allowed as needed.
- A week before the operation you need to refrain from: baths, swimming pools, saunas, water parks. High temperatures are dangerous due to changes in pressure; visiting public places can lead to infection.
- Before the vision test, you need to remove eyelash extensions and do not use perfumes or cosmetics. Strong odors can make you feel tearful.
Vision correction eliminates the consequences, but not the cause. For some diseases, such as progressive myopia, it is necessary to undergo preliminary treatment. The ophthalmologist will give detailed advice and prescribe individual tests.
The presence of specific diseases, such as false myopia, is dangerous due to false data. Training requirements will be more stringent. The doctor will prescribe anti-spasm drops to get more accurate test results. The subsequent result depends on how correctly the diagnosis was carried out before vision correction.
Preliminary diagnostics must be taken seriously: the parameters of the resulting studies are important - the process occurs on very small volumes, every millimeter matters. The diagnosis - knowledge of the cause of visual impairment - influences the choice of treatment method.
What tests are taken during laser vision correction?
Preparation takes 2 hours including the first consultation. In eye disease treatment centers, the devices are located in one office. There are no diagnostic restrictions before vision correction; you can go to any clinic. It is better to be examined where LASIK will be performed to ensure the accuracy of the data that the surgeon will receive.
- The traditional test of visual acuity is carried out using a device - an autorefkeratotonometer. Sivtsev tables are used as a testing method
- Refraction testing is a test of the ability to see at night. The term “twilight vision” is more commonly used.
- An individual map is drawn up. The parameters of curvature, shape, and thickness are entered.
- The eye examination occurs through: an ophthalmoscope, a fundus lens. The condition of the retina, optic nerve, and blood vessels is checked. The medical term is ophthalmoscopy.
- Tonometry is a mandatory study of the pressure level of the eyeball.
A large number of contraindications require a full examination. The operation cannot be performed: minus is greater than -10, plus is greater than +6 diopters, there are corneal diseases, dry eye syndrome, glaucoma, cataracts, retinal detachment have been detected. In severe cases, correction alone is not enough; more serious surgery is needed.
What is needed for laser vision correction?
Before the day of surgery, you need to submit a list of blood tests: general analysis, hepatitis B and C - the test is accepted up to 1 month, HIV - 3 months, RW (MRP + ELISA) - 2 weeks.
Documents for concluding an agreement
When it has been determined that there are no contraindications to the operation, a service agreement is concluded and a day for laser correction is scheduled.
- Russian Federation passport - data is indicated in the contract.
- General health insurance policy - compulsory medical insurance and SNILS for opening a sick leave.
If the work does not have dangerous, harmful production factors, sick leave is issued for a period of 7-10 days. Payment in many clinics is possible using an installment plan. Down payment 20% - 40%.
Restrictions for coronavirus infection covid-19
It is now not recommended to come with relatives and friends on the day of vision correction to maintain sterility in the context of the spread of COVID-19. The appointment is by appointment, the laser takes 10-15 minutes, including preliminary preparation - special drops are used and a suit is issued to ensure sanitary cleanliness, worn over clothing.
Examination on the day of laser vision correction
All diagnostics are carried out before the day of intervention, but after that control is carried out: the acuity is checked using a device, and ophthalmoscopy is performed. Based on this, the patient is given a report on the postoperative condition. Afterwards, the client is released for outpatient rest - staying at home. The first 24 hours are the most important and difficult. If you have the opportunity to meet a relative or friend afterward, this will greatly alleviate the condition. The consequences will be swelling, severe tearfulness, photophobia. You need to take sunglasses with you.
Follow-up appointment and diagnostics after LASIK
Before closing the sick leave, all initial studies are carried out to determine the success of the operation. A map with all indicators is drawn up - this is necessary for further monitoring of the condition. Pathologies are rare; further observation is recommended to exclude risks.
Return to normal life after laser vision correction
To maintain the clinic’s guarantee, two mandatory examinations are prescribed - after 6 and 12 months. The period is determined by the reaction to changing seasons and individual characteristics. For astigmatism or myopia, behavioral factors are important. Regular preventive maintenance is required - undergo control diagnostics.
The period considered critical is 3 years; if the results are stable, the diagnosis is removed. Medical institutions prescribe a time period of 7-10 years, after which weakening due to age-related reasons is possible; repeating the correction is considered normal.
Treatment
It is prescribed depending on the reason why blood pressure decreases. If we are talking about secondary symptomatic hypotension, it is necessary to first eliminate the underlying disease. If the patient has arterial hypotension of neurovegetative origin, it is necessary to correct the autonomic balance.
To relieve the symptoms of hypotension itself, the following measures are necessary:
- normalization of sleep and daily routine;
- various massage options (cervical-collar area, aromatherapy, etc.);
- hydrotherapy, physiotherapy.
You may also be prescribed medications - herbal adaptogens, anticholinergics, antioxidants, nootropics and other drugs.