According to Rosstat, in 2010 the mortality rate in Russia from diseases of the cardiovascular system was 805.9 cases per 100 thousand people. This is 2-3 times more compared to road traffic accidents and infectious diseases.
Heart and vascular diseases are the first and main cause of mortality in the Russian population - 56.8% of all deaths. The main reason is insufficient knowledge about the dangers of this group of diseases.
September 29 is World Heart Day, which is supported by the World Health Organization (WHO) and UNESCO. Its goal is to inform society about the danger caused by the epidemic of cardiovascular diseases in the world and encourage the entire population to take preventive measures. On World Heart Day, it is customary to also talk about the culture of health: about regular medical monitoring for early detection of diseases, risk factors, developing skills to deal with stress, and how to maintain health in poor environmental conditions.
We are talking about cardiovascular diseases and how to prevent them with Bespalko Inna Arkadyevna, Doctor of Medical Sciences, doctor of the highest category, chief cardiologist of the multidisciplinary clinic CELT.
Our heart is constantly working - it pumps about 10,000 liters of blood per day in an adult. It is constantly under pressure: work overload, family problems, stress, bad habits. The main organ of the complex vascular web - the cardiovascular system - must serve as long as it needs. But in practice, it turns out that the heart lasts as long as you take care of it.
About risk factors and epidemics of cardiovascular diseases
Diseases of the cardiovascular system kill such a colossal number of people every year that for several decades they have been the leader in the competition for the title of “the most mass killer of the 21st century.” The World Health Organization (WHO) projects that by 2030, approximately 23.6 million people will die from cardiovascular diseases, mainly from stroke and ischemia.
The tragedy of the situation is that diseases of this group are asymptomatic: sometimes a heart attack or stroke becomes the first sign that attention needs to be paid to the condition of the heart and blood vessels. The obvious solution to the problem - early diagnosis, regular monitoring of blood pressure and heart rhythms - faces an inexorable human factor: patients, convinced that instead of a heart they have a fiery engine, brush aside medical recommendations, not wanting to waste time on prevention.
The most important risk factors for cardiovascular mortality, which had already become known by the end of the 50s, were age and family history. This is something that cannot be influenced. But there are others: smoking, arterial hypertension, cholesterol levels, diabetes, obesity. You can influence them. By the forties of the twentieth century, it became clear that people began to most often die not from infections, as was the case before, but from cardiovascular diseases. Therefore, the American Heart Institute was organized, and since 1948 in Framingham, a small town near Boston, all residents of the city were included in the study, which continues today. They measure blood pressure, sugar, fibrinogen and other indicators. These data were later confirmed in large randomized controlled trials: special tables were created that allow one to estimate the risk of death within 10 years depending on factors. By the way, controlling risk factors lengthens life and improves its quality.
Is it possible to avoid on-site inspections?
The tax office does not waste time on companies that behave in a law-abiding manner. If you pay taxes honestly and submit reports without errors, they are unlikely to be interested in you.
Entrepreneurs who have just started running a business also have nothing to worry about. There is nothing to take from the new company yet. And why should the tax office rush: the statute of limitations for tax violations is three years. It is more profitable for inspectors to look for violations over several years at once.
No one is 100% immune from inspections. To calculate the risk of “running into” an on-site inspection, study the order of the Federal Tax Service of Russia dated May 30, 2007 No. MM-3-06 / [email protected] Appendix No. 2 to this order lists the criteria that help entrepreneurs check themselves.
The problem of the century is atherosclerosis
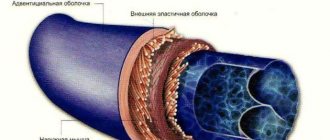
Atherosclerosis is deposits of cholesterol in the wall of a vessel in the form of plaques, which can partially or completely close the lumen of the vessel. This process happens with age for everyone, but in different ways. Its development is influenced by heredity (heart attacks or strokes in close relatives at an early age), the level of cholesterol and its fractions in the blood, lifestyle (smoking, lack of physical activity, poor nutrition) and the presence of concomitant diseases (arterial hypertension, diabetes mellitus, kidney disease ). All these diseases and conditions contribute to faster and more intense growth of atherosclerotic plaques.
The most “popular” atherosclerosis is obliterating - when atherosclerotic plaques are deposited on the walls of blood vessels and therefore block them. It usually affects large arteries of the elastic and muscular-elastic type - for example, the terminal aorta, iliac or femoral arteries. Often these are the lower extremities. People die from this type of atherosclerosis all over the world because it ends in a stroke or heart attack. Less is known about vasodilatory atherosclerosis - when the nutrition of the vascular wall is disrupted, causing it to expand, forming a pouch. At the final stage of type 2 atherosclerosis, it is called an aortic aneurysm. An aneurysm occurs in the thoracic or abdominal aorta. Statistics show that abdominal aneurysm occurs more often. But all aneurysms are equally dangerous. At one unexpected moment, the bag bursts and the person dies. Vasodilating atherosclerosis is talked about less, but people die from it just as often as from obliterating atherosclerosis. The percentage of people dying from vasodilating atherosclerosis is quite high - up to 75%.
The aorta delivers blood from the heart to all organs and tissues, passing through the chest and abdominal cavity. The normal diameter of the abdominal aorta is about 2 cm. When the diameter increases by 1.5-2 times, an aneurysm is formed. To prevent aneurysm rupture, endoprosthetics is performed. Aortic aneurysm is one of the most unpredictable diseases. Very often it appears and gradually increases in size unnoticed by the patient - therefore, sometimes the first clinical symptom of an aneurysm is its rupture. The incidence of aneurysms increases with age.
A ruptured aneurysm is usually fatal, regardless of treatment. The survival rate of patients after a standard aortic replacement procedure, even in a planned manner, is low; every fifth patient dies.
What types of tax audits are there?
There are two main types: office and away.
- A desk audit takes place every time after submitting a declaration - and usually unnoticed. The inspector is studying information about the company in his office. If questions arise, he sends the entrepreneur a request for clarification or documents.
- The on-site inspection takes place at the entrepreneur's home. Tax officers study the company, look at documents, talk with the manager and his employees. Entrepreneurs are usually afraid of precisely such “tax measures.”
An on-site inspection is a thorough investigation that takes a lot of time. It is impossible to verify all companies. Therefore, the tax office selects the most suspicious taxpayers. It follows certain criteria, which we will describe below.
About “good” and “bad” cholesterol
We get only a third of the necessary cholesterol from the outside, and synthesize two thirds ourselves. From cholesterol, the body produces bile salts (without them it is impossible to digest fats), steroid hormones (responsible for reproductive function), and cortisol (regulates carbohydrate metabolism). Cholesterol is necessary for kidney cells, spleen and bone marrow functions; it is responsible for the strength of cell membranes. In the skin, vitamin D is formed from cholesterol under the influence of light. In general, we need cholesterol in much the same way as fats, proteins, carbohydrates and water.
Not so long ago, a cholesterol level of 6.5 mmol/liter was considered the norm in Russia, and 3.5 mmol/liter in Japan. Now in Europe, the USA and Russia, the normal level of total cholesterol is considered to be below 5.2 mmol/l. But the main indicator is low-density lipoprotein cholesterol, popularly called “bad” cholesterol. In people with a low risk of developing coronary heart disease, it should be less than 3.0 mmol/l, in patients with a high risk - less than 2.6 mmol/l, and in those who have atherosclerosis and its complications - coronary heart disease, brain disease and other vascular zones, its target level is less than 1.8.
How to assess the levels of professional risks at an enterprise: a step-by-step algorithm
Stage 1. Risk identification
Sources of information for identifying hazards are:
- regulatory legal and technical acts, reference and scientific and technical literature, local regulations, etc.;
- results of production control over compliance with sanitary rules and implementation of sanitary and anti-epidemic (preventive) measures;
- results of a special assessment of working conditions in the workplace;
- results of monitoring the technological process, production environment, workplace, work of contractors, external factors of the production environment;
- results of the analysis of questionnaires received from employees.
- results of an audit (survey) of employees;
- practical experience.
In addition to questionnaires, sources of information for identifying risks can be statistical information on injuries and occupational diseases, production control data, analysis of job descriptions and standard operating procedures (work plans, technological maps and technical regulations).
Expert recommendation: All employees of the organization fill out questionnaires in which they note the frequency and likelihood that the hazard occurs rarely, often, or constantly. Based on the analysis of information sources, it is necessary to create a register of identified hazards, subject to regular and timely updating.
Stage 2. Determining the probability and frequency of damage
In the second stage, the Register is processed to find out what damage could be caused if the hazard occurs. To do this, an expert group consisting of members of the risk commission can independently or with the involvement of an external expert determine the severity of the resulting health damage against each hazard.
Note! Be sure to include a labor protection specialist in the composition of such a commission, as well as leading technical specialists - experts, a representative of a trade union or other workers' body.
To correctly assess risks, it is necessary to establish qualitative values for the probabilities of damage occurrence: low, medium and high. In this case, the probability of an outcome not associated with the occurrence of damage is assessed as average.
Low - in job descriptions there is no need to carry out operations or manipulations that are characterized by a specific danger. Therefore, the danger should not arise at all.
For example, the hazard register indicates the danger of an animal bite. At the same time, in the workplace and in the workspace (including the territory), data from the video surveillance console did not record a single case of the appearance of an animal.
Medium - a risk may occur if the employee grossly violates labor protection requirements, standard operating procedures, technological maps and regulations, or performs job duties not included in the job description, for which the employee is not trained, does not have the necessary qualifications and permission.
High - the onset of a risk of danger is typical for the specified position and is determined by the technology of performing the work.
For example, during the special assessment, it was determined that the employee was affected by such a factor as noise, and hazardous working conditions of subclass 3.1 were determined at the workplace. And during the assessment of professional risks, they determined the likelihood that the employee will lose his hearing.
Stage 3. Assessment risk calculation
At the third stage of risk assessment, the obtained data on the likelihood of a threat occurring and the severity of its consequences are calculated in order to establish the level of risk for each hazard, as well as the integrated risk. Then a ranking is made - from high-risk to low-risk hazards.
To determine the degree of risk, it is necessary to carry out a calculation. To do this, perform the following operations sequentially:
- Identify hazards and, if necessary, their manifestations.
- Each identified hazard is assigned a possible damage and a corresponding weighting factor.
- Determine the qualitative values of the probabilities of the occurrence of damage and the outcome not associated with the occurrence of damage, and the corresponding weighting coefficients by logical analysis of the event tree or using a verbal description of the probabilities (frequencies).
- By multiplying the numerical values of the probabilities (frequencies) of damage occurrence by the corresponding weighting coefficients of damage, the risks for each of the identified hazards are determined.
- Using the risk significance assessment scale, the significance of risks for each of the identified hazards is assessed.
By adding up the risks for each identified hazard in the workplace, the total risk is determined.
Stage 4. Development of an action plan to reduce the level of risk and control its implementation
At this stage, the process of direct assessment ends, and the final stage begins - the stage of making a decision to reduce or abandon the risk (exclusion from the technological chain) and replacement with an acceptable level of risk. This is the stage of developing an action plan to reduce risks.
Upon completion of work on assessing occupational risks, the following local regulations are developed, approved and communicated to employees:
- hazard register;
- report on the assessment of risk levels, indicating the established levels for each risk.
- action plan to reduce levels of professional risks
All detected (identified) hazards must be taken into account when conducting workplace briefings and internships.
All personal protective equipment should be issued, and collective protective equipment should be installed based on the identified hazards.
Stage 5. Management of assessed risks
Since risk assessment is not an end in itself, the main stage is precisely the management of assessed risks. Taking measures to reduce levels of occupational risks or eliminate them is the task facing the employer.
After the order on the application of the results of the occupational risk assessment comes into force, the commission carries out work to inform workers about the risk of damage to health. To do this, you need to make changes to the workplace briefing program, the introductory briefing program, and also place the occupational risk assessment materials in the “Occupational Safety and Health” section - “Assessment of occupational risks in the workplace” on the official website.
Note! The effectiveness of developed measures to manage occupational risks must be constantly assessed. To do this, it is necessary to assess the effectiveness of risk reduction measures at a specified frequency, for example, at least once a year (every three years, every five years) with the preparation of a corresponding report agreed upon by the representative body of workers.
If necessary, the heart can instantly change its operating mode
Normally, the heart is a strong muscular pump capable of pumping blood throughout the body to provide oxygen and nutrients to all organs and tissues of the body, and remove waste products. But in order to move blood through spasmodic vessels, the heart requires more effort than normal. This leads to its size becoming larger, especially the left ventricle. Because of this, weakness of the heart muscle develops. When the heart stops adequately supplying tissues and organs with oxygen and nutrients, doctors diagnose heart failure. It can be caused by irregular heartbeats (cardiac arrhythmias). It is dangerous and can lead to heart failure when the heart beats more than 140 beats per minute, since the processes of filling and ejecting blood by the heart are disrupted.
You can live with heart failure for many years without a diagnosis. This is not an independent disease, but the outcome of various heart diseases. It signals itself in the form of increased fatigue, swelling of the legs, shortness of breath, asthma attacks, and causeless weight loss. These symptoms, if noticed individually, appear in a wide variety of diseases. Therefore, the correct diagnosis is rarely made and usually in later stages. Significant weight loss, which is typical of severe heart failure, is often mistaken for a sign of cancer. And harmless swelling of the legs caused by stagnation of lymph is diagnosed as “heart failure.” With some primary symptoms (for example, pulmonary edema), there is an immediate risk of death. Within 3-5 years, 50% of patients die from heart failure, and after 9 years, only 2 people out of 1000 patients remain alive - of course, provided that appropriate treatment is not carried out. There is a radical way to help - a new heart transplant. But restrictions - an age limit, an expensive operation, few donor hearts - make it unrealistic for most.
In recent years, medical science, pharmacology and medical experience have helped to achieve amazing success in treating even severe forms of heart failure. Patients can not only save their lives, but also restore their quality. Moreover, treatment can take place on an outpatient basis, without a hospital stay.
Treatment of people with cardiovascular diseases requires effort, time and great pedantry. The speed and accuracy of diagnosis of the underlying disease that caused heart failure plays a huge role. In 50% of cases, this is coronary heart disease, which can be identified and treated with coronary angiography and angioplasty. The earliest, they are called preclinical (that is, before the onset of complaints), forms of heart failure can be treated only by using instrumental research methods: echocardiography, Holter monitoring, stress tests.
Introduction
Mortality from cardiovascular diseases (CVD) is much higher than that from infectious and oncological diseases. The World Health Organization (WHO) estimates that 17.5 million people worldwide died from CVDs in 2012, accounting for 31% of all global deaths. Of this number, 7.4 million (42%) died from coronary heart disease (CHD), 6.7 (38%) million from stroke. According to WHO estimates, by 2030, about 23.6 million people will die annually from CVDs. The annual overall mortality of the population is, according to various sources, 1.2–2.4%, while cardiovascular mortality (CVM) is 0.6–1.4%, the incidence of non-fatal myocardial infarction (MI) is from 0.6 (according to the RITA-2 study) to 2.7% (according to COURAGE). At the same time, in very high-risk patients, the annual mortality rate increases to 3.8%, while in persons with hemodynamically insignificant atherosclerosis of the coronary arteries, the mortality rate is at the level of 0.63% (data from the REACH registry). CVD is the leading cause of death in the Russian Federation, contributing 57% to overall mortality. CVD is also the most common cause of hospitalization and disability in the Russian population. The economic damage from CVD in the Russian Federation is about 3% of the country's gross domestic product. The mortality curve from CVD in the Russian Federation has a wave-like shape: from 1991 to 1994 it increased from 621 to 836 cases per 100 thousand population, then there was a decline to 747 cases in 1998, after which the mortality rate increased again to 927 cases in 2003 d. From that moment to the present, there has been a relatively stable trend towards a decrease in mortality from CVD, which in 2013 amounted to 698.1 cases, in 2014 – 653.7 per 100 thousand population. However, these indicators are still among the highest in the world, exceeding similar indicators in developed countries by 4–6 times [1]. Therefore, an important point remains the individualization of approaches to the correction of risk factors depending on the severity of the disease. In this regard, it is advisable to introduce a fifth risk category, which will make it possible to justify and carry out the most intensive treatment using drugs that have proven their influence on achieving not only certain parameters and indicators, but also significantly reducing the risk of cardiovascular complications (CVC). It is proposed to call such a group an extreme risk group (ER). Thus, patients can be divided into five risk categories - low, moderate, high, very high and extreme.
Rationale for introducing the ER category
As is known, the category of very high CVD risk includes a fairly broad category of patients, among which there are patients with the presence of several pathologies, each of which falls under this category [2]. There is no doubt that their combination significantly increases the risk of complications. This dictates the need to identify an additional category, which is proposed to be defined as the ER group. This will introduce more stringent requirements for the control of risk factors for these patients, which should have a positive impact on the incidence of cardiovascular events and mortality in this most severe category.
Indeed, at present, both a patient with IHD and a patient who has a combination of IHD with type 2 diabetes mellitus (T2DM) and circulatory failure can be classified as a very high risk category. However, the cardiovascular risk (CVR) in the second case is undoubtedly much higher. In particular, the combination of T2DM with CVD significantly worsens the prognosis. In this regard, recently in the treatment of T2DM there has been a transition from a “glucocentric” approach to a more global tactic, with the main goal of reducing the incidence of cardiovascular events [3]. It is not so much the absolute levels of fasting plasma glucose and the level of glycosylated hemoglobin (HbA1c) that become important, but the safety of the drugs used in a particular case and their ability to reduce the incidence of cardiovascular events. This approach is similar to what was previously proposed to combat arterial hypertension: it is not so much the hypotensive effect of therapy itself that is important, but its effect on cardiovascular risk [4]. In 2021, the National Atherosclerosis Society (NSA) proposed more stringent low-density lipoprotein (LDL) cholesterol targets. In very high-risk patients, the target LDL level should be 1.5 mmol/L or lower [2]. This LDL level may also be one of the treatment targets for patients with ER.
The ER category was officially designated in the 2021 guidelines by the American Association of Clinical Endocrinologists and the American College of Endocrinologists (AACE) [5].
These guidelines include patients with the following conditions as ER:
- Progression of CVD caused by atherosclerosis, including unstable angina in patients with LDL levels less than 1.8 mmol/l.
- Clinically significant CVD in patients with diabetes, chronic kidney disease (CKD) stage 3–4. or with heterozygous familial hypercholesterolemia (heFH).
- Development of CVD in men under 55 years of age or women under 65 years of age.
In table 1 presents the gradation of risk categories and treatment tactics proposed in these recommendations.
As follows from the table. 1, the definition of risk categories is slightly different from that presented in the 2021 NOA Recommendations. Taking into account the existing Russian recommendations for the correction of lipid metabolism disorders and based on a number of clinical studies described below, the following definition of ER for the Russian population is advisable: a combination of clinically significant CVD, caused by atherosclerosis, with T2DM and/or FH, CVS in a patient with CVD caused by atherosclerosis, despite optimal lipid-lowering therapy and/or achieved LDL level ≤1.5 mmol/l. In this case, CVD caused by atherosclerosis should include ischemic heart disease, ischemic stroke or transient cerebrovascular accident, and ischemia of the lower extremities.
Thus, with the introduction of the ER category, the classification of cardiovascular risk categories takes on the following form (Table 2).
As can be seen from table. 2, ER patients are required to achieve a target LDL level of ≤1.5 mmol/L. However, there is reason to believe that a target LDL level of ≤1.3 mmol/L would be more optimal. At the moment, the evidence base for a lower target LDL level is only developing, which does not allow it to be recommended as mandatory.
In order to facilitate the work of doctors, it is advisable to develop an electronic application for mobile devices, in which, after the doctor fills out the appropriate fields, the risk category will be shown, target LDL levels will be given and therapeutic tactics will be described.
In addition to changing the treatment tactics for these patients, the identification of an ER group may make it possible to influence the preferential drug provision for patients included in this group.
Treatment tactics for patients with ER
Patients in this group require correction of risk factors: arterial hypertension, physical inactivity, abdominal obesity; quitting smoking, using a Mediterranean or Nordic diet. Monitoring of Lp(a) levels is recommended, with a target HbA1c level of <7%.
Patients with a total cholesterol level of more than 7.5 mmol/l and/or an LDL level of more than 4.9 mmol/l must exclude the presence of FH.
For this purpose, it is advisable to use the Dutch criteria. In addition, if FH is suspected, cascade screening with examination of first- and second-degree relatives is required [6]. If a familial disorder of lipid metabolism is suspected, if possible, a genetic examination of the patient should be performed using NGS (Next Generation Sequences) technology to exclude mutations in the genes encoding the production of LDL receptors, LDL receptor modulator protein, apoB, PCSK9. If a mutation is detected in cascade screening cancers in first-degree relatives of the index patient, genetic analysis should be performed using SNP (Single Nucleotide Polymorphism) technology.
When choosing antihypertensive therapy for patients with ER, the target blood pressure (BP) level should be ≤130/80 mmHg. (and not lower than 120/80 mm Hg), but only if achieving such a blood pressure level is possible without significant side effects of antihypertensive therapy [7].
For patients with ER, the mandatory requirement is to achieve a target LDL level of ≤1.5 mmol/L, an optimal level of ≤1.3 mmol/L. Its achievement is expected by enhancing lipid-lowering therapy, namely statin therapy (atorvastatin or rosuvastatin) in maximum tolerated doses in combination with ezetimibe; in some cases, combination with PCSK9 inhibitors is possible as a third component. Achieving the target LDL level in this group of patients is a priority, so it is necessary to use the entire available arsenal of lipid-lowering drugs. When choosing statin drugs, preference should be given to original statins. In case of CKD with GFR <60 ml/min/1.73 m2, atorvastatin at a dose of 40–80 mg/day should be considered as a first-line drug. For patients with CKD and reduced GFR, the use of atorvastatin is more preferable than rosuvastatin, as was shown in the studies with the original atorvastatin - PLANET I and PLANET II. Despite the fact that rosuvastatin reduced LDL levels more significantly, atorvastatin demonstrated a more pronounced renoprotective effect in CKD patients with and without diabetes [8]. In addition, when studying the effect of statins on the time of development of cardiovascular events compared with placebo, it was shown that the time to divergence of the curves was shorter in studies with statins compared to non-statin lipid-lowering drugs - 10.3 versus 20.0 months. Among studies with statins, the time to divergence is shorter in studies with atorvastatin compared with other statins: 4.75 versus 11.4 months [9]. When choosing a specific drug atorvastatin, it is necessary to take into account its evidence base.
There is evidence that a target LDL level of ≤1.3 mmol/L may be preferable for patients with ER, but the evidence base for such a recommendation is currently insufficient.
Below is data on this issue.
In the case of a combination of ER with T2DM, empagliflozin and/or liraglutide should be used as antihyperglycemic therapy along with metformin. When T2DM is combined with chronic heart failure (CHF), preference is given to empagliflozin; when proven CVD is combined with T2DM, empagliflozin or liraglutide is preferred; when CVD, T2DM and obesity are combined, liraglutide is preferred.
IMPROVE-IT, FOURIER and ODYSSEY Outcomes: clinical studies supporting the need for more intensive LDL-lowering in ER patients
One of the first studies to demonstrate the benefit of greater LDL-C reduction in individuals with very high ER was the IMPROVE-IT trial. Patients who had undergone ACS were included, and the effects of lipid-lowering therapy with statins alone and combination therapy with a statin and ezetimibe were compared. The primary endpoint was cardiovascular death, myocardial infarction, unstable angina, and PCI. In the intensive control group, the LDL value was 1.369 mmol/l. During treatment for 7 years, Kaplan-Meier survival analysis showed that the incidence of the end point in the intensive therapy group was significantly lower compared to conventional therapy - 32.7 versus 34.7%. The relative risk (RR) decreased by 6.4% (RR=0.936, 95% confidence interval [CI] - 0.89-0.99; p=0.016). The absolute risk reduction was 2%. Analysis of a subgroup of patients with diabetes (27% of all included in the study) demonstrated a decrease in RR by 14.4% (RR = 0.856, 95% CI - 0.779–0.939) in the intensive therapy group and only 2.3% in the standard treatment group ( RR=0.977, 95% CI – 0.915–1.044; p=0.023). Dividing patients into other subgroups (depending on smoking, hypertension, history of PCI, creatinine level) did not demonstrate a significant difference in the subanalysis [10].
The FOURIER study examined the effect of more intensive lipid-lowering therapy in individuals with very high ER. The additional effect of adding evolocumab to standard lipid-lowering therapy was studied. The primary endpoint was MI, cardiovascular death, stroke, PCI, and unstable angina. 27.5 thousand patients were included, the duration of the study was 2.2 years, the study was placebo-controlled. In the evolocumab group, the mean LDL level was 0.775 mmol/L. Against this background, 9.8% of patients in the evolocumab group and 11.3% in the comparison group reached the end point. Thus, intensive lipid-lowering therapy allowed an additional 20% reduction in risk (95% CI – 0.73–0.89). It was after this study that the AACE proposed to distinguish the ER category and use lower target LDL levels [11].
In addition, in 2010, the CTT (Cholesterol Treatment Trialists') Collaboration conducted a meta-analysis of 26 clinical trials involving 169,138 patients. Groups of patients with ACS, stable coronary artery disease, T1DM (337 patients), T2DM (5414 patients), and CHF were considered. All cases demonstrated an additional 24% reduction in risk for every 1 mmol/L reduction in LDL cholesterol. In addition, it has been shown that the lower LDL levels are reduced, the greater the risk reduction. Even for individuals with an initial LDL level <2.0 mmol/l, a decrease of every 1 mmol/l reduces the risk of significant cardiovascular events by 29%, in individuals with an initial LDL level <1.8 mmol/l - by 37% [12]. In another 2014 meta-analysis, which included 38,153 patients, patients were divided into groups depending on the achieved LDL level: 1.3 mmol/L, 1.9; 2.6; 3.2; 3.9 mmol/l. Compared with a level of 3.9 mmol/l in the group of patients with an LDL level of 1.3 mmol/l, the reduction in the relative risk of cardiovascular events was 0.44 (95% CI - 0.35–0.55). When comparing a group of patients with LDL levels of 1.3 and 1.9 mmol/l, the reduction in RR was 0.81 (95% CI - 0.70–0.95). Thus, when the level of LDL <1.3 mmol/l, non-HDL cholesterol <1.9 mmol/l, and apoB <50 mg/dl are achieved, the lowest level of cardiovascular events is observed [13].
Similar results were shown by the ODYSSEY Outcomes study (the number of included patients was 18,924) [14]. Treatment with alirocumab demonstrated a reduction in the RR of cardiovascular events, regardless of baseline LDL-C. There was a significant reduction in absolute risk in the group of patients who achieved LDL levels ≥2.5 mmol/L of 3.4% for the primary composite endpoint and 1.7% for overall mortality. The reduction in RR was 15%.
Features of treatment of patients with ER in combination with T2DM
Empagliflozin is the first antihyperglycemic drug to demonstrate in a large, prospective, multicenter, double-blind, phase III EMPA-REG Outcome study (NCT01131676) not only safety, but also the benefits of use - reducing the incidence of cardiovascular events and improving outcomes associated with heart failure (HF) in patients with T2DM and established cardiovascular diseases and high cardiovascular risk.
The EMPA-REG Outcome study was conducted at 590 clinical centers in 42 countries and included 7020 patients (71% of them men) with T2DM and confirmed CVD, with an average follow-up of more than 3 years. Patients were divided into two groups and received empagliflozin or placebo in addition to standard therapy, which included drugs with proven ability to reduce the incidence of cardiovascular events. The primary composite endpoint included cardiovascular death, nonfatal MI (excluding silent MI), and nonfatal stroke (3P-MACE); The secondary composite endpoint also included hospitalizations due to HF. The study continued until at least 691 patients experienced standardized assessment events that met the primary endpoint.
The EMPA-REG Outcome study demonstrated a 14% reduction in the rate of achievement of the primary endpoint 3P-MACE (p=0.038). At the same time, the results for each of the components of the combined point were different: overall mortality decreased by 32% (p<0.001), cardiovascular disease - by 38% (p<0.0001), the frequency of non-fatal myocardial infarction decreased significantly by 13% (p=0. 22), the frequency of non-fatal stroke, on the contrary, tended to increase (by 24%; p=0.22), and the overall frequency of death from non-cardiac causes only tended to decrease (by 16%; p=0.29). At the same time, a decrease in mortality in the empagliflozin group was observed at the early stage of the study (<3 months) and was noted in all subgroups of those examined.
The incidence of hospitalization for HF decreased by 35% (p=0.002), incl. by 37% among patients who did not have HF at baseline, and by 28% among patients with HF diagnosed at baseline. The rate of hospitalization or death due to HF decreased by 39%, the number of new cases of HF (according to the criteria established in the study for HF, in particular HF with left ventricular ejection fraction <35%) - by 30%; the frequency of composite outcomes (hospitalization for HF or prescription of loop diuretics) – by 37%.
Thus, the EMPA-REG Outcome study demonstrated not only the cardiovascular safety of empagliflozin, but also its clear protective cardiovascular effects in the form of a reduction in the incidence of cardiovascular events and improvement in indicators characterizing the course of HF in patients with T2DM [15].
The effect of the glucagon-like peptide analogue liraglutide on cardiovascular system was demonstrated in the placebo-controlled LEADER study. Primary composite outcome: cardiovascular death, nonfatal MI, nonfatal stroke. 9340 patients were included, and the follow-up period was 3.8 years. The primary end point was recorded significantly less often in the liraglutide group - 608 (13.0%) out of 4668 patients than in the placebo group - 694 (14.9%) out of 4672 patients (RR = 0.87, 95% CI - 0. 78–0.7; p<0.01 for noninferiority; p=0.01 for superiority). CV risk in the liraglutide group was 4.7%, in the placebo group – 6.0%; p=0.007, mortality from any cause was also lower in the liraglutide group – 8.2 versus 9.6% in the placebo group (p=0.02). The incidence of MI, stroke and CHF was also lower in the liraglutide group [16].
Conclusion
Due to the fact that the first manifestation of CVD may be cardiovascular death, it is extremely important to identify patients at high risk levels not only at the stage of the appearance of clinical symptoms, but also before the occurrence of such manifestations. It should be emphasized that the danger is not the degree of stenosis of the coronary or carotid arteries, but the condition of the atherosclerotic plaque. However, at the present stage of development of cardiology, there are no reliable non-invasive methods to identify unstable atherosclerotic plaques. Therefore, it is extremely important to assess the patient’s risk category to determine treatment tactics. Among the risk factors for cardiovascular disease, 4 main ones should be identified: hypertension, dyslipidemia, smoking, T2DM/impaired glucose tolerance.
There are two main multidirectional errors in identifying patients with coronary artery disease – overdiagnosis and underestimation of the degree of risk. Frequent reasons for an unfounded diagnosis of coronary artery disease are the presence of pain in the chest without proof of its ischemic origin, advanced age and changes in the final part of the ventricular complex on the electrocardiogram (ECG). Underestimation of the risk stems from the fact that treatment, as a rule, is started only in the presence of hemodynamically significant stenosis. In addition, PCI is unjustifiably widely used. However, it has been shown that in stable CAD, endovascular treatment does not affect the prognosis [17] and does not in all cases affect the quality of life [18].
To increase the effectiveness of the fight against special forces, it is advisable to make the following adjustments:
- if there are risk factors or if there is a suspicion of CVD caused by atherosclerosis, it is necessary to determine the risk category;
- when diagnosing coronary artery disease, one should be guided by the data of instrumental methods confirming the presence of myocardial ischemia: myocardial perfusion scintigraphy or stress echocardiography. Detecting coronary artery disease using ECG at rest and 24-hour ECG monitoring is impractical;
- When identifying patients with HF, it is necessary to measure the level of natriuretic peptide in the blood in addition to chest x-ray and echocardiography. This is especially true for patients with heart failure with preserved ejection fraction;
- in the presence of CVD caused by atherosclerosis, the prescription of lipid-lowering therapy is mandatory, regardless of the initial LDL level.
- In patients with T2DM, statin therapy is mandatory regardless of the initial LDL level. When choosing antidiabetic therapy, drugs that reduce the risk of cardiovascular complications should be used;
- pacemakers should be used more widely, incl. with the function of cardioverter-defibrillators, in cases where this meets the requirements of the recommendations [19].
Thus, the introduction of an additional risk category should promote closer attention to patients with ER, to more stringent and frequent monitoring of their lipid profile, HbA1c, and blood pressure. Patients in this category require close attention to the correction of risk factors and adherence to prescribed therapy, more careful instrumental monitoring, in particular, duplex scanning of extracranial arteries and arteries of the lower extremities. In the case of diabetes, it is advisable to manage such patients jointly by a cardiologist and an endocrinologist. Acceptance of this risk category will increase the motivation of both patients and their attending physicians, which should help reduce the risk of developing cardiovascular complications.
The science of the marathon runner or how running affects the cardiovascular system
While running, your heart rate increases and your blood pressure rises. The heart works under increased load. Therefore, with moderate intensity loads, a positive training effect on the cardiovascular system is noted. But with too intense and frequent exercise, there is a negative effect on the cardiovascular system. And if there are pronounced atherosclerotic plaques in the vessels, then such loads can lead to insufficient vasodilation and ischemia (reduced blood supply) in organs and tissues, or even to rupture of plaques with subsequent thrombus formation.
Therefore, before running intensively, especially after 40 years, if you smoke or have smoked before (even 15 years ago), if you have high blood pressure or blood glucose, you must first be examined by a cardiologist who will conduct stress tests.
It is a myth that you either need to run regularly or it is better not to engage in physical activity at all, because sudden exercise is harmful to the heart. It is always better to practice some physical activity than not to do any physical activity at all. For example, the clinical guidelines of the European Society of Cardiology for the prevention of coronary heart disease (September 2021) recommend aerobic (dynamic) exercise of 150 minutes per week (30 minutes per day, 5 days a week). Best: Walking until mildly tired, or 75 minutes per week of vigorous aerobic activity (15 minutes 5 times a week - such as jogging or a combination of these activities) and oxygenating aerobic activity (this could be cycling, swimming or tennis). At any age, walking 2 times a week for 1.5-2 hours (8-10 km) is useful, but not in strong winds and cold. There is no need to suddenly start exercising very intensively; the load is usually increased gradually.
What kind of punishment will you face if you don’t assess the profrisks?
The assessment is required for all employers - if the company employs at least one employee under an employment contract (including external part-time workers). Therefore, the absence of a labor safety specialist on staff is not a basis for failure to conduct a risk assessment , and, accordingly, for non-compliance with labor safety rules.
The status of risk assessment increased significantly after the procedure was specified in the labor protection rules, which are a regulatory legal act registered with the Russian Ministry of Justice. Part 1 of Article 5.27.1 of the Code of Administrative Offenses interprets the failure to conduct and apply the results of a risk assessment as a violation of state regulatory requirements for labor protection contained in other legal regulations of the Russian Federation.
The fine for a company will be up to 80,000 rubles, and for an individual entrepreneur or an official of an organization - up to 5,000 rubles.
Everyone needs cardiology
Many people have a strong opinion that cardiology is a field of science for those “over 50.” But according to estimates from the National Research Institute, in Russia 59% of women and 54% of men over 20 years of age are overweight, and 15% and 28.5% are obese. That is, every third Russian of working age is overweight or obese - risk factors for cardiovascular diseases. An unhealthy lifestyle, which leads to the development of cardiovascular diseases, most often develops in childhood and adolescence, and over time, the risk of cardiovascular diseases only increases. Therefore, prevention should begin from childhood.
There are no nerve endings in the vessels, they do not hurt. Therefore, their defeat occurs gradually and symptoms appear only when complications develop: ischemia or infarction of organs, more often after 50 years in men and after 60 years in women. But the processes that cause irreversible changes begin much earlier and are easier to prevent. Therefore, all men after 40 years of age and women after 50 years of age need to undergo preventive examinations by a cardiologist with ultrasound examinations, biochemical markers and stress tests.
If there is a family history of early heart attacks or strokes, if the patient is a smoker or suffers from diabetes, if he has high blood pressure or chronic kidney disease, if the person simply does not tolerate physical activity, then you should definitely come to a cardiologist at an earlier age than 50 or 40 years. And the sooner the better.
Evidence-based medicine and myths of cardiology
Until the 90s, Russian cardiologists treated based on the opinions or views of different medical schools, which often did not agree with each other on scientific research. When the massive advent of computers helped to introduce the principles of evidence-based medicine everywhere, uniform requirements for conducting scientific research were formulated. When evaluating drugs, double-blind randomized studies have begun to be used, which are highly accurate and impartial. We created a unified knowledge base and assessment of all research conducted in the world that corresponds to a high scientific and technical level. As a result, the efficiency and safety of diagnosing and treating patients has dramatically increased.
A myth that all doctors face, but which is especially dangerous in cardiology, can be expressed in one common phrase: “Don’t take medicine, you’ll destroy your liver.” Medicines are metabolized in the liver and eliminated through the liver or kidneys, but they do not destroy them. Canceling the selected therapy can lead to a sharp increase in blood pressure, cholesterol levels and other indicators. This aggravates diseases from heart attack and stroke to diabetic coma. Surprisingly, patients are not afraid to take dietary supplements (dietary supplements) or alcohol in any quantity.
The second common myth in the practice of a cardiologist is the erroneous opinion about the dangers of cholesterol-lowering drugs - statins. A large number of studies based on the principles of evidence-based medicine confirm the high effectiveness of this group of drugs in preventing the development of atherosclerosis and its consequences (heart attack, stroke, damage to the arteries of the legs, intestines); these drugs are included in all generally accepted recommendations. Statins require constant, simple laboratory monitoring in order to avoid fairly rare side effects. Individual intolerance occurs when using any medicine or even food product. When using statins too, but rarely.
Conducting professional risk assessments with specialists
A company can conduct a risk assessment independently, or it can delegate this task to a specialized organization .
Not everyone, even the most experienced occupational safety specialist, is able to personally conduct a risk assessment. Yes, he can organize the work, but it takes teamwork to complete the assessment. This is especially true for manufacturing enterprises and large businesses. We advise you to involve external experts or send members of your internal commission for training for such a complex task as assessing profrisks. You can competently assess the profit risks in your company here >>>
Remember that having a third-party risk assessment provider has the obvious advantage of providing a fresh, independent perspective on your business's problems. Professionals from a specialized organization for labor protection are “sharpened” on assessment, master various techniques, constantly improve their skills, participate in round tables and conferences.
To avoid claims from the GIT inspector, entrust the risk management to experienced professionals. Read our article Occupational Risk Assessment: Which Company to Engage .
About medical examination
Clinical examination in the field of cardiology is one of the main measures to reduce mortality from cardiovascular diseases. There is a clearly defined concept of risk factors that must be controlled and treated for a long and fulfilling life. Therefore, clinical examination including cardiac examination is indicated for all men over 40 years of age and women over 50 years of age.
How risk category affects the frequency of inspections
| RISK CATEGORY | HOW OFTEN ARE INSPECTIONS OF ANY KIND ALLOWED? |
| Extremely high risk | The maximum frequency of planned control (supervision) activities is at least one, but not more than 2 per year |
| High or significant risk | Average frequency of holding – at least one event every 4 years and no more than one every 2 years |
| Medium and moderate risk | The minimum frequency of planned control (supervision) activities is at least one every 6 years and no more than one every 3 years |
Thus, the types and frequency of planned control (supervisory) activities depend on the assigned risk category (Article 25 of Law No. 248-FZ).
The regulation on the type of control may establish:
- reduced time frames for control (supervision) activities;
- features of their content;
- volume of submitted documents, instrumental examination, tests, examinations and experiments.
“Smart” gadgets are an assistant in heart control
I really like modern devices that allow you to assess how much work a person did during the day, how many steps and kilometers he walked, and what his heart rate was. This is useful, since the load level is often calculated based on the pulse. I also like devices that allow you to evaluate the duration and quality of sleep (by sleep phases). This is a very useful feature for people living in the modern world, when both pleasure and work are prolonged due to sleep. Meanwhile, only in sleep the body is restored, healed and absorbs daytime information. “Smart” gadgets are my favorite gift to everyone who is dear to me.