37th week of pregnancy for baby
At the 37th week of pregnancy, the baby’s height is approximately 48 cm, and his weight is 2,600 g. Externally, the fetus is almost no different from a newborn; all facial features are developed, and cartilaginous tissue is clearly visible. The accumulation of subcutaneous fat at this stage of pregnancy makes the body contours softer and rounder. The baby’s skin gradually smoothes out, it is no longer as pink as in the previous weeks of intrauterine development, and the integument gradually becomes lighter. The baby's body is still abundantly covered with lubricant, but the amount of vellus hair decreases noticeably, vellus hair remains only on the shoulders and back, and in some babies it disappears almost completely.
This week the accumulation of fatty tissue continues. It reaches a maximum of 15% of the child’s total body weight. It is difficult to overestimate the importance of adipose tissue for newborns; it is this tissue that protects the child from overheating or hypothermia, since the baby’s thermoregulation system after birth is not yet sufficiently formed and continues to develop in the first months of the little person’s life.
At this stage, not only the volume of subcutaneous fat increases, but also the muscles and skeleton intensively develop. The child constantly moves his arms and legs. These unique workouts help increase muscle mass. The baby also makes rhythmic breathing movements that strengthen the intercostal muscles and diaphragm, preparing the respiratory organs for childbirth.
Pregnant woman at 37 weeks
As the due date approaches, pregnant women begin to notice the appearance of their precursors, that is, certain signs and changes that occur under the influence of hormones. A woman’s body is preparing to give birth to a child, progesterone gives way to the dominant role of the birth hormone estrogen, and the pregnant woman’s well-being changes.
From the 37th week, expectant mothers may observe the following changes:
- slight loss of body weight;
- reduction in abdominal volume;
- the appearance of training or “false” contractions and an increase in their intensity;
- discharge of mucus from the cervix.
The nature of the stool changes, it becomes weaker, aching pain in the lower back of varying intensity may appear, and the fundus of the uterus descends. The woman notes some signs on her own, others are observed by the gynecologist during a routine examination.
Precursors do not appear in all women. Some expectant mothers notice only some of the symptoms listed above, while others observe signs of impending labor not two or three weeks before the due date, but just a few hours. Both the appearance of precursors at the 37th week and their absence are normal and depend on the individual characteristics of the woman’s body.
This week, the female body is intensively preparing for the birth of a child. If the fetus is positioned correctly, head down, it gradually lowers, goes to the lower part of the uterus, presses it to the body and bends its limbs, intuitively taking the most comfortable position for passing the birth canal. The consequence of fetal movement is prolapse of the uterine fundus. The abdomen lowers, the pressure on the diaphragm decreases significantly, the pregnant woman can breathe easily, and the shortness of breath that plagued her in the previous weeks disappears. The pressure on the stomach also decreases, heartburn, a feeling of heaviness after eating and other unpleasant sensations disappear. Moving your baby can put pressure on your bowels and bladder. A pregnant woman at this stage often experiences the urge to urinate and may suffer from frequent loose stools. The reason for frequent bowel movements is not only the mechanical effect of the uterus on it, but also an increase in the content of estrogen in the body, hormones that promote the excretion of fluid. At the 37th week, the expectant mother can have bowel movements up to 3-4 times a day and at the same time observe significant dilution of the stool.
Is coronavirus dangerous for pregnant women?
Respiratory diseases in pregnant women are generally more severe and cause more complications. Doctors explain this by saying that during pregnancy the immune system weakens in order to protect the fetus from the risks of an accidental attack from the mother’s immune system. The downside of this mechanism: the body becomes more susceptible to colds and infectious diseases.
In general, the risk of contracting a coronavirus infection in pregnant women is the same as in everyone else. They are often asymptomatic, and if they have symptoms, they are mild or moderate. The most common clinical manifestations of the disease are fever, cough and myalgia (muscle aches). In addition, fatigue, diarrhea, shortness of breath, and sore throat are common. Overall, most pregnant women experience COVID-19 in the same way as others.
But the chances of getting seriously ill and dying from COVID-19 are still higher. An international study organized by scientists at the University of Oxford and conducted in 18 countries (including Russia) showed that the risk of severe complications is increased in both mother and child. And according to a comparative review of studies involving 10 thousand pregnant and 128 thousand non-pregnant women, the former have almost twice the risk of death. It is just over 11%.
38th week of pregnancy: development of the unborn baby
At the 38th week, the fetus is fully formed, so childbirth at this stage is no longer dangerous for both mother and baby. The weight of the fetus is about 3 kg, but this figure can vary significantly between babies; the weight depends on the individual characteristics of the mother and child, body structure and other factors. The body length of a newborn is approximately 50 cm.
All organs and systems at a period of 38 weeks are characterized by physiological and morphological maturity, they are completely ready for work. At this stage, the baby is preparing for childbirth, making breathing movements and preparing the intercostal muscles for breathing. The lung tissues are washed with amniotic fluid, which helps maintain the required level of surfactant covering the baby's lungs from the inside. All elements of the respiratory system are ready for use. With the first breath after birth, the alveoli begin to transfer oxygen from the air into the blood, gas exchange occurs, and the respiratory and circulatory systems begin to work intensively.
Mucolytic therapy for acute respiratory infections in pregnant women
R.A. BONTSEVICH
, Ph.D.,
O.V.
GOLOVCHENKO , Candidate of Medical Sciences,
State Budgetary Institution "St. Joasaph Regional Clinical Clinical Hospital"; Belgorod Research State University Acute respiratory diseases (ARI) are one of the most common pathologies in pregnant women.
During pregnancy, about 2/3 of women experience one or more episodes of acute respiratory infections of varying severity. The significance and importance of studying this problem is due to the fact that in a certain percentage of cases, pathogens of acute respiratory infections can directly or indirectly cause damage to the fetus or disrupt the normal course of pregnancy. The issues of optimal treatment of acute respiratory infections, one of the main manifestations of which is cough syndrome, are insufficiently studied. The paper discusses the features of acute respiratory diseases (with the exception of pneumonia) in pregnant women. The experience of our own use in the complex therapy of cough syndrome of the drug ambroxol is presented. Modern medical science considers various viral infections as one of the main causes of reproductive losses. Viral agents in acute respiratory infections (ARVI) in some cases can have a direct damaging effect on the fetus, in addition, they lead to complex changes in the reactions of the maternal body, which leads to a complicated course of pregnancy [1, 2]. The drugs themselves used for treatment can also cause pregnancy disorders [3, 4].
Epidemiology
The incidence of various acute infections of the respiratory system (ARVI, influenza, pharyngitis, tracheitis, bronchitis) is, according to various sources, from 50 to 75% during pregnancy. Most often, women experience mild or moderate acute respiratory viral infection episode(s). Up to 30% of pregnancy episodes are accompanied by acute bronchitis. The seasonality of the disease is characteristic: people get sick more often in the autumn-spring and winter periods, during epidemics of ARVI/flu [2, 5, 6].
Etiology
The main causative agents of acute respiratory infections are viruses. A significant role belongs to influenza, parainfluenza, adeno-, rhino-, corona and enteroviruses. The proportion of viral infection increases during characteristic epidemic periods and seasonally. Bacterial flora can also cause a number of diseases: pharyngitis, laryngitis, tracheitis, bronchitis [5, 7, 8].
Risk factors
The risk group for infection with acute respiratory infections includes women with concomitant background diseases and dysfunctions of various organs and systems (respiratory, cardiovascular, digestive, endocrine, immune). And also people who often suffer from acute respiratory infections (three or more times in the year preceding pregnancy), which indirectly confirms the patient’s immunological deficiency (more pronounced than the natural decrease in immunity against the background of normal pregnancy). Such individuals are characterized by a protracted, recurrent course of diseases (rhinitis, pharyngitis, tracheitis, bronchitis), the presence of foci of chronic infection (chronic tonsillitis, sinusitis, bronchitis). A particularly significant role in the risk of developing acute respiratory infections is played by chronic pathology of the respiratory system, background tobacco smoking and pathology of the digestive tract (dysbacteriosis and chronic intestinal diseases) [5, 6, 9].
Pathogenesis and complications of gestation
The causative agent of acute respiratory infections enters the mother's body through the upper respiratory tract, penetrates the cylindrical ciliated epithelium, where its active reproduction occurs, which leads to cell damage and an inflammatory reaction. In severe forms of the disease (influenza), all parts of the airways can be involved, up to the alveoli, with the development of complications in the form of acute bronchitis, sinusitis, otitis, pneumonia 10.
The infectious agent that causes acute respiratory infections can have an adverse effect both on the course of pregnancy and directly on the fetus (fortunately, this is rare). Thus, viruses that cause most acute respiratory infections (i.e., in fact, these are acute respiratory viral infections) are especially dangerous in the 1st trimester, when they can cause embryopathic, teratogenic, fetopathic effects and termination of pregnancy; and influenza suffered in the 1st trimester increases the likelihood of developing schizophrenia in a child [8, 11]. At later stages, acute respiratory infections can disrupt the physiological course of pregnancy, causing functional disorders in the mother and fetus, in some cases leading to pregnancy failure, infection of the fetus with subsequent postnatal manifestations [2, 12].
The national obstetrics guidelines highlight the following complications of gestation in acute respiratory infections: the formation of malformations (if infected in the 1st trimester of pregnancy - from 1 to 10%), the threat of miscarriage in 25–50% of cases, intrauterine infection of the fetus, placental insufficiency with the formation intrauterine growth retardation and chronic fetal hypoxia, placental abruption in 3.2% of cases 10.
In the case of bacterial infection during acute respiratory infections, there are also some risks. Firstly, indirect – from a violation of the functional status of the mother and fetus against the background of this infection. And secondly, a direct effect of the bacterial agent on the fetus is potentially possible if it is tropic to the reproductive system: transplacental infection with the development of chorioamnionitis and damage to the fetus. This is most likely in the presence of “atypical” pathogens of acute respiratory infections (mycoplasma, chlamydia), since intracellular agents related to them also cause classical urogenital and reproductive infections. In addition, certain risks exist in the presence of staphylococcal, streptococcal and gram-negative infections (E. coli, etc.). The following possible and probable mechanisms of the pathogenesis of gestational disorders against the background of acute respiratory infections are identified [1, 8, 9].
1. Immunotropic changes in the body that occur under the influence of infection. Usually these are immunodeficiency changes that aggravate the physiological immunodeficiency of pregnant women. Sometimes disturbances can activate diseases that were previously in a latent and inactive form (bronchial asthma, allergies, systemic and autoimmune diseases). Activation of chronic foci of infection, including intrauterine. 2. Due to the toxic effect on the endothelium, disturbances in the hemostasis and blood systems are possible, manifested by either hypo- or hypercoagulation, thrombocytopenia and, consequently, an increased risk of bleeding or thrombosis. 3. Oxygen starvation of the mother and fetus, associated with the toxic effect of the infectious agent on the tissues of the respiratory system and the vascular bed. 4. In rare or specific cases (as, for example, with rubella) – transmission of viruses/bacteria of the respiratory group through the placenta from a sick mother to the fetus with the occurrence of intrauterine infection/disease. 5. Infection of the placenta with the possible development of chronic inflammation and persistent infection can lead to the formation of structural changes in the placenta, the formation of uteroplacental insufficiency and, as a result, increase the likelihood of developing preeclampsia (nephropathy, gestosis of the 2nd half of pregnancy).
Features of the course of acute respiratory infections in pregnant women
Typically, pregnant women have acute respiratory infections with a mild or moderate course of the disease. The exception is influenza, especially pandemic strains, which can be very severe (especially in the 3rd trimester), causing respiratory distress syndrome, severe respiratory failure, pneumonia, and requiring mechanical ventilatory support (ventilatory support). Also, pregnant women are characterized by a protracted course of acute respiratory infections. The main prolonged symptom is cough, usually in the form of a non-productive cough of moderate or low intensity, sometimes of a paroxysmal nature. Also typical is prolonged malaise, weakness, fatigue, dyspnea, low-grade fever, unstable blood pressure, with a tendency to hypotension. In some cases, such “erased” symptoms are incorrectly assessed by attending physicians as vegetative-vascular dystonia, etc. 5, 10.
With the leading cough symptom (acute bronchitis), the following features can be noted:
1) the presence of a long-term “initial” non-productive cough of moderate or significant intensity, often of a paroxysmal nature; 2) fairly rapid transformation into a productive one during therapy and a rapid (within several days) reduction of the cough symptom; 3) long-term “residual” unproductive cough of moderate or low intensity, with a rather poor response to typical “weekly courses” of bronchitis therapy (as a result, often after 3-6 weeks of sluggish residual effects, such patients seek consultation with a referral diagnosis of “chronic bronchitis”, "BA") Thus, pregnancy itself after suffering from an acute respiratory infection acquires a number of features. The most likely complications after acute respiratory infections may be [5, 9]:
formation of placental insufficiency (more than doubling of frequency is noted), progression of existing chronic placental insufficiency; early gestosis (preeclampsia); oligohydramnios (an accompanying sign of placental insufficiency, as well as a manifestation of viral damage to the fetoplacental complex); threat of premature termination of pregnancy (usually in the 2nd trimester, namely in the period 17–26 weeks); after acute respiratory viral infection, a constant course of threatened miscarriage is characteristic, insensitive to standard therapy; intrauterine growth retardation and intrauterine fetal hypoxia; increase in the general morbidity of newborns; hypoxic damage to the central nervous system (most typical for ARVI in the 2nd trimester) 1, 8, 9].
Treatment
Treatment of most diseases in pregnant women is associated with a lack of evidence on the safety of a significant part of potentially indicated drugs. In recent years, attempts have been made by the global scientific community to create registries and databases on the use of drugs in pregnant women. In our country, only the first steps are being taken in this direction, therefore, in practical activities, doctors and scientists are guided by information from the FDA register, European analogues, specialized sites (www.reprotox.org, https://www.motherisk.org, domestic project - babyrisk.ifo, etc.) [4].
Currently, various recommendations for the treatment and prevention of acute respiratory infections in pregnant women contain the following main groups of drugs and agents [5, 6, 8, 11].
1. Preventive vaccination. Recommended as an anti-influenza vaccine in case of a significant deterioration in the epidemiological situation (or an unfavorable prognosis) in the world/region for pregnant women belonging to risk groups: those suffering from bronchial asthma, COPD, diabetes mellitus, renal and hepatic pathology, 3rd degree obesity, immunodeficiency conditions, system pathology blood, a number of neurological diseases, as well as under the age of 19 years. It is known that the maximum risk of getting moderate to severe influenza occurs in the last – 37–42nd – weeks of pregnancy [11, 12]. It has been noted that specific prevention of influenza does not eliminate the risk of other respiratory viral infections, since the share of ARVI of non-influenza etiology is up to 75% even during influenza epidemic periods [9, 11].
2. Etiotropic - specific antiviral agents: oseltamivir (category C according to the FDA), zanamivir (category C according to the FDA, although there is less experience with use in pregnant women). There is some information about the successful and safe use of a domestic drug with antiviral activity, Arbidol, in pregnant women [13]. If the role of a bacterial pathogen is proven or highly probable, antibacterial drugs are prescribed: in the vast majority of cases, these are penicillins, cephalosporins (all category B) or macrolides (azithromycin or erythromycin - category B) [3, 4]. However, for erythromycin, after analyzing data from the Swedish Medical Register, there was evidence of an increased risk of congenital heart defects and pyloric stenosis [3].
3. Pathogenetic agents. These include interferon-containing drugs, which have a whole range of natural specific antiviral mechanisms. Most interferon-containing drugs are approved for use in pregnant women with caution from the 2nd trimester. Indirectly, this group of drugs will also include interferon inducers. However, there is insufficient information about their safety. Our market has a fairly large selection of such products, but they are usually products of small manufacturers who, unfortunately, do not have the opportunity to conduct full-scale research on their safety and effectiveness. Therefore, such drugs are currently practically absent in Western countries and are not represented in treatment regimens for pregnant women. Taking into account the various manifestations of acute respiratory infections, in relation to a number of them, a number of other groups of drugs will be pathogenetic, for example, mucolytics, bronchodilators, etc. However, these drugs are traditionally considered under the rubric of symptomatic drugs [6, 7, 11].
4. Homeopathic remedies. An ambiguous and little-studied group of drugs in classical medicine and science. The advantage of these drugs is their potential safety: based on the essence of creating homeopathic drugs, the doses of active substances are ultra-low or even zero, which implies the absence of potential toxic effects, as can be the case with the use of classical medicine drugs. Another advantage is the relative cheapness of the funds. The disadvantages are the insufficient evidence base on the effectiveness and safety of these products, unexplained mechanisms of “bioenergetic” effects on the macroorganism. Therefore, these funds require careful further evidence-based study. At the moment, practical medicine has accumulated experience in the use of a number of homeopathic medicines for acute respiratory infections in pregnant women, some of which are registered as “conventional” medicines that are sold in the general pharmacy chain and have some positive experience in clinical use. Such drugs include Stodal, Oscillococcinum, Engystol, Girel and a number of others [14].
5. Herbal remedies. Despite the fact that this is the oldest group of drugs, it is also insufficiently studied from the standpoint of evidence-based medicine. Moreover, recently, in relation to a number of herbal preparations, data have appeared on their obvious or potential danger during pregnancy [3, 15]. Thus, the addition of herbal drugs (especially combined ones) to a standard therapy regimen increases the likelihood of adverse drug interactions. Their safety in general has been studied extremely poorly, and there is virtually no evidence of safety during pregnancy. The WHO database contains several tens of thousands of reports of adverse reactions to herbal products, including several hundred with fatal outcomes. Thus, due to hepatotoxicity, the use of dietary supplements containing kava kava is prohibited in many countries, including Russia. It is possible that many of the plants have carcinogenic properties. And even for the components of such a widely used drug as Canephron, there is an insufficient evidence base for safety: rosemary and lovage have a stimulating effect on the myometrium, and centaury has not been sufficiently studied and is recommended to be avoided [3, 16]. In order to study the effect of drugs (including herbal preparations) on the course and outcomes of pregnancy, Roszdravnadzor and the Federal Center for Monitoring Drug Safety recommend that medical workers report all cases of drug use at any stage of pregnancy, even if their negative effect on the course has not been identified. and gestational outcomes [3]. Thus, at this time, most herbal drugs are considered poorly studied and, therefore, potentially dangerous. It is recommended to limit their use during pregnancy.
6. Symptomatic remedies. This diverse group of drugs for acute respiratory infections during pregnancy most often includes the following subgroups of drugs: antipyretics (NSAIDs), decongestants, mucolytics and mucoregulators, bronchodilators and antitussives. Of the antipyretic drugs, paracetamol is the safest; Ibuprofen, diclofenac and indomethacin are relatively safe in the 1st half of pregnancy. However, it should be remembered that NSAIDs in the 2nd–3rd trimester can contribute to premature closure of the ductus arteriosus and the development of persistent pulmonary hypertension in the fetus; a decrease in the tone, excitability and contractility of the uterus, up to the cessation of labor [17, 18].
Decongestants can be used during pregnancy only if the expected benefit justifies the potential risk to the fetus. However, in practice, they are very often prescribed and even more often used without the consent of a doctor, on their own. Ephedrine, oxymetazoline, phenylephrine, phenylpropanolamine and pseudoephedrine are Category C drugs (i.e., clinical studies have not been conducted, and their side effects on the fetus have been identified in animal experiments). Expert council of Russian specialists consisting of A.S. Lopatina, I.S. Gushchina (Moscow) et al., in a consensus on the treatment of allergic rhinitis, spoke categorically against the prescription of all nasal decongestants to pregnant women at any stage of pregnancy. According to Ukrainian colleagues, it is possible to use minimal doses of drugs if a woman used them systematically before pregnancy (“medicinal rhinitis”) [7, 19]. Based on my experience, I consider children’s forms of oxymetazoline (0.05%), i.e. diluted 10 times compared to adult concentrations, to be the optimal drug. This allows their relatively safe use by those women who cannot refuse this group of drugs.
As a bronchodilator, salbutamol can be used if necessary. And from the 2nd trimester - a drug combined with ipratropium bromide (Berodual) [7, 17].
Most standard antitussive drugs are not recommended or contraindicated during pregnancy (according to domestic sources, due to the presence of codeine and other prohibited components in their composition). Stodal homeopathic syrup is approved for use [17] and quite effective [14 and according to our own data]. It is also possible to use plantain syrup and some breast mixtures (their composition must be clarified) [17]. According to foreign data, in the presence of a persistent cough at any time, the use of dextromethorphan and codeine is acceptable. However, one should remember the risk of dependence on these drugs and the risk of respiratory depression in the newborn when the mother takes codeine [7].
If clinically necessary, it is permissible to use a pulmotropic anti-inflammatory and bronchodilator drug, an H1 receptor blocker - fenspiride [17].
Of the mucolytics and mucoregulators, it is possible to use bromhexine, acetylcysteine and ambroxol, which is used most widely due to its safety profile, availability and effectiveness (according to the instructions, ambroxol is allowed to be taken in the 2nd–3rd trimesters).
In the presence of prolonged bronchitis, based on my own experience, the following combinations can be effective: 1) for an unproductive cough - ambroxol (10–20 days) + acetylcysteine (several days) +/- fenspiride (10–20 days) +/- chest collection (Phytopectol No. 2), herbal or homeopathic syrup (plantain syrup or Stodal - 1-2 weeks); 2) for productive cough – ambroxol (1–2 weeks) +/- chest preparation (Phytopectol No. 1), homeopathic syrup (Stodal – 1–2 weeks). An additional effect can be obtained by including alkaline and/or pine inhalations in the treatment regimen (5–10 sessions).
Own experience of using ambroxol in the treatment of acute respiratory infections in pregnant women.
Purpose
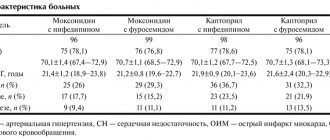
To analyze the effectiveness and safety of prescribing the drug ambroxol in the treatment of acute bronchitis in pregnant women in the 2nd–3rd trimester. Material and methods
The study included 37 pregnant women: from 17 to 39 years old.
The patients were observed by a general practitioner at the perinatal consultation and diagnostic department during 2011–2013. In group 1 (N = 20), the drug Ambrobene produced by Ratiopharm GmbH / Merckle (Germany) was used, 30 mg 3 times a day.
In the control group (N = 17), ambroxol was not used. The treatment also included the use of approved herbal infusions and other herbal preparations, alkaline inhalations, suppositories with interferon, and symptomatic remedies.
Clinical observation of the dynamics of their condition continued for 1.5–3 weeks. The following clinical symptoms and signs were scored: cough, shortness of breath, amount of sputum, sputum viscosity (difficulty of clearing), purulence of sputum, presence of wheezing in the lungs. The severity of subjective parameters was assessed as follows: 0 points – absence of symptom (sign), 1 – slight severity, 2 – moderate, 3 – severe [20. In addition, patients and doctors rated the overall effectiveness of treatment using the same scale. The average integrative indicator for the totality of the evaluated parameters was also calculated [21].
results
In group 1, with the addition of ambroxol to basic therapy, a more rapid regression of clinical symptoms, changes in the nature of sputum and its viscosity, quantity, and positive auscultatory dynamics were noted. In most cases, by the 7th day of treatment, cough, shortness of breath, and wheezing decreased significantly, sputum discharge became easier and its purulence decreased. In group 2, less pronounced dynamics were noted, partly with statistical significance of the differences.
After two weeks of treatment, a significant decrease in the intensity of cough, shortness of breath, purulence of sputum, and the number of wheezing was noted. At the same time, in the control group (group 2), the assessment of cough intensity and sputum viscosity was significantly worse. Both doctors and patients with the same positive dynamics noted the effectiveness of the treatment; statistically significant differences were identified between groups 1 and 2. In group 1, no adverse drug reactions were identified, in group 2, one possible ADR was identified. The initially planned number of patients in group 2 – 25 – was not achieved, because the comparison was stopped early due to significantly better parameters in the main group. The dynamics of changes in the severity of symptoms and parameters are presented in the table.
GENERAL CONCLUSIONS
– inclusion of the drug Ambrobene in the combination therapy regimen for acute respiratory infections in pregnant women significantly reduces the intensity of cough, shortness of breath, the amount, viscosity and purulence of sputum, and the number of wheezing after two weeks of therapy; – statistically significant differences in the presence of cough, quantity, viscosity of sputum, the presence of wheezing in the lungs over time in comparison with the group of patients without the inclusion of Ambrobene in the combination therapy regimen; – statistically significant differences in patients’ subjective assessment of the effectiveness of treatment and improvement over time compared to the group of patients without the inclusion of Ambrobene in the combination therapy regimen; – the presence of various dosage forms of the drug allows you to optimize the treatment regimen depending on the requirements of the clinical situation and modify it if necessary. It is possible to carry out stepwise therapy (start with intravenous administration, switch to tablet form when the condition improves); – Ambrobene is an effective and safe drug in the treatment regimen for acute respiratory infections and acute bronchitis in pregnant women in the 2nd–3rd trimester; – our analysis revealed no side effects when taking Ambrobene.
LITERATURE
1 Darios Getahu, Cade V. Aath, Morga R. Peltier, Joh C. Smulia, Athoy M. Vitzileos Acute ad chroic respiratory diseases i pregacy: Associations with placetal abruption // Am. J. of Obstetrics & Gyecology. Vol. 195.Is. 4. P. 1180–1184. October 2006. 2 Infections in obstetrics and gynecology: A practical guide / ed. prof. VC. Seagulls. Donetsk: Almateo LLC, 2006. 3 Ushakova E.A. / Safety of the use of drugs for infections in pregnant women // Handbook of a polyclinic doctor. 2009. No. 2 (therapeutic department). 4 Eliseeva E.V., Feoktistova Yu.V., Shmykova I.I.. Safety of pharmacotherapy in pregnant women. 3rd ed., revised. and additional Vladivostok: Medicine DV, 2012. 5 Shekhtman M.M. Guide to extragenital pathology in pregnant women. M.: Triad - X, 1999. 6 Extragenital pathology and pregnancy: A practical guide / ed. Z.Sh. Gilyazutdinova. M.: LLC Med Press, 1998. 7 Christoph Schaefer. Drug therapy during pregnancy and lactation: [guideline]. 8 Maly V.P. Flu and pregnancy / V.P. Small // Clinical immunology. Allergology. Infectology. 2009. No. 6/7. pp. 15–17. 9 https://rybelm.ru/akusherstvo/gripp-i-orvi-u-beremeyih 10 Obstetrics: national guide / ed. E.K. Ailamazyan, V.I. Kulakova, V.E. Radzinsky, G.M. Savelyeva. M.: GEOTAR - Media, 2009. (Series “National Guidelines”). 11 Maly V.P., Romantsov M.G., Sologub T.V. Flu: A manual for doctors. St. Petersburg; Kharkov, 2007. 12 www.pamf.org/flu/preg.html - Pregacy ad the Flu (Iflueza) / Palo Alto Medical Foudatio. https://www.pamf.org/flu/preg.html, https://www.pamf.org/flu/highrisk.html 13 https://pharmstd.ru/images/articles/RP_Arbidol%20rmz%2012% 2008.pdf Arbidol is an effective drug for the treatment and prevention of influenza and acute respiratory viral infections: a review of the results of clinical studies by I.A. Leneva T.A. Guskova. 14 Nikiforova G.N., Svistushkin V.M. Possibilities of using complex homeopathic medicines in the treatment and prevention of acute respiratory viral infections // Attending physician. 2012. No. 4. pp. 91–93. URL: https://www.lvrach.ru/2012/04/15435409/ 15 Boie J. Tesch. Herbs commonly used by wome: A evidence-based review // Am. J. of Obstetrics & Gyecology. Vol. 188. Is. 5. Part BP S44–S55. May 2003. 16 ewall C. et al. Herbal Medicines. Lodo, Eglad // Pharmaceutical Press. 1996. No. 67. 17 Directory of drugs RLS. URL: https://www.rlset.ru/ 18 https://www.practica.ru/DrugBook/idex.htm 19 S.M. Chubby. Nasal decongestants - pros and cons // Health of Ukraine. https://health-ua.com/articles/3889.html article published in No. 9/1, April 2009. pp. 32–33. 20 Korzh A.N. Experience of using ambroxol in the treatment of patients with chronic obstructive pulmonary disease // Health of Ukraine. The article was published in No. 23–24, December 2008. pp. 60–61. 21 Enseeva Zh.T. Experience of using ambroxol in the treatment of patients with chronic bronchitis // Bulletin of KazNMU. URL: https://kazmu.kz/press/2011/10/07/
Pregnant woman
The body of a pregnant woman continues to actively prepare for the birth of a baby, the content of estrogen rapidly increases, and the level of progesterone decreases significantly. Changes in hormonal levels help soften the tissues of the birth canal and cervix. Throughout pregnancy, the lumen of the cervical canal is closed by a plug of thick mucus, which protects the baby from infection, and the uterine cavity protects against the penetration of microorganisms hazardous to health. In the last weeks of pregnancy, the consistency of the mucus changes, it becomes more liquid and begins to gradually flow out. In some women, the mucus disappears gradually, while in other women in labor it comes off simultaneously. The discharge resembles colorless egg white in its consistency and appearance. Sometimes the mucus is pinkish, brown or yellow. The removal of the plug is painless; the woman may experience a slight feeling of discomfort in the lower abdomen. The removal of the plug may be signaled by more abundant vaginal discharge than during the entire pregnancy.
A woman should carefully monitor the color and volume of discharge, since too much colorless discharge may indicate not only the passage of the plug, but also be one of the symptoms of leakage of amniotic fluid. Indicator pads and amniotests or test strips will help determine the cause of the discharge. The pads are sold in many pharmacies and can be easily used at home. If leakage of amniotic fluid is confirmed, you should immediately consult a doctor.
After the mucus plug comes off, you should avoid visiting the pool and swimming in open water, as the risk of infection for the child increases significantly. It is also necessary to exclude sexual contact.
39th week of pregnancy: what happens to the fetus?
At the 39th week, the child’s weight reaches 3,100-3,500 g, and his height is 50-52 cm. Height and weight indicators are very relative and can differ significantly. The baby is rapidly preparing for the most important test in his life - birth, which requires endurance and significant effort. During this period of pregnancy, the size and weight of the child’s adrenal glands, that is, the glands of the endocrine system, which are responsible for the human body’s response to stress factors, increase. It is the hormones adrenaline and norepinephrine produced by the adrenal glands that help the child adapt as quickly as possible to new temperature conditions, tactile, sound and light impulses.
All the baby's senses are developed at 39 weeks. Within a few moments after birth, the baby can focus his gaze, he reacts to bright light and moving objects, many scientists claim that newborns distinguish colors and see the faces of parents and doctors. In the last weeks of intrauterine life, the baby's hearing is also fully developed; after birth, he reacts to loud sounds and noise. A newborn baby can identify the basic shades of taste, recognize sour, bitter, sweet and salty.
In the womb, the baby is in an aquatic environment that minimizes contact. Immediately after birth, the baby experiences many tactile sensations; unlike intrauterine life, he feels the touch of his mother’s hands and diapers, towels, dressings and other materials. Babies especially like the touch of skin to skin, so in a modern maternity hospital, newborns are always placed on their mother’s stomach even before the umbilical cord is cut. The child adapts more easily to the new environment and feels protected. Placing the baby out has not only a psychological aspect, since it promotes the colonization of microorganisms from the mother’s skin onto the skin and mucous membranes of the baby, and increases his immunity.
What are the possible concerns?
Corvalol during pregnancy, especially in the early stages, poses a great danger due to the high risk of developing fetal abnormalities. Barbiturates are teratogenic substances that increase the likelihood of nervous system disorders, heart defects, cleft lips and palate, and mental disorders in the unborn baby.
In the second and third trimester, the risk to the fetus decreases, but long-term use of Corvalol is fraught with addiction. It should be remembered that easily penetrating the placental barrier, the medicine can also pass into mother’s milk during breastfeeding. Due to this fact, use during breastfeeding is prohibited.
Pregnant woman
In the last weeks of pregnancy, the expectant mother strives to prepare her apartment or house as much as possible for the arrival of a new family member. Scientists call this sign of impending birth nesting syndrome. Many women observe signs of the syndrome from the thirtieth week of pregnancy, but at the 39-40th week nesting reaches its maximum point. Pregnant women strive to do general cleaning and repairs, re-stick wallpaper and purchase many new things that, in their opinion, are simply necessary in the house. After giving birth, many purchases cause confusion. The reason for this behavior is an increase in the level of adrenaline and norepinephrine in the body. These hormones are produced by the adrenal glands; they are necessary not only for the woman, but also for the baby to prepare for the upcoming birth.
40th week of pregnancy: how is the baby developing?
40 weeks – full-term pregnancy. The weight of a child born at this period ranges from 2,600 g to 4,400 g, and his body length is 48-53 cm. These indicators are very arbitrary, since at 40 weeks miniature babies weighing 2,600 g and real heroes are born, whose body weight approaches 5,000 g. The body length of newborns can also vary from 45 to 55 cm.
Most women give birth at 40 weeks. At this stage, the baby is completely ready for birth; it meets all the parameters of a full-term baby. Before birth, the baby presses its arms and legs closely to the body, bends its head as much as possible and presses against the exit of the uterus. This position makes it possible to pass the birth canal with the narrowest part of the skull. During labor, with each contraction, the child gradually moves downward; he does not move in a straight line, but makes helical-translational movements, as if screwing into the mother’s birth canal. As the newborn moves forward and his head descends completely, the cervix opens completely. This is followed by pushing, that is, contractions of the uterus that move the baby along the birth canal. The baby's head gradually appears, followed by his body. Childbirth is a complex mechanism that is aimed not only at the safe passage of the birth canal by the child, protecting him from accidental injuries due to increased pressure, but also at preventing ruptures of the woman’s soft tissues.
Corvalol: composition, properties, indications for use
This drug is available in two dosage forms: tablets and drops for oral use. Each type of this medication has the same active substances. They differ in composition, appearance, and method of use. Detailed descriptions of Corvalol release forms are presented in the table.
| Release form | Compound | Appearance | Packing |
| Drops | Ethyl ether, phenobarbital, 95% ethyl alcohol, food additive E524, peppermint oil. | Transparent colorless liquid with a pleasant unobtrusive aroma. | The medicine is in glass bottles of 15, 25 and 50 ml, with a plastic screw cap and a dosing device. Bottles with medicine are placed in cardboard boxes. |
| Pills | Peppermint oil, ethyl ether, phenobarbital, stabilizer E459, potato starch, lactose monohydrate, food additive E572, microcrystalline cellulose. | White or almost white pressed powder of round flat shape with beveled edges. | Tablets are packaged in plastic blister packs of 10, 20, 30, 40, 50 and 100 pieces. Blisters are in thick cardboard boxes of 1, 2, 3, 4, 5 and 10 pieces. |
The drug has the following spectrum of therapeutic action:
- calms the nervous system;
- relieves muscle spasms;
- eliminates sleep disorders;
- lowers blood pressure.
Indications for use of Corvalol:
- neurotic conditions;
- cardiopalmus;
- increased irritability and anxiety;
- intestinal and biliary colic;
- pain in the heart area;
- disruption of the process of falling asleep;
- high blood pressure;
- mild forms of arterial hypertension;
- malfunction of the autonomic nervous system.
Pregnant woman
The long wait to meet your unborn child is coming to an end; the 40th week of pregnancy is the last for most women. Every day the expectant mother’s anxiety increases, and the long wait affects her mood and well-being. Women strive to give birth to a child as quickly as possible, so that pregnancy and painful contractions become a thing of the past. Every pregnant woman dreams of meeting her baby, wants to hold him to her breast and stroke his tender head.
Many women, especially first-time mothers, worry that labor will begin unnoticed, but such cases are extremely rare. A woman feels the onset of labor, feels regular contractions that repeat at certain intervals and gradually increase, the time interval between them shortens.
Contractions may be preceded by prenatal rupture of amniotic fluid, which is observed in a certain percentage of women in labor. After the water breaks, contractions may be quite weak or completely absent. Regardless of the intensity of contractions, the release of water is one of the signs of the onset of labor and requires immediate contact with specialists and the woman’s hospitalization in a maternity hospital or hospital, since when the water breaks, the integrity of the bladder is disrupted and the risk of microorganisms dangerous to the baby’s health entering the uterine cavity increases. It is important that after the water breaks, the baby is born within a maximum of 10-12 hours.
A pregnant woman must properly tune in to childbirth, concentrate on the desired result and believe in her own strength, and complete the task intended for her by nature. The right psychological attitude and theoretical knowledge will help a woman become a mother, successfully go through all stages of childbirth and hold the long-awaited child to her heart.