Magnesium deficiency?
Magnesium is among the top most popular dietary supplements. There are at least three reasons for this.
- This metal really plays a very important role in the life of the body. It is needed by mitochondria to produce energy. Neurons - for transmitting electrical impulses. Cell ribosomes - for protein synthesis. With its help, damaged DNA molecules are restored, muscles contract and cholesterol is removed. Magnesium is involved in 500+ intracellular biochemical reactions and activates 300+ enzymes. And at the same time it is not produced inside the body. This means that we depend on its supply from the outside.
- According to frequently cited information, about 30% of Russians receive less than 70% of their daily dose of magnesium. But don't panic! We have found the original epidemiological study and hasten to reassure: it is not about all Russians, but only about 2,000 patients from several clinics.
- Anyone can suspect magnesium deficiency, even if a standard plasma or serum test shows that everything is normal. The catch is that 99% of magnesium is found inside cells (about 60% in bone tissue, the rest in muscles, brain, kidneys and liver), from where it is released into the blood when necessary to maintain optimal concentrations. So a normal level of magnesium in the blood does not exclude its deficiency at the cellular level. Therefore, popular health publications often advise focusing on external signs of deficiency. And there are so many of them (from apathy and high blood pressure to irritability and caries) that making a “diagnosis” is as easy as shelling pears.
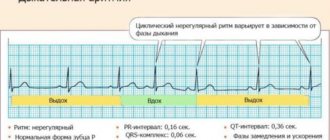
The true diagnosis of magnesium deficiency is a battery of tests, including ECG, myography, bone density testing, saliva, urine, nails and hair analysis. Therefore, even if your legs often cramp, goosebumps appear, or your eyelid twitches (these are the most characteristic signs of magnesium deficiency), only a specialist can determine the real cause.
The role of magnesium in diseases of the cardiovascular system
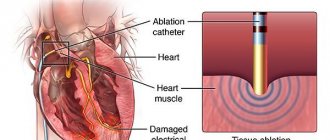
In the human body, the amount of magnesium is approximately 20-28 g - mostly inside the cells themselves, where, along with potassium, it is the second most important mineral. Only 1% of magnesium is found in the blood. It is a macronutrient, a natural calcium antagonist and a regulator of vascular tone, blood pressure and peripheral circulation. Magnesium activates ATPase, an essential enzyme for the functioning of the cell membrane and an energy source for the Na–K pump. Intracellular magnesium deficiency can cause an increase in cellular sodium and calcium content and a decrease in potassium content [1]. Despite the important role of magnesium, its level is rarely determined, although in one study hypomagnesemia was detected in 42% of hospitalized patients, hypermagnesemia in 6% [2]. At the same time, the level of magnesium, like potassium, in the blood serum often remains normal, despite a decrease in its content in the body. In general, neither the serum level nor the determination of intracellular magnesium content gives a true picture of its physiological activity, in contrast to the determination of free magnesium, which is possible using magnetic resonance imaging [3]. However, in clinical practice, only determination of serum magnesium levels is available. Despite the fact that almost all magnesium is found intracellularly in the body, low serum levels correlate with general magnesium deficiency [4]. Conducted epidemiological studies indicate that serum magnesium levels are inversely associated with risk factors for cardiovascular diseases, such as arterial hypertension, type 2 diabetes mellitus, metabolic syndrome, as well as with the presence of coronary heart disease [5]. Other evidence from environmental studies, clinical studies, and autopsies suggests that increasing magnesium levels potentially protects against cardiovascular disease [6]. The physiological role of magnesium in the body Magnesium influences the regulation of biochemical processes in the body through magnesium-containing enzymes and free magnesium ions (being a cofactor in many enzymatic reactions (hydrolysis and transfer of the phosphate group, the functioning of the Na+–K+–ATP pump, Ca2+–ATP pump, proton pump, participates in the exchange of electrolytes, ATP hydrolysis, reduces the uncoupling of oxidation and phosphorylation, regulates glycolysis and the oxidation of fatty acids; participates in protein biosynthesis, transmission of genetic information, synthesis of cyclic AMP and synthesis of nitric oxide in the vascular endothelium).In addition, magnesium is involved in maintaining electrical balance cells (including in the process of depolarization, with a lack of magnesium the cell becomes hyperexcitable).Magnesium has an inhibitory effect on the conduction of nerve impulses, is part of numerous enzymes of nervous and glial tissues, is involved in the processes of synthesis and degradation of neurotransmitters (norepinephrine, acetylcholine), and also in the regulation of neuromuscular activity of conducting tissues of the body (cardiac muscle, skeletal muscles, smooth muscles of internal organs), since it prevents the entry of calcium ions through the presynaptic membrane, which determines the presence of myotropic, antispasmodic and disaggregation effects. This element is a component of the antioxidant system, an important component of the immune system. It inhibits premature involution of the thymus, regulates the phagocytic activity of macrophages, and the interaction of T- and B-lymphocytes. Being next to calcium in the group of the periodic table, magnesium is a calcium antagonist: these two elements easily displace each other from compounds. Magnesium deficiency in a diet rich in calcium causes calcium retention in all tissues, which leads to their calcification [7]. Magnesium enters the body with food (in particular table salt) and water. The intake rate is usually 200–400 mg per day. Plant foods are especially rich in magnesium: legumes and cereals, spinach, salads, nuts. However, the magnesium content in them can vary significantly depending on the growing soil. Water is also an important source, and the harder it is, the higher its magnesium content. In regions with soft water, the incidence of hypomagnesemia is high. Part of the ionized magnesium is split off from the magnesium salts of food in the stomach and absorbed into the blood. The main part of the sparingly soluble magnesium salts passes into the intestines and is absorbed only after they are combined with fatty acids. Up to 40–45% of incoming magnesium is absorbed in the gastrointestinal tract. In human blood, about 50% of magnesium is in a bound state, and the rest is ionized. The concentration of magnesium in human blood is 2.3–4.0 mg. Complex magnesium compounds enter the liver, where they are used for the synthesis of biologically active compounds. The main “depot” of magnesium is in bones and muscles. Magnesium is excreted from the body mainly through urine (50–120 mg) and sweat (5–15 mg). The absorption of magnesium increases with its deficiency in the body. For absorption, a sufficient amount of cofactors must be supplied to the body: lactic, aspartic, orotic acids and vitamin B6. Vitamins B1, B6, C, D, E, calcium, phosphorus (supplied in optimal quantities), protein, estrogens help increase magnesium levels in the body [7]. Magnesium is excreted primarily by the kidneys, also through sweating. The causes of magnesium deficiency may be: • insufficient supply (regions with “soft” water”); • malabsorption in the intestine (dysbacteriosis, chronic duodenitis); • dysregulation of magnesium metabolism; • decreased absorption due to excess phosphates, calcium and lipids; • long-term use of antibiotics (gentamicin), diuretics, antitumor and other pharmacological drugs; • parenteral nutrition; • increased need for magnesium (during pregnancy, during the period of growth and recovery, with chronic alcoholism, excessive sweating); • violation of insulin synthesis; • intoxication with aluminum, beryllium, lead, nickel, cadmium, cobalt and manganese. Magnesium deficiency is the most common type of mineral deficiency in the population in many countries, particularly in the United States. The main manifestations of magnesium deficiency: • fatigue, irritability; • insomnia disorders, dizziness; • loss of appetite, nausea, vomiting, diarrhea, constipation; • cardialgia, palpitations, fluctuations in blood pressure (BP), prolongation of the QT interval; • arrhythmias, vasospasms, muscle weakness, muscle cramps; • immunodeficiencies (possibly increased risk of tumor diseases); • bronchospasm and laryngospasm; • paresthesia, spasms of smooth muscles. Magnesium deficiency, by increasing uterine contractility, can provoke premature birth. Increased magnesium content in the body The main causes of excess magnesium: excess intake; Dysregulation of magnesium metabolism. An increase in magnesium concentration is observed with hyperfunction of the parathyroid glands, thyroid gland, nephrocalcinosis, arthritis, psoriasis, dyslexia (a disorder with impaired understanding of readable text in children). Magnesium salt, when administered orally, even in large doses, does not cause poisoning, but acts only as a laxative. At the same time, with parenteral administration of magnesium sulfate, symptoms of intoxication may be observed in the form of general depression, lethargy and drowsiness. With a significant overdose of magnesium compounds, there may be a risk of poisoning (for example, with antacids). Anesthesia occurs when magnesium concentrations in the blood are 15–18 mg%. The role of magnesium in the pathogenesis of various diseases of the cardiovascular system Coronary heart disease (CHD) It was found that during post-mortem assessment of magnesium content in patients who died from ischemic heart disease, the level of magnesium was lower than in those who died from other causes. Several studies have shown that patients who have suffered a myocardial infarction are significantly more likely to have magnesium deficiency, but it is unknown whether it was a cause or a consequence of the disease [8]. Some, although not all, studies have shown improved survival of patients with myocardial infarction with magnesium therapy [9]. A recently completed study assessing the correlation between magnesium levels and sudden cardiac death found a significant reduction in the risk of sudden cardiac death with increasing serum magnesium levels, independent of other factors such as hypertension, diabetes, potassium levels, heart rate, and history of coronary artery disease. However, no connection has been established between the level of magnesium intake and the risk of sudden cardiac death [10]. However, in relation to arterial hypertension and coronary artery disease, a connection was also previously established with serum magnesium concentration, and not with its consumption [11]. It has been revealed that a reduced magnesium content in drinking water increases the risk of developing cardiovascular diseases (especially coronary heart disease) and sudden death [12]. Atherosclerosis and dyslipidemia There is evidence of a relationship between magnesium deficiency and atherosclerosis. It has been shown that magnesium deficiency is associated with increased levels of total cholesterol, low-density lipids, triglycerides, decreased activity of lecithin-cholesterol-aminotransferase and lipoprotein lipase, and increased activity of SMC-COA reductase [13]. Several animal experiments have shown that supplemental magnesium, even in combination with an atherogenic diet, slowed the progression of atherosclerosis compared with controls, regardless of cholesterol levels. In some studies among patients with hyperlipidemia, a positive significant effect was obtained in reducing the level of total cholesterol and its atherogenic fractions. In addition, several risk factors, such as hypertension, obesity, insulin resistance, have a common denominator - magnesium deficiency. Diabetes Magnesium deficiency is important in the pathogenesis of diabetes for several reasons: many enzymes involved in the process of glycolysis are magnesium-dependent. In both insulin-dependent and non-insulin-dependent diabetes mellitus, magnesium deficiency was detected in the serum, intracellularly, as well as increased urinary excretion [14]. In addition, it was shown that the degree of diabetes control was directly related to the degree of magnesium deficiency, and supplemental magnesium intake was associated with improved diabetes control. However, not all people with diabetes have hypomagnesemia, and the degree of hypomagnesemia varies depending on the type of diabetes and gender [15]. Arterial hypertension Magnesium deficiency may play a role in the pathogenesis of hypertension, another risk factor for coronary heart disease. Magnesium is involved in the activation of the Na–K–ATP pump and also regulates the entry of calcium into the cell. Thus, magnesium deficiency can lead to a decrease in intracellular sodium and calcium content, an increase in total peripheral resistance and vasospasm, as found in experimental studies in animals. A number of studies have found an association with the intake of certain macronutrients, including magnesium, and hypertension [16]. However, the importance of magnesium in the pathogenesis of hypertension is not completely clear, since various studies have reported conflicting results when examining the relationship between intake, excretion, serum magnesium levels and the degree of hypertension. A systematic review concluded that there is currently insufficient evidence to make a definitive judgment on the relationship between magnesium and hypertension [17]. However, for certain categories of patients with hypertension, impaired magnesium metabolism is definitely important. In particular, it has been established that with a family history of hypertension, there is a reduced intracellular magnesium content. In addition, the hypotensive effect of additional magnesium intake was noted in patients with reduced urinary excretion, in contrast to other categories of patients where the hypotensive effect was absent [18]. Patients with high plasma renin levels had reduced plasma magnesium levels and responded better to magnesium supplementation. An inverse relationship has been established between plasma aldosterone and renin levels, indicating that low magnesium levels are associated with increased activity of the renin–angiotensin–aldosterone system [19]. Once satisfactory control of arterial hypertension is achieved, the level of free magnesium is normalized. When taking non-potassium-sparing diuretics for antihypertensive purposes, significant hypomagnesemia also often occurs. Supplemental magnesium helps eliminate it, improving hypertension control [20]. Spasm of the coronary arteries Magnesium can be considered a natural calcium channel blocker, since as a coenzyme it is involved in the movement of calcium into and out of smooth muscle cells. The importance of hypomagnesemia in the development of spasm and the effectiveness of intravenous administration of magnesium in its elimination has been confirmed both in vitro and in vivo experiments. Finally, intravenous administration of magnesium sulfate for vasospastic angina helps to effectively eliminate vasospasm, which once again confirms the importance of magnesium deficiency in the development of coronary spasm [21]. Myocardial infarction The state of magnesium metabolism in the period preceding the development of myocardial infarction is difficult to assess, for obvious reasons: the available data are contradictory. However, it is clearly established that after a myocardial infarction, hypomagnesemia occurs, which persists for up to 6 months. A meta-analysis of several controlled trials showed that with magnesium infusion, the mortality rate in the treatment group was 3.8% compared with the control group, where this figure was 8%. The main effect is the elimination of malignant arrhythmias [22, 25]. Most studies have found a correlation between hypomagnesemia and post-infarction ventricular arrhythmias. Chronic heart failure The development of hypomagnesemia in heart failure is explained by several factors. Due to an increase in the volume of extracellular fluid and the development of secondary hyperaldosteronism, magnesium absorption decreases. In addition, non-potassium-sparing diuretics also promote the excretion of magnesium. In turn, hypomagnesemia aggravates hyperaldosteronism, which leads to fluid retention, can reduce myocardial contractility, and increases vasoconstriction. Hypomagnesemia in combination with hypokalemia contributes to the occurrence of ventricular arrhythmias. However, not all researchers recognize the importance and prevalence of hypomagnesemia in heart failure; it has only been clearly established that active diuretic therapy leads to hypomagnesemia and this occurs in more than half of patients [23]. Arrhythmias Since magnesium is involved in the transport of sodium, potassium and calcium, changes in its concentration affect the exchange of electrolytes and the processes of electrical excitation of the cell. The best known relationship is between hypokalemia and hypomagnesemia. An increase in magnesium levels leads to bradycardia, increased conduction time and suppression of automaticity. Magnesium deficiency, which is often accompanied by hypokalemia, causes prolongation of the QT interval, depression of the ST segment and low-amplitude T waves. Magnesium combines a membrane-stabilizing effect and the properties of a calcium antagonist, reduces the variability of the duration of the QT interval, which is an unfavorable prognostic factor for the development of fatal arrhythmias. In addition, magnesium is able to inhibit sympathetic effects on the heart [24]. The effectiveness of intravenous administration of magnesium in stopping ventricular extrasystole has been identified for a long time, not only in patients with hypokalemia, but also with normal levels of magnesium in plasma. The Framingham study demonstrated the relationship between hypomagnesemia and an increased incidence of ventricular extrasystoles, tachycardia, and ventricular fibrillation. In the PROMISE study, in the group of patients with hypomagnesemia, greater mortality and a higher incidence of ventricular premature beats were noted compared with the group with normal plasma magnesium levels [25]. For many years, magnesium in the form of sulfate has been effectively used in stopping torsade de pointes (TdP), its effect is due to the inhibition of trace depolarizations and shortening the duration of the QT interval [26]. For supraventricular arrhythmias, magnesium infusion often transforms supraventricular tachyarrhythmias (atrial tachycardia, polyfocal atrial tachycardia) into sinus rhythm. Moreover, this category of patients often exhibits hypomagnesemia or concomitant use of loop diuretics, digoxin, aminoglycosides - drugs that promote hypomagnesemia. The mechanism of influence on arrhythmias caused by digitalis intoxication remains unclear. Magnesium can work by blocking potassium or calcium channels or restoring the function of potassium -soda pump. With digitalis intoxication, hypomagnesia is much more common than without it, among patients on therapy with digoxin, hypomagnesia is detected in each fifth. At the same time, the introduction of magnesium is effective both in patients with hypomagnium and with a normal level of magnesium [27]. In general, the results of a randomized multi -centered -controlled double blind study of Magica made it possible to consider magnesium and potassium preparations as a generally accepted European standard in the treatment of arrhythmias in patients against the background of heart glycosides, diuretics, and antiarrhythmics. The antiarrhythmic effect of magnesium drugs manifests itself after 3 weeks. From the onset of treatment, it allows you to reduce the number of ventricular extrasystoles by 12% and the total number of extrasystole by 60–70% [24]. Mitral valve prolapse according to epidemiological studies in patients with mitral valve prolapse, as well as with other congenital dysplasias of connective tissue, magnesium deficiency is detected in almost 2/3 cases, which is associated with impaired collagen synthesis against the background of magnesium deficiency [28]. Conclusion of magnesium deficiency can play a significant role in the pathogenesis of the development of coronary artery disease, some types of arrhythmias and sudden heart death, however, it should use the clinician to use this information in daily practice, remains unclear. Moreover, even with a normal level of magnesium in plasma, the patient may suffer from hypomagnesia. Since many among these patients take diuretics about arterial hypertension or heart failure, in many cases it is advisable to join potassium -saving diuretics to the treatment of magnesium. In a hospital, in patients documented with hypomagnia, magnesium preparations should be used intravenously, intramuscularly or orally depending on the clinical situation [29]. Thus, magnesium preparations play an important role in the conduct of patients with cardiovascular pathology, primarily due to their ability to favorably affect existing risk factors and reduce the risk of cardiovascular diseases at the population level. With a deficiency of magnesium, its additional administration is required at the rate of 10-30 mg per 1 kg of body weight per day for at least 2 months, due to slow saturation of the tissue depot. It is impossible to ensure such an increased income of magnesium only due to changes in the food diet. It is necessary to use magnesium preparations [30]. Magnesium sulfate is used for parenteral administration in urgent situations, in some cases it is also used orally, causing diarrhea. For prolonged treatment with hypomagnesia, magnesium -containing drugs are used: tablet or in the form of a solution. Currently, there are several drugs containing magnesium for replacement therapy: Magnerot, Panangin, Magne B6, magnesium citrate. The first magnesium preparations in their composition had inorganic salts, from which magnesium absorbed no more than 5%, in addition, they often caused diarrhea, since magnesium stimulates intestinal motility. Modern magnesium preparations are much better absorbed and do not cause side effects from the gastrointestinal tract. Magnesium preparations are used combinations with vitamin B6 (which increases digestibility) with potassium, with irrigation. Magnes salt of irrigation acid is poorly soluble in water, so it practically does not have a laxative effect, it is well absorbed. Polyvitamin complexes with minerals are an unsuccessful source of magnesium, since the calcium contained in them prevents the absorption of magnesium. In a laboratory confirmed state of excessive magnesium content in the body, magnesium -containing is canceled and calcium -containing drugs are prescribed. As you accumulate knowledge and additional studies, the range of use of magnesium preparations will no doubt expand significantly. Literature 1. Rardon DP, FISCH C: Electrolytes and the Heart. In the Heart, 7th Edition (Ed. Hurst JW). McGraw - Hill Book Co., New York (1990), 1567 2. Whang R, Ryder KW: Frequency of Hypomagnesemia and Hypermagnesemia: Requested vs. Routine. J Am Med Assoc 263, 3063–3064 (1990) 3 White Re, Hurtle HC: Magnesium Ins in Cardiac Function: Regulator of Ion Channels and Second Messengeers. Biochem Pharmacol 38, 859–867 (1989) 4. Elin RJ: Magnesium metabolism in Health and Disease. In dissease - a - month. (Ed. Bone RC). Year Book Medical Publishers, Inc. (1988). 5. Ma J, Folsom Ar, Melnick SL, et al. Associations of Serum and Dietary Magnesium with Cardiovascular Disease, Hypertension, Diabetes, Insulin, and Carotid Arterial Wall Thickness. Atherosclerosis risk in comunites Study. J Clin Epidemiol. 1995; 48: 927–940. 6. Chakraborti S, Chakraborti T, Mandal M, et al. Protective Role of Magnesium in Cardiovascular Diseases: A Review. Mol Cell Biochem. 2002; 238:163–179. Eisenberg mj. Magnesium Deficiency and Sudden Death. Am heart J. 1992; 124: 544–549. 7. Gorodetsky V.V. Magnesium preparations in medical practice. Small Encyclopedia of magnesium / V.V. Gorodetsky, O. B. Talibov. M.: Medical Practice, 2003. 44 p. 8. Eisenberg mj. Magnesium Deficiency and Sudden Death. Am heart J. 1992; 124: 544–549. 9. Woods K, Fletcher S, Roffe C, et al. Intravenous Magnesium Sulphate in Suste Myocardial Infarction: Results of the Seconder Intravenous Magnesium Intervention Trial (Limit - 2). Lancet. 1992; 339: 1553–1558. 10. James M. Peacock, Phd; Tetsuya Ohira, Serum Magnesium and Risk of Sudden Cardiac Death in the Atherosclerosis Risk in Communities (Aric) Study American Heart Journal. 2010; 160 (3): 464–470. 11. Peacock JM, Folsom Ar, Arnett DK, et al. Relationship of Serum and Dietary Magnesium to Incident Hypertension: The atherosclerosis Risk in Communities (Aric) Study. Ann Epidemiol. 1999; 9: 159–165. 12. Liao F, Folsom Ar, Brancati FL. Is Low Magnesium Concentration a Risk Factor for Coronary Heart Disease? The atherosclerosis risk in communates (Aric) Study. Am heart J. 1998; 136: 480–490. 13. Shechter M. Does Magnesium has a role in the Treatment of Paty Coronary Artery Disease? Am J Cardiovascus Drugs. 2003; 3 (4): 231–239. 14. Ma B., Lawson AB, Liese Ad et al. Dairy, Magnesium, and Calcium Intake in Relation to Insulin Sensitivity: Approaches to Modeling a Dose - Dependent Association. Am. J. Epidemiol. 2006. SEP 1; 164 (5): 449–458. 15. Kao what, folsom ar, nieto fj, et al. Serum and Dietary Magnesium and the Risk for Type 2 Diabetes Mellitus: The Atherosclerosis Risk in Communities Study. Arch Intern Med. 1999; 159: 2151–2159. 16. Peacock JM, Folsom Ar, Arnett DK, et al. Relationship of Serum and Dietary Magnesium to Incident Hypertension: The atherosclerosis Risk in Communities (Aric) Study. Ann Epidemiol. 1999; 9: 159–165. 17. Jeee SH, Miller Er, Guallar E, et al. The Effect of Magnesium Supplementation on Blood Pressure: A Meta - ANALYSIS of RANDOMIZED CLINICAL TRIALAS. Am J Hypertens. 2002; 15: 691–696. 18. Geeijnse J. M, Witteman J. C, Bak A. A, Den Breeijen J. H. H. H. H. H. H. Grobbee de Reduction in Blood Pressure with A Low Sodium, High Potassium, High Magnesium Salt in Older Subjects with Mild to Moderate Hypertension. BMJ. 1994. Aug. 13; 309 (6952): 436–440. 19. Geeijnse J. M, Witteman J. C, Bak A. A, Den Breeijen J. H. H. H. H. H. H. Grobbee de Reduction in Blood Pressure with A Low Sodium, High Potassium, High Magnesium Salt in Older Subejects with Mild to Moderate Hypertension. BMJ. 1994. Aug. 13; 309 (6952): 436–440. 20. Ekmekci O. B, Donma O, Tunker A. Angiotensin - Converting Enzyme and Metals in Untreed Essential Hypertension. Biol. Trace Elem. Res. 2003. Dec; 95 (3): 203–210. 21. Shechter M., Sharir M., Labrador Mj et al. Oral Magnesium Therapy Imprings Endothelial Function in Patients with Coronary Artery Disease. Circulation, Nov. 2000; 102: 2353–2358. 22. Teo kk, yusuf S., collins R. et al. Effects of Intravenous Magnesium in Suspated Acute Myocardial Infarction. OverView of Randomid Trials // Brit. Med. J. 1991. Vol. 303. P. 1499–1503. 23. IEZHITSA in Potassium and Magnesium Deplection in Congestive Heart Failure - Pathophysiology, Consequences and Replenishment. Clin Calcium. 2005. NOV; 15 (11): 123–33. 24. Zehender M., Meinertz T., Just H. Magnesium Deficiency and Magnesium Substition. Effect on Ventricular Cardiac Arrhythmias of Various Etiology. Herz. 1997 Jun; 22 SUPPL 1: 56–62. 25. Shilov A.M. et al. The use of magnesium preparations for the prevention of heart rhythm disorders in patients with acute myocardial infarction // Ros. cardiol. Journal 2002. No. 1. S. 16–19. 26. Hoshino K., Ogawa K., Hishitani T. et al. Successful Uses of Magnesium Sulfate for Torsades de Pointes In Children with Long Qt Syndrome. Pediatr. Int. 2006. APR; 48 (2): 112–117. 27. SUETA CA, Clarke SW, Dunlap SH Effect of Acute Magnesium Administration on the Frequency of Ventricular Arryhythmia in Paty Heart Failure. Circulation, Feb. 1994; 89: 660–666. 28. Durlach J. Primary Mitral Valve Prolapse: A Clinical Form of Primary Magnesium Deficit / J. Durlach // Magnes. Res. 1994; 7: 339–340. 29. Ueshima K. Magnesium and Ischemic Heart Disease: A Review of Epidemiological, Experimental, and Clinical Evidences. Magnes Res. 2005 Dec; 18 (4): 275–84. 30. Lazubnik L. B., Drozdova S. L. Correction of magnesium deficiency in cardiovascular pathology // Cardiology. 1997. No. 5. S. 103–104.
Magnesium as a medicine
The logic of using magnesium in medicine is based on two principles.
- If you have a deficiency, it must be replenished to eliminate the risk of complications.
- Since magnesium is necessary to perform certain functions, it means that if they are impaired, it can be useful, even if there is no obvious or severe deficiency.
There are no questions about the first principle. A number of studies show that taking magnesium in case of deficiency actually reduces the risk of complications, such as heart attack - sometimes by more than a third (,). The second principle is more difficult.
If we assume that magnesium is involved in biochemical processes that affect dozens of vital functions, it can be prescribed for almost any disease - like vitamins. Therefore, magnesium supplements are often taken “just in case” for conditions as diverse as osteoporosis, chronic fatigue syndrome, and even mental disorders, including depression. But at the same time, patients, especially those suffering from serious diseases, are never treated with magnesium alone. This means that without a placebo-controlled study it is impossible to understand what exactly produced the therapeutic effect. And there are too few such studies to draw clear conclusions. In this situation, the most reliable criterion is the practical experience of medical specialists. To get first-hand information on the most proven uses of magnesium, we turned to several experts.
Cardiovascular diseases
As an electrolyte (conductor of electrical signals), magnesium plays an important role in the functioning of the cardiovascular system. For example, if there are fewer magnesium ions in the heart cells, the electrolyte balance is disrupted. This is often observed with arrhythmia and acute coronary insufficiency. Therefore, magnesium sulfate injections are actually used in intensive care when cardiac arrhythmias are life-threatening.
It is believed that magnesium generally has a beneficial effect on blood pressure. A meta-analysis of 11 placebo-controlled studies found that taking magnesium supplements did reduce blood pressure in people with chronic diseases, although only slightly: systolic by an average of 4 mm and distolic by 2 mm. Previously, magnesium injections were also given during hypertensive crises (a sharp increase in blood pressure), says cardiologist Anton Rodionov. But in fact, there is no point in using them for hypertension, because a “rebound” follows a decrease in pressure. Experiments on the use of magnesium injections in the treatment of acute heart attack also yielded conflicting results. One study found a 16% reduction in mortality. And the other two did not confirm this effect (,).
But with additives everything is more or less clear. “Dietary supplements with magnesium, in principle, cannot serve as medicines for cardiovascular pathologies,” says cardiologist and cardiovascular surgeon Alexey Utin. Anton Rodionov shares the same opinion: “Popular and widely sold drugs containing magnesium (panangin, asparkam) have neither an evidence base nor clinical meaning.”
Headache and migraine
One of the signs of magnesium deficiency is headaches and migraines. But does taking it help relieve headaches? “If everything were so simple, we would have defeated migraine a long time ago,” says Daria Korobkova, a neurologist at the University Headache Clinic. “Migraine is associated with the malfunction of pain neurons, its course depends on a colossal number of factors, and magnesium is only one brick in this multicomponent scheme.” There are several small placebo-controlled studies showing the effectiveness of magnesium in migraine prevention. Therefore, the American Migraine Foundation recommends taking 400–500 mg of magnesium oxide per day for this purpose. According to Daria Korobkova, she also often recommends magnesium preparations as an additional remedy to her patients suffering from episodic and menstrual migraines (it was precisely these subjects who participated in clinical studies of magnesium). In her experience, in such cases magnesium “works well,” but she cannot call its effectiveness high.
Diabetes
Not all people with type 2 diabetes suffer from magnesium deficiency, and magnesium deficiency does not always lead to diabetes. However, there is clearly a connection between these two conditions. Magnesium is involved in the processing of glucose, and its deficiency reduces the sensitivity of cellular receptors to insulin. Because of this, cells lose the ability to absorb sugar from the blood in the required volume. In addition, with type 2 diabetes, kidney function is often impaired, so too much magnesium is excreted from the body along with fluid. This is a theory. What about practice?
Attempts to use magnesium in the treatment of diabetes have yielded conflicting results, says endocrinologist Denis Lebedev. Although the subjects' blood sugar levels decreased after taking the drugs, a test for glycated hemoglobin (a key indicator for diabetes control) did not reveal statistically significant changes. The authors of the meta-analysis came to the same conclusion, summarizing all studies on this topic over the past six years, included in the largest scientific databases. Taking microelements and vitamins is justified in old age and with dietary restrictions, says Denis Lebedev. But not all diabetic patients need magnesium supplements. They are not prescribed on a regular basis.
Muscle spasms
Taking magnesium is the first thought that arises when your leg muscles cramp at night. And in cases where seizures are caused by excessive physical activity, and not by neurological diseases and age-related problems, this really has an effect - this is the conclusion made by the authors of the authoritative Cochrane review. Another thing is that, according to a special controlled study, this is more of a placebo effect. If you've ever suffered from calf muscle cramps and found relief from taking a magnesium supplement, you may find this hard to believe. But chiropractor and muscle pain expert Paul Ingram reminds us that we have no reason to expect that increasing blood magnesium levels will benefit muscles. Because we simply “don’t know how it works.”
Sleep disorders
Low magnesium levels are correlated with insomnia. This is the only concrete argument in favor of taking magnesium for sleep disorders. Because the biology of the interaction of magnesium with the sleep mechanism has been little studied. And studies of practical application give conflicting results. The authors of one major review even suggest that magnesium supplements are prescribed simply because they are much cheaper than sleeping pills. But there are exceptions. In one small placebo-controlled study, subjects' sleep quality improved by as much as 75 to 85% over 4 to 6 weeks. At least in their own opinion.
Alexey Moskalev, head of the laboratory of genetics of life expectancy and aging, also believes that magnesium in the form of citrate, malate or taurate has a calming effect before bedtime. Neuroscientist and science podcast author Andrew Huberman agrees. True, he himself prefers magnesium L-threonate, which more effectively overcomes the blood-brain barrier, that is, it more actively penetrates from blood plasma into brain tissue. “200–400 mg approximately 30 minutes before bedtime has a powerful hypnotic effect,” says the scientist. But at the same time he emphasizes that people with cardiovascular diseases should consult a doctor before such experiments.
Magnelis B6
Magnesium is involved in ensuring the most important biochemical and physiological processes in the body, affects energy, plastic, electrolyte metabolism, and is involved in the work of about 300 enzymes. Magnesium deficiency increases the risk of developing cardiovascular, neurological, gastroenterological diseases, and diabetes. Frequent manifestations of Magnesium deficiency are: irritability, anxiety, chronic fatigue, sleep disturbances, headaches, spasms and muscle pain.
A good supply of Magnesium to the body protects it from destructive stress. In just 10 minutes of stress, the daily requirement of Magnesium is burned. And in pregnant women, Magnesium deficiency aggravates the risk of miscarriage, therefore magnesium and vitamin B6 preparations are widely used in obstetric and gynecological practice (in the complex therapy of miscarriage, for the prevention of preeclampsia).
- Magnelis B6 contains a complex of Magnesium lactate and vitamin B6, which ensures their easy absorption.
- Vitamin B6 increases the absorption of Magnesium in the intestines, improves its entry into cells and accumulation in them.
Magnesium is involved in the activation of pyridoxine in the liver.
Composition: Magnesium lactate 470 mg (equivalent to magnesium content 48 mg) + pyridoxine 5 mg
Indications for use
established magnesium deficiency, isolated or associated with other deficiency conditions.
Question answer
Is it possible to take magnesium supplement (Magnelis B6) during pregnancy?
According to the instructions for medical use, pregnancy is not a contraindication to the use of magnesium preparations. The decision on the duration of taking a drug containing magnesium lactate 470 mg and pyridoxine hydrochloride 5 mg should be made by the attending obstetrician-gynecologist based on an assessment of your condition (for example, if there is increased uterine tone in the early stages of pregnancy, higher doses are usually prescribed than in later stages , if magnesium preparations are prescribed to prevent gestosis).
I am pregnant, and the gynecologist prescribed me a magnesium supplement. Magnesium is known to relieve spasms, does this affect overall blood pressure? Is it possible to use magnesium with initially low blood pressure if it was prescribed by a gynecologist?
Magnesium does not have a direct hypotensive effect, so it is not contraindicated in the presence of low blood pressure. The need to take magnesium or other medications should be decided by the attending physician, obstetrician-gynecologist and therapist after additional examination.
During pregnancy I have been experiencing leg cramps. Is this related to magnesium deficiency?
Clinical manifestations of magnesium are often increased anxiety, irritability, increased uterine tone, leg cramps, sleep disturbances and many others. The phenomenon you describe may be due to magnesium deficiency, and taking magnesium supplements can help eliminate it. The question of the advisability of using magnesium preparations and dosages can be decided by your attending physician.
Hello. Will a magnesium supplement help you carry out a pregnancy? The last 2 pregnancies ended in birth at 36 and 38 weeks.
Due to the fact that magnesium is involved in the regulation of neuromuscular transmission, taking magnesium preparations helps normalize muscle tone, including magnesium preparations used for increased uterine tone. However, in the later stages of pregnancy, the use of complex therapy is indicated to prevent premature birth, and in some cases hospitalization in a hospital is indicated. In each case, the prescription of therapy is individual, so I recommend that you discuss this issue again with your obstetrician-gynecologist.
Good afternoon The period is 23 weeks, from the first weeks I have been taking Magnelis B6. Now I wanted to start taking calcium. They say it doesn't mix well with magnesium. At what interval is it better to take these drugs?
To avoid interactions between calcium and magnesium preparations, it is advisable to maintain an interval between their doses of at least 6 hours; the optimal regimen is the following: magnesium preparations in the morning, and calcium preparations in the evening, before bedtime.
Can I take magnesium supplements during lactation?
According to the instructions for medical use of the drug Magnelis B6, magnesium passes into breast milk, so use of the drug should be avoided during lactation and breastfeeding.
Is there a need for a time interval between taking Magnelis and taking iron supplements?
To avoid interactions between iron and magnesium preparations (Magnelis B6), it is advisable to maintain an interval between their doses of at least 2 hours.
How can an overdose of magnesium affect the condition of the fetus?
Magnesium supplements during pregnancy are prescribed by your doctor. When prescribing them, the clinical manifestations of a deficiency of this microelement and the characteristics of the course of your pregnancy should be taken into account, which allows you to avoid an overdose of magnesium. Typically, magnesium preparations are prescribed in prophylactic or therapeutic doses that do not exceed the daily requirement for magnesium (it is 400 mg, and increases significantly during pregnancy).
The new formula Magnelis® B6 forte (Magnesium + Vitamin B6) contains 2 times more magnesium and vitamin B61.
- The first Russian analogue of the French drug with the highest concentration of Magnesium + B6!2
- The only 3 large package No. 60*! It lasts a long time!
- Affordable price!
The optimal formula for better absorption of the mineral and convenient administration!
Compound
Magnesium citrate 618.43 mg (equivalent to magnesium content 100 mg) + pyridoxine 10 mg.
Indications
established magnesium deficiency, isolated or associated with other deficiency conditions, accompanied by symptoms such as increased irritability, minor sleep disturbances, gastrointestinal cramps, rapid heartbeat, increased fatigue, pain and muscle spasms, tingling sensation in the muscles. If after a month of treatment there is no improvement in the symptoms of magnesium deficiency, continuing treatment is not advisable.
Nutritional supplements
Magnesium supplements come in the form of tablets, powder, solutions, capsules, and even chewing gum. But in this case, it is not the form that is important, but the content.
Dosage.
The recommended daily dose of magnesium is 300 mg for women and 400 mg for men. But there is an important nuance: the more magnesium enters the body at a time, the worse it is absorbed in the intestines. Therefore, it is better to take it several times a day in small portions.
Compound.
Which supplement to choose is also not just a matter of convenience. Due to the high chemical activity of magnesium, there is no point in taking it in its pure form. (Except for the laxative effect: it absorbs water, diluting the contents of the intestines.) Therefore, it is commercially available in the form of compounds with other substances, mainly organic acids. According to the principle of action, these compounds do not differ from each other. The active ingredient in them is the same. Their job is simply to deliver magnesium to the small intestine, where it is absorbed into the blood. And everyone copes with this task. But how much magnesium gets from the intestines into the blood depends on the size and chemical properties of the molecules with which it is combined. And the additives differ in this parameter. Here is a rating of dietary supplements based on the degree of magnesium absorption.
Magnesium gluconate ⭐️⭐️⭐️
Used in medicine for magnesium deficiency. In online stores it is sold under the names Mag-G, Magonate, Magonate Natal, Magtrate. May cause nausea and diarrhea.
Magnesium Orotate ⭐️⭐️⭐️
Magnesium salt of orotic acid. Magnesium content is just over 3%.
Magnesium malate ⭐️⭐️
Magnesium salt of malic acid. Magnesium content is about 7%.
Magnesium Citrate ⭐️⭐️
The most popular form is magnesium with citric acid. Magnesium content - 5%.
Magnesium L-threonate ⭐️⭐️
Magnesium salt of threonic acid. The patented formula is Magtein, specially designed to facilitate the penetration of magnesium from the blood into the brain tissue. Magnesium content is about 3%.
Magnesium Taurat ⭐️⭐️
Compound with taurine molecule. Magnesium content is less than 4%.
Magnesium oxide ⭐️
Binding of magnesium and oxygen. The low level of bioavailability is compensated by the highest concentration of magnesium among dietary supplements - 50%. More often than other supplements, it causes side effects - nausea, stomach cramps and diarrhea.
The absorption of magnesium into the blood from the small intestine can be interfered with by iron, zinc and phosphorus, as well as oxalic acid, which is abundant in spinach and cabbage. Magnesium also has a difficult relationship with calcium, which is also absorbed in the small intestine and there competes with it for its place in the sun. But vitamin D, on the contrary, is friendly with magnesium and enhances its absorption.
Magnesium is the main anti-stress macronutrient!
Murzaeva Irina Yurievna
Endocrinologist, Preventive medicine
March 13, 2018
Not so long ago, I began to get involved in the problems of violations of the most important micro (macro) elements in the human body , and it all started with a search for the causes of autoimmune thyroiditis and the reasons for its prevalence, with a textbook on micro element violations in AIT, then the topic began to expand in search of the causes of “massive hair loss ", including in children, searching for the causes of frequent acute respiratory viral infections in children... more to come. It turned out that the violation of the microelement composition of the human body is a huge science and more than one Russian scientist is engaged in this, but this topic is poorly covered and there is little literature where you can familiarize yourself with it:!: But whoever searches will always find.
Today we start talking about the most important microelements and macroelements for humans.
Magnesium is a mineral that is now actively discussed and advertised ... “magnesium for stress”, “magnesium for irritability”, “magnesium for arimagnesium for seizures” “magnesium for uterine hypertonicity during pregnancy”, etc. MagneB6 and Magnelis are perhaps the most famous magnesium preparations. But this is just the tip of the iceberg, magnesium is not so simple...)
Magnesium is involved in more than 300 enzymatic processes in the body; magnesium, along with sodium and potassium, is a vital macroelement (not even a microelement  ).
).
There is only 24 grams of magnesium in the body (this is not much), but without it, it is not possible to conduct a nerve impulse along nerve fibers, or contract the heart, or contract muscles, or regulate blood pressure; without it, blood coagulation is disrupted, appetite is disrupted, there can be nausea and vomiting and other disorders. A separate book has been written about magnesium; it is a serious scientific work, 800 pages long, entitled “Magnesium and the Diseases of Civilization.” In this article I will not cover all the most important “points of application” of magnesium in the body, sometime later, I’d rather talk about its practical application...
Magnesium is a mineral that is difficult to “accumulate” in the body, it is consumed extremely quickly, and the more stress, the more pronounced the magnesium deficiency... But not all magnesium preparations can successfully replenish its deficiency.... For its absorption and for the best effect in a given situation, it is important to understand what magnesium is “connected” with. I’ll explain in more detail... In order to enter the body, magnesium must be “in the composition” of salt or some organic compound, and the effect of magnesium and digestibility will depend on the nature of “this conductor - salt or organic matter”.
Now about magnesium absorption: Magnesium can exist in the following 15 forms −
magnesium citrate, magnesium malate, magnesium glycinate and bisglycinate, magnesium threonate, magnesium carbonate, magnesium lactate, magnesium taurate, magnesium chloride, magnesium orotate. magnesium sulfate, magnesium chelate, magnesium oxide, glutamate and magnesium aspartate.
And now I’ll decipher:
Magnesium citrate is a magnesium salt of citric acid, the most digestible form of magnesium, used in most well-known drugs - MagneB6 and Magnelis, magnesium citrate solgar, etc., is used more often as an antispasmodic, relieves spasms of the gastrointestinal tract, that is, relieves constipation and impaired bile secretion, good in gastroenterology.
Magnesium malate is a magnesium salt of malic acid that relieves hypomagnesium muscle cramps, relieves fatigue and aluminum intoxication in the body.
Magnesium threonate - in combination with threonic acid, in studies improves long-term and short-term memory, better than magnesium citrate
Magnesium taurate is a non-toxic form of magnesium, very bioavailable, good to use for insulin and leptin resistance, that is, it reduces cravings for overeating sweets and “night gluttons.”
Magnesium oxide - can only be used in cases of reducing high stomach acidity; in other cases it causes severe osmotic diarrhea. Therefore, it is good for constipation.
Magnesium chloride - used primarily as bath salts with a calming effect on the nervous system, but more on that later.
Magnesium orotate is a compound of magnesium with orotic acid, has a predominant effect on the heart muscle, is used for rhythm disturbances and congenital heart disease such as mitral valve prolapse.
Magnesium sulfate - combined with sulfuric acid, used in bath salts (in this form it is practically irreplaceable), in “famous” intravenous injections, mainly to relieve hypertensive crises.
Magnesium aspartate and glutamate - it is better not to use, they belong to the class of endotoxins.
Magnesium glycinate and bisglycinate are a good form of magnesium, mixed with glycine, good for chronic fatigue syndrome and pelvic pain, good because it does not cause a laxative effect.
Magnesium lactate is an artificially synthesized, inexpensive form of magnesium, has a general strengthening effect, as an excipient it is used in most magnesium preparations as an integral part.
Magnesium carbonate - also used for increased stomach acidity, neutralizes the effect of NSAIDs, good for GERD, not for phenylketonuria.
Magnesium chelate is a form of magnesium immersed in an amino acid, facilitating bioavailability. The absorption of the chelate and, accordingly, magnesium from it is 90% , it does not change the acidity of the stomach, unlike forms combined with acids - therefore it is suitable for everyone, but accordingly it is less effective for constipation and other gastrointestinal dyskinesias, but is rarely found in retail sales and is expensive form of magnesium.
Magnesium is in close relationship with calcium, vitamins K2 and D3. The balance of these four elements will help maintain health without complications.
Only for thyroid function, magnesium has a less significant effect than selenium, iodine and iron, for example.
Now about my favorite form of magnesium...... If you don’t want to swallow pills, you don’t need a laxative effect, and your nerves are “on edge and you can’t sleep,” it wouldn’t be a bad idea to carry out an Anti-Stress or Detoxification program—your ideal option—English baths salt, or, simply put, baths with magnesium sulfate 0.5-1 kg of salt per 1 bath and within the first 15 minutes “you will start to fall asleep in the bath.”
Below are questionnaires by which you can determine magnesium deficiency in an adult and a child.
Transdermal magnesium
Despite all the efforts of manufacturers, the bioavailability of magnesium from dietary supplements remains quite low. Hence the idea of delivering it to the body in other ways. For example, through the skin.
Creams and sprays
And also gels, soaps, oils and lotions, mainly with magnesium chloride (it has the second highest concentration of magnesium after oxide - 30%). American naturopath Norman Shealy was the first to speak about their effectiveness. In 2005, he published a comparison table that showed that by rubbing magnesium cream into the skin, you can correct the deficiency much faster than using nutritional supplements (in a month and a half, rather than in six months). It is this research that is usually meant when it is repeated like a mantra that magnesium is absorbed better through the skin. The problem is that there is no study - only a short abstract with conclusions is available. But several screening tests with animals and people did not confirm them. Apparently, the author rubbed in not only magnesium. So a large review of current research on this topic does not recommend transdermal use.
Magnesium baths
This practice dates back to the 18th century, when a resort with unusual mineral water opened in the English town of Epsom - a natural solution of Epsom salts (magnesium sulfate). Now this mixture is credited with various healing properties: it helps to relax and lose weight, relieves pain, and among the most toxic, it “removes toxins.” But initially it was believed that it simply had a laxative effect, which is closer to the truth: taking capsules or tablets with magnesium sulfate sometimes causes diarrhea.
The only study on the effects of magnesium baths was conducted in England, involving 19 students at the University of Birmingham. They lay in a solution of magnesium sulfate (1 g/100 ml) for 12 minutes a day at temperatures up to 55 degrees. At the end of the study, the majority of subjects had increased magnesium concentrations in their blood, although only slightly. This did not affect their health in any way. But questions remain.
Magnesium molecules are small enough to penetrate the skin barrier. Magnesium ions labeled with fluorescent markers actually penetrate into the top layer of the skin, using the openings of the hair follicles as a loophole. But for the cellular absorption of magnesium, special transport channels are needed, and they are not present in the skin. How could magnesium get into the blood of students? There are several assumptions. The first is boring, but the most plausible: through the lungs with steam. The second is much more fun: thanks to the absorption of magnesium ions by the mucous membrane of the anus. In the same way, the body could absorb alcohol from a hot bath. But, as Paul Ingram rightly notes, if you really want to take magnesium (or alcohol), then it’s more pleasant and easier to do it by mouth.
The importance of magnesium in the body.
The human body contains about 760 mg of magnesium at birth, approximately 5 g at 4-5 months of age and almost 25 g at adulthood. At the same time, 30-40% of the magnesium contained in the body is found in muscles and soft tissues, 1% is found in extracellular fluid, and the rest is found in bone tissue. The importance of magnesium is difficult to overestimate. Thus, almost all chemical processes in the body require the participation of enzymes. An enzyme system basically consists of 3 components: a specific protein molecule (the enzyme itself), a smaller molecule (usually a vitamin such as pyridoxine or vitamin B6) and a positively charged metal ion such as zinc, copper, manganese or magnesium. Magnesium is the second most abundant intracellular cation after potassium and serves as a cofactor for more than 300 enzyme reactions, including energy metabolism, protein and nucleic acid synthesis. From all of the above, we can conclude that magnesium is a vital element, the lack of which can cause serious disruptions to the functioning of the body. In this article we will try to describe the nosological forms of cardiovascular diseases (CVD) that are associated with magnesium deficiency.
Magnesium and atherosclerosis.
There is compelling evidence that extracellular magnesium concentration plays an important role in regulating endothelial cell activity [1]. Indeed, magnesium levels influence the synthesis of nitric oxide [2], the release of intracellular calcium [1], the uptake and metabolism of low-density lipoproteins [3], the degree of membrane permeability to water and albumin [4], and the proliferation of endothelial cells [5]. In addition, magnesium deficiency enhances the cytotoxic effect of free radicals in endothelial cells [6]. Since endothelial cells play an important role in atherogenesis [7], it can be assumed that magnesium influences the mechanisms of atherosclerosis development. J. Maier et al. [8] in their study in 2004 proved that the inhibition of endothelial cell growth that occurs with magnesium deficiency ceases when its normal level is restored, thus indicating that no irreversible changes occur with magnesium deficiency. Most likely, stimulation of cell growth occurs due to the effect of intracellular magnesium, which catalyzes reactions necessary for the process of proliferation of endothelial cells. Since magnesium acts as a natural calcium antagonist, it can also be assumed that the balance between these two ions also affects cell growth processes.
Data from other studies also indicate the direct participation of magnesium in the pathogenesis of CVD in general and atherogenesis in particular. For example, the consumption of water enriched with magnesium ions simultaneously with a high-cholesterol diet by mice with a reduced level of apolipoprotein (which has a strong anti-atherosclerotic effect) led to the inhibition of atherogenesis [9].
At the same time, oral magnesium supplementation is associated with a significant improvement in endothelial function in patients with coronary insufficiency [10]. According to the ARIC study (Atherosclerosis Risk in Communities Study), a high risk of developing coronary insufficiency is observed in patients with low serum magnesium levels, even taking into account traditional risk factors for coronary insufficiency [11].
In cultured endothelial cells, a low concentration of magnesium increases the adhesion of monocytes to them, since the vascular cell adhesion molecule (VCAM) is activated. Under these conditions, the activity of plasminogen activator inhibitor-1 (PAI-1) is also suppressed, the level of pro-inflammatory cytokines (interleukin 3 IL-1α) increases, endothelial proliferation worsens and cell aging occurs [12, 13]. A study conducted on mice with hereditary hypomagnesemia (MgL mice, hypomagnesemia in mice) indicated a significant decrease in endothelial function [14].
In support of the results obtained in cultured cells, MgL aorta also showed higher expression of VCAM and PAI-1 than controls [14].
Magnesium and arterial hypertension (AH).
The inverse correlation between magnesium levels (serum and/or tissue) and blood pressure (BP) levels has long been known. In addition, the relationship between the renin-angiotensin system (RAS), magnesium and blood pressure has been described. Patients with hypertension and high plasma renin activity (PRA) have lower serum magnesium concentrations than those with normal blood pressure [15]; thus, serum magnesium concentration is inversely related to ARP. Since an increase in ARP indicates activation of the RAS, it is possible that angiotensin II-dependent hypertension is, at least in part, due to the consequences of hypomagnesemia.
Earlier studies measured total magnesium ion levels, which did not always reflect a reliable relationship between intra- and extracellular magnesium. Currently, thanks to fluorescent methods for determining the concentration of Mg2+ and Mg2+-specific electrodes, it has become possible to study the content of magnesium ions directly in living cells. Moreover, according to modern analytical data, a significantly reduced concentration of magnesium ions is determined in the cells of many types of patients with hypertension, even if the level of total magnesium is within normal limits [16]. The main reasons for changes in magnesium metabolism in hypertension are unclear; most likely, genetic, dietary and hormonal factors, as well as drug therapy, play a significant role.
Not all clinical studies support a decrease in magnesium levels in hypertension. Some studies have shown no changes in magnesium levels in patients with hypertension compared with those with normal blood pressure [17], while others even indicate an increase in the concentration of Mg2+ in erythrocytes in patients with essential hypertension [18]. Moreover, several epidemiological studies have failed to detect an association between magnesium intake and blood pressure [19]. It follows from this that not all patients with hypertension have magnesium deficiency, just as not all people with magnesium deficiency are patients with hypertension. Despite conflicting views on the role of magnesium in the development of hypertension, there are subgroups of patients with hypertension who always have impaired magnesium metabolism.
These include African Americans, overweight patients, patients with insulin resistance, hypertriglyceridemia, and patients with severe or malignant forms of hypertension [20].
Heart failure (HF).
C. Adamopoulos [21] et al. in their work indicate that serum magnesium levels ≤2 mEq/L increase the risk of death in patients with chronic heart failure (CHF). This is one of the first studies to examine the long-term effect of low magnesium levels on mortality and hospitalization among patients with heart failure. According to this work, hypomagnesemia is directly associated with cardiovascular mortality, but not with hospitalization for heart disease. The authors hypothesize that magnesium deficiency is associated with sudden cardiac death and life-threatening arrhythmias [22–24]. In addition, hypomagnesemia can cause myocardial fibrosis and increase platelet aggregation, which also affects cardiovascular mortality [25, 26]. Finally, low serum magnesium levels may be a marker of HF progression. Aldosterone, a neurohormone whose activity increases in heart failure, increases urinary magnesium excretion, thereby causing hypomagnesemia [27].
In addition, medications taken by patients with HF have an effect on magnesium levels. Diuretics used for CHF have different effects on the level of magnesium excretion in the urine. Because renal reabsorption of magnesium occurs in the loop of Henle, furosemide and other loop diuretics cause significant losses of magnesium in the urine. Thiazide diuretics, by inhibiting the reabsorption of magnesium in other areas, also cause hypomagnesemia, but to a lesser extent than furosemide. At the same time, spironolactone, amiloride and triamterene reduce urinary magnesium loss [28]. Regarding the effect of angiotensin-converting enzyme (ACE) inhibitors on the level of magnesium in the blood, there is a version according to which patients with higher doses of ACE inhibitors have reduced RAS activity, which has a beneficial effect on the level of magnesium in the blood.
Based on the foregoing, we can conclude that in patients with CHF it may be advisable to study the level of magnesium in the blood, and in case of its deficiency, taking oral medications containing magnesium and/or aldosterone inhibitors should improve the prognosis.
Conclusion
The modern Western diet contributes to an insufficient intake of magnesium from food, since preference is given to high-calorie foods that are poor in microelements, and magnesium salts, which cause increased “hardness” of water, are removed from water. Oral administration of magnesium preparations to replenish its deficiency may be useful in a number of pathologies, including hypertension, coronary heart disease, coronary insufficiency, cardiac arrhythmias, as well as chronic fatigue syndrome, many types of musculoskeletal disorders, epilepsy, bronchial asthma, panic disorders and many other organic and mental pathologies. However, in practice, magnesium-containing supplements are extremely rarely prescribed by doctors, which indicates an underestimation of the importance of this element. Until recently, interest in magnesium in traditional medicine was observed only among obstetricians, who used magnesium sulfate to relieve hypertension, preeclampsia and eclampsia in pregnant women. Recently, interest in the behavior of magnesium has spread to doctors in other specialties. Of course, magnesium cannot be treated as a miracle cure that can solve all the problems in modern medicine at once. Thus, S. Patrick et al. [29] in their study put an end to the assumption that intravenous administration of magnesium into the coronary vessels significantly reduces mortality during an acute heart attack. It may be more correct to raise the question of preventive correction of magnesium deficiency in the development of CVD with the use of oral organic magnesium salts, such as magnesium citrate, magnesium pidolate and magnesium lactate, especially in combination with pyridoxine as a magnesium protector. A multicentre observational study of 2000 patients found that insufficient magnesium levels corresponded to a significantly increased risk of the following conditions: R56.8. Convulsions; I63.0. Ischemic cerebral infarction; I10. Essential primary hypertension; I34.1. Mitral valve prolapse; F43.0. Acute reaction to stress; I20.0. Unstable angina; I47.9. Paroxysmal tachycardia, unspecified, etc. [30]. The advantages of magnesium citrate and pidolate compared not only with inorganic salts, but also with some organic salts (orotate, gluconate) are a higher content of elemental magnesium, better bioavailability, especially in combination with pyridoxine. Citrate is an ideal, fully utilized carrier of magnesium into the cell. There are no magic substances or drugs, just as there are no cures for all diseases. But there are useful and somewhat underestimated groups of drugs that, apparently, will occupy their niche in the complex treatment of patients.
Supplements or food?
All the experts we interviewed were unanimous on this issue. Why take magnesium supplements at all if you are not deficient when there are so many delicious foods around that are rich in this micronutrient? Here are some examples.
- Dark Chocolate: Approximately 64 mg of magnesium per slice (16% DV).
- Avocado: One medium-sized fruit contains 58 mg of magnesium (15% of the daily requirement).
- Cashews: A 28g handful of cashews provides 82mg of magnesium (20% of the daily requirement).
- Brazil nuts: 100 g (approximately 12-15 pieces) cover the daily requirement for magnesium by 100%.
- Beans: A cup of cooked black beans provides 120 mg of magnesium (30% of the daily requirement).
- Banana: one piece contains 37 mg of magnesium (9% of the daily requirement).
- Salmon: Half fillet weighing 178 g contains 53 mg of magnesium (13% daily requirement).
The benefits of normal food do not end with the fact that it is tastier and more nutritious. There are two more important points.
Compatibility.
Dietary supplements with magnesium cannot be taken together with antibiotics (tetracyclines and quinolones), because magnesium forms poorly soluble compounds with them. Real food has no such restrictions.
Side effects.
When taking supplements, an overdose is possible, which is accompanied by unpleasant symptoms such as nausea, abdominal cramps and diarrhea. And this, in turn, can cause dehydration and loss of magnesium. There is no risk of overdosing on nuts, pumpkin seeds and salmon. Also because in this case a “smart” algorithm works. The body itself regulates the level of absorption: it increases from an average 30-40% to a maximum of 80% if there is little magnesium in foods, and reduces to 25% if there is too much.
Magnesium deficiency. Cases from the practice of a neurologist
Clinical observation 1. Hyperventilation syndrome Patient L., 40 years old, chief physician of one of the Moscow clinics. Complaints: low mood, irritability, fatigue, feeling of exhaustion; poor tolerance to changing weather conditions; lability of blood pressure with increases up to 140/100 mm Hg. and more, rapid heartbeat, frequent pain in the heart and dizziness against the background of emotional experiences, accompanied by a feeling of “lack of air” and “coma in the throat”; difficulty falling asleep and daytime sleepiness; increased sweating in the armpits, palms and feet, convulsive movements of the calf muscles. History of the disease. The mild complaints described above have been bothering me periodically over the last year, during which the patient notes a tense interpersonal situation at work and at home. Given the medical background, the patient neglected communication with his colleagues and was treated independently. The diagnostic search excluded somatic pathology. Sedative and restorative therapy was carried out. However, against the backdrop of 2 weeks of hard work and an escalation of the conflict with management, the intensity of the complaints increased. The usual treatment regimens did not improve the condition. Constant pain appeared in the heart area. This forced the patient to contact the Department of Pathology of the Autonomic Nervous System for examination and subsequent treatment. Life story. He grew up and developed as a strong, athletic child. At a young age, he suffered an injury to his right knee joint with full recovery. I was involved in bodybuilding. Among previous diseases, gastritis is indicated. He has been working as a general practitioner since the age of 23. Married, has two children. Upon examination, the condition is satisfactory, the physique is athletic. The background mood is reduced. No somatic disorders were identified. There are no meningeal signs in the neurological status. No pathology was detected from the cranial nerves. There are no paresis. Muscle tone is not changed. Tendon reflexes are moderately animated D=S, there are no pathological signs. The Romberg test is negative, coordination is not impaired. No sensory disorders were identified. When assessing the autonomic nervous system, acrocyanosis of the hands and feet, sweating in the armpits, palms and soles, frequent sighs, uneven depth and frequency of breathing, and emotional lability were noted. When studying neuromuscular excitability at rest, Khvostek's symptom was negative; after 3 minutes of hyperventilation, an increase in neuromuscular excitability was noted (III degree Khvostek's symptom in combination with convulsive sensations in the feet and paresthesia in the calves). Paraclinical examination. Consultation with an ophthalmologist, therapist, ECG, ultrasound examination of the brachiocephalic vessels, radiography of the skull and cervical spine did not reveal any significant pathology. Pathologists did not reveal a general blood and urine test or a biochemical blood test. A study of the microelement composition of hair and psycho-vegetative testing was carried out (Table 1). Its results did not reveal a pronounced anxiety-depressive syndrome in the patient; there was a decrease in the quality of night sleep, levels of well-being, activity and mood. There were autonomic dysfunction and pronounced signs of hyperventilation syndrome, a decrease in stress resistance and quality of life in our patient. Carrying out the “30:15” cardiovascular test and spectral analysis of heart rate variability in a state of relaxed wakefulness and active orthotest made it possible to assess the autonomic regulation and adaptive capabilities of the patient. A decrease in parasympathetic influences on the heart was revealed in the form of a low index “30:15” and a low representation of respiratory influences at rest against the background of excessive sympathicotonia, which led to rigidity of the heart rhythm against the background of tachycardia and increased blood pressure. When an orthostatic load was presented, the detected sympathetic reactivity was provided not by segmental regulatory mechanisms, but by excessive activation of suprasegmental structures, which reflects not only the strain of functioning under normal conditions, but also a violation of adequate adaptive mechanisms in this patient. Hair analysis determined magnesium deficiency compared to normal. Based on the obtained clinical and paraclinical data, the patient was diagnosed with psychovegetative syndrome. Syndrome of vegetative dystonia against the background of chronic emotional stress with hyperventilation manifestations and decreased adaptive capabilities. The patient was prescribed a 2-month course of Magne B6 therapy at a dose of 1 ampoule of a drinking solution 3 times a day for 2 weeks, followed by a transition to taking 1 ampoule 2 times a day with meals. While taking the drug, complaints were reduced. The background mood and sleep improved, activity and performance increased, blood pressure stabilized, heart palpitations, a feeling of lack of air, and cramps in the calf muscles stopped bothering me. Subjective improvement was noted from the middle of the second week of taking the drug. However, increased sweating during excitement and poor tolerance to changes in weather conditions still persisted, but the intensity of these manifestations was much lower. Against the background of an increase in magnesium content in the body, positive dynamics of psycho-vegetative indicators were noted. Despite the fact that magnesium levels only reached subthreshold values, improvements were found in test scores. There was also a beneficial effect on autonomic regulation at rest (vagotonia and increased heart rate variability, normalization of blood pressure and pulse) and orthotest (increased “30:15” index and segmental sympathetic influences in terms of hemodynamics and heart rate variability). This indicates an improvement in vegetative support and the formation of adequate adaptation mechanisms. This, in turn, helps reduce hyperventilation syndrome and increase his resistance to stress while staying in our patient’s previous living conditions. Conclusion. Clinical manifestations of chronic emotional stress were expressed in a decrease in adaptive abilities and were accompanied by a decrease in magnesium content in the body and clinically pronounced autonomic dysregulation in the form of hyperventilation syndrome. Even partial replenishment of magnesium deficiency contributed to the reduction of subjective and objective manifestations of the latter. Clinical observation 2. Episodic tension headaches Patient L., 52 years old, complained of frequent (up to 15 times a month) diffuse headaches of a compressive nature in the second half of the working day or after emotional stress, of average intensity (intensity according to the visual analog scale was 6–7 points). The headache was accompanied by a feeling of rapid heartbeat, pain in the heart area, numbness in the hands and feet, and difficulty breathing like a “coma in the throat.” The headache was not accompanied by nausea, photo- or phonophobia, and was not aggravated by the patient’s usual activities. Headaches decreased after taking analgesics in combination with muscle relaxants and sedatives (for example, No-shpalgina with Valocardin). The patient also complained of low mood, tearfulness, fatigue, sleep disturbances in the form of difficulty falling asleep and early morning awakenings, poor tolerance of stuffy rooms, and periodic pain in the heart area. History of the disease. She became ill 9 years ago when, due to chronic emotional stress (divorce from her husband), sleep was disturbed and periodic diffuse pressing headaches occurred. She was treated on an outpatient basis with nootropic, vascular and vitamin preparations with a positive effect. I noticed an improvement in my health in the spring and summer, during vacations. About a year ago, due to dismissal from work and the onset of menopause, headaches became more frequent and more intense. Conventional treatment regimens did not improve the patient's condition. Against this background, pain appeared in the heart area and sensations of respiratory distress. Life story. Among previous diseases, gastritis is indicated. Referred by a therapist to the Department of Pathology of the Autonomic Nervous System for examination and treatment. Upon examination, the condition is satisfactory. The background mood is reduced. No somatic disorders were identified. There are no meningeal signs in the neurological status. No pathology was detected from the cranial nerves. There are no paresis. Muscle tone is not changed. Tendon reflexes are moderately reduced D=S, there are no pathological signs. The Romberg test is negative, coordination is not impaired. No sensory disorders were identified. The temporal, masticatory, trapezius and splenius muscles of the neck without an accent on the side, the pectoralis major and minor muscles with an accent on the left and without the presence of trigger points in them are sharply painful and tense during palpation. When assessing the autonomic nervous system, increased neuromuscular excitability (III degree Chvostek's symptom), persistent pink dermographism, lability of heart rate, generalized sweating, frequent sighs, uneven depth and frequency of breathing, and decreased mood were noted. Paraclinical examination. Consultation with an ophthalmologist, therapist, ECG, ultrasound examination of the brachiocephalic vessels, radiography of the skull, cervical and thoracic spine did not reveal any significant pathology. Psychovegetative testing was carried out, the results of which revealed that the patient had moderate depression (12 points on the Beck test with a norm of up to 9 points), reactive anxiety (43 points on the Spielberger test with a norm of up to 30 points), as well as a decrease in the quality of night sleep (13 points with a norm of 22 points) and quality of life (by 80% with a norm of up to 10%). When studying the magnesium content in a hair biopsy, the level of the microelement was low and amounted to 19 μg/g. Thus, the patient had the following syndromes: 1. Cephalgic syndrome (frequent, but not more than 15 days a month, diffuse bilateral contracting headaches with an intensity of 6–7 points on a visual analogue scale, not aggravated by habitual daily physical activity, but significantly disrupting social activity of the patient, reducing her performance, worsening her quality of life). 2. Psychovegetative syndrome (in the form of moderate depression, anxiety, asthenia, dyssomnia, cardialgic and hyperventilation syndromes). 3. Painful tension of the pericranial, cervical and pectoral muscles. 4. Established magnesium deficiency. Based on this, the patient was diagnosed with psychovegetative syndrome. Anxiety-depressive syndrome of moderate severity. Episodic tension headaches with tension in the muscles of the neck, scalp aponeurosis and pectoral muscles. Menopause. The patient was prescribed a 2-month course of therapy with Magne B6 at an initial saturating dose of 2 tablets 3 times a day for 2 weeks, followed by transfer to a 2-time dose for 2 months. During this period, the patient actively kept a “Headache Diary”, in which she noted the duration in hours and intensity in points on the visual analogue scale of headaches. During 2 weeks of therapy, pain intensity (4 points) and frequency (1–2 times a week) significantly decreased, and sleep improved (20 points). By the end of the 8th week, the patient was not bothered by headaches. A repeat examination after 2 months revealed a pronounced positive trend in the form of an increase in magnesium content in the body (41 mcg/g). This was accompanied by a reduction in cephalgic, psychovegetative syndromes and painful muscle tension. Headaches did not bother me. My mood improved and I felt more energetic. Depressive and anxiety symptoms were not detected either clinically or based on the results of psychometric testing. There were no signs of hyperventilation syndrome. Cardialgia and interruptions in heart function did not bother me. The drug had a beneficial effect on the muscular component of the pain syndrome: there was no tension in the pericranial, cervical and pectoral muscles. The patient's quality of night sleep significantly improved (23 points). All this contributed to improving the patient’s quality of life. Conclusion. A course of Magne B6 in a patient suffering from episodic tension headaches with moderately severe psychovegetative syndrome and painful muscle tension contributed to the reduction of the latter, thereby significantly improving the patient’s quality of life and her social adaptation.
Discussion. The presented clinical case shows the development of tension headaches in a patient with increased anxiety during a period of hormonal changes who is not receiving adequate therapy. In the treatment of episodic tension headaches in this patient, it was necessary to influence the main mechanisms involved in the formation of headaches: correction of mental disorders (anxiety), reduction of muscle tension. Chronic stress, combined with hormonal changes in the body, led to decompensation and transformation of rare episodic tension headaches into frequent ones. It should be noted that the clinical picture of such headaches is combined with pain syndromes of other localization, for example, pain in the heart and abdomen, which are somatic masks of depression. Frequent comorbid syndromes with headaches are permanent or paroxysmal psychovegetative disorders.
Clinical observation 3. Chronic fatigue A 33-year-old woman complained of feeling exhausted, daytime sleepiness, increased fatigue, decreased concentration and memory, emotional lability in the form of sudden mood swings, irritability and tearfulness, as well as diffuse muscle pain, including left half of the chest, sleep disturbances in the form of difficulty falling asleep and shallow sleep, which did not bring a feeling of rest and recuperation. When the weather changes, there is a deterioration in health, poor tolerance of cold and heat. History of the disease. Throughout the year, general weakness, fatigue, attention problems, and irritability have been a concern. 6 months ago, after the sudden death of my father, sleep disturbances and tearfulness appeared. Diffuse muscle pain also developed. The patient underwent a comprehensive diagnostic examination, which made it possible to exclude organic somatic pathology. Slightly expressed radiological signs of spinal osteochondrosis were revealed. The attending physician referred the patient for consultation with subsequent therapy to the Department of Pathology of the Autonomic Nervous System of the Research Center MMA with a diagnosis of “Neurocirculatory dystonia. Astheno-neurotic syndrome." Life story. The patient, from her first normal pregnancy, grew up and developed as a healthy child, but since childhood she was easily vulnerable, tried to avoid conflict situations, and suffered from grievances for a long time. She was interested in music, drawing, and writing poetry. She was the only child in the family. Denies chronic diseases of internal organs. Menstrual function was not impaired, there were no pregnancies or childbirths. Social status – unmarried, works as a leading accountant in a large foreign company. On examination, the condition is satisfactory, the physique is asthenic. The background mood is reduced. No somatic disorders were identified. There are no meningeal signs in the neurological status. No pathology was detected from the cranial nerves. There are no paresis. Diffuse painful muscle tension is noted in the head, neck, and chest. Otherwise, muscle tone is unchanged. Tendon reflexes are alive D=S, there are no pathological signs. The Romberg test is negative, coordination is not impaired. No sensory disorders were identified. When assessing the autonomic nervous system, spotty hyperemia on the neck, face and chest, increased sweating of the palms and feet, and emotional lability were noted. When studying neuromuscular excitability at rest, grade II Khvostek’s symptom, after 3 minutes of hyperventilation, an increase in neuromuscular excitability was noted (grade III Khvostek’s symptom in combination with paresthesia in the feet). Paraclinical examination. Based on the results of the studies, minimal manifestations of spinal osteochondrosis were identified. The use of algometry made it possible to identify a decrease in pain sensitivity thresholds in the studied muscles of the head, neck and pectoral muscles, which manifested itself in the occurrence of intense pain with a slight pressure force (on average 4–5 lb/sm2) at standard points. A study was carried out on the microelement composition of hair, psychological and vegetative testing. The results showed that the patient had an established magnesium deficiency (the magnesium content in the hair biopsy, the microelement level was 26 mcg/g, with a norm of 50 mcg/g) was accompanied by a psychovegetative syndrome in the form of anxiety (16 points on the hospital anxiety scale with a norm of up to 7 points), asthenia (33 points on the activity scale with a norm of 50 points), sleep disturbance (16 points on the night sleep quality scale with a norm of 22 points), a decrease in quality of life by 35%. Autonomic dysfunction was manifested in increased activity of the sympathetic-adrenal system at rest and insufficient activation of functional reserves when test loads were presented. Based on the obtained clinical and paraclinical data, the patient was diagnosed with psychovegetative syndrome. Astheno-neurotic syndrome. The patient was prescribed a 2-month course of Magne B6 therapy at a dose of 1 ampoule of a drinking solution 3 times a day for 2 weeks, followed by a transition to taking 1 ampoule 2 times a day with meals. After 2 months of regular use, the patient’s condition improved, complaints were reduced. The patient became more active, her sleep and emotional background normalized, she became less sensitive to weather changes, sweating decreased, and muscle pain stopped bothering her. Objectively: against the background of an increase in magnesium content in the body to 47 mcg/g, positive dynamics of psycho-vegetative indicators were noted. Levels of anxiety and asthenia did not exceed standard values. The quality of night sleep, neuromuscular excitability and pain sensitivity threshold were restored. Indicators of autonomic tone did not differ from those of practically healthy people. When conducting an active orthotest, insufficient activation of adaptive mechanisms still remained, but there was already a tendency towards the adequacy of vegetative support. The patient's quality of life improved. Discussion. This clinical case illustrates the formation of astheno-neurotic manifestations of magnesium deficiency in a patient initially belonging to the asthenic type of people. Low constitutional functional activity of the body systems, combined with the developed energy deficiency against the background of stressors, led to the predominance of asthenic manifestations of psychovegetative syndrome. The use of a magnesium-containing drug made it possible to improve energy metabolism - a basic characteristic of the body's metabolism, which contributed to the improvement of vegetative status and maintenance, as well as the normalization of psycho-vegetative relationships and increased activity of the patient. Thus, the clinical cases presented demonstrate the importance of magnesium as a mineral that regulates the activity of the nervous system, its necessity in regulating optimal metabolism and the functioning of the body. However, the magnesium content in modern human food is decreasing. Reduced levels of the microelement were also found in people with certain chronic somatic and mental illnesses. All this showed the need to increase awareness of the importance of magnesium intake and its potential therapeutic role in a range of diseases. In their practice, doctors are already faced with clinical manifestations of established magnesium deficiency. Research in recent years shows the effectiveness of magnesium in neurological and mental pathologies, eclampsia and preeclampsia, arrhythmia, severe asthma and migraine. Magnesium-containing therapy has demonstrated promising results in reducing the risk of metabolic syndrome and insulin resistance, improving metabolism, reducing symptoms of dysmenorrhea, and reducing leg cramps in pregnancy. Because magnesium is excreted through the kidneys, it should be used with caution in patients with kidney disease. However, long-term intake of magnesium citrate helps to normalize the metabolism of purines and oxalates, which is used in the prevention and treatment of metabolic disorders. To prevent magnesium deficiency, it is recommended to include green leafy vegetables, nuts, legumes, and whole grain products in the diet [9]. In cases of established magnesium deficiency or in patients with symptoms similar to those described by us, it is recommended to supplement magnesium with bioorganic salts (lactate, pidolate or citrate), which have a high degree of absorption by the human body [4].
Literature 1. Pathophysiology. Lecture course; Textbook/P.F. Litvitsky, N.I. Losev, V.A. Voinov and others; Ed. P.F. Litvitsky.– M., 1995.–752 p., ill. 2. Spasov A.A. Magnesium in medical practice, Volgograd, 2000, 268 pp. 3. Durlach J, Bac P, Durlach V, Bara M, Guiet–Bara A. Neurotic, neuromuscular and autonomic nervous form of magnesium imbalance. //Magnes Res. 1997 Jun;10(2):169–95. 4. Gromova O.A. Magnesium and pyridoxine: basic knowledge, M.:, 2006, 223s 5. Jacka FN, Overland S, Stewart R, Tell GS, Bjelland I, Mykletun A. Association between magnesium intake and depression and anxiety in community–dwelling adults: the Hordaland Health Study. //Aust NZJ Psychiatry. 2009 Jan;43(1):45–52 6. Eby GA 3rd, Eby KL. Magnesium for treatment–resistant depression: a review and hypothesis. //Med Hypotheses. 2010 Apr;74(4):649–60 7. Nechifor M. Magnesium in major depression. // Magnes Res. 2009 Sep;22(3):163S–166S 8. Vorobyova O.V., Akarachkova E.S. Magne B6: experience of 5 years of clinical use in neurological and therapeutic practice // Farmateka 2008 No. 20 P. 73–80 9. Guerrera MP, Volpe SL, Mao JJ. Therapeutic uses of magnesium. //Am Fam Physician. 2009 Jul 15;80(2):157–62 RU.MGP.10.09.16