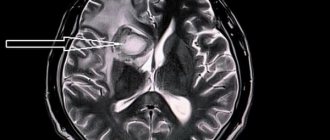
Toxoplasmosis on MRI of the brain Magnetic resonance imaging is a painless and informative way to study the brain. Layer-by-layer MR scanning allows you to examine in detail all parts of the organ and evaluate their structure. Using certain sequences, it is possible to study in detail the white and gray matter, blood vessels, and ventricular system.
MRI is considered an effective method for identifying focal brain lesions. These include limited areas with a disturbed structure inside the substance of the organ. Such changes are often accompanied by mass effect, swelling, and deformation of the surrounding areas. Lesions in the brain on MRI appear as areas of change in the MR signal. Based on specific features, location, size and degree of influence on surrounding structures, the radiologist can make assumptions about the nature of the pathology. Using the information listed, the doctor makes a diagnosis, makes a prognosis for the patient and selects treatment.
Localization
- Epiphysis,
- epiphysis stalk,
- Choroid plexus,
- Dura mater (falx, tentorium cerebellum),
- Ligaments (petrosphenoid and intersphenoid),
- Pituitary,
- Internal carotid artery (cavernous part),
- Basal ganglia and dentate nucleus.
Physiological intracranial calcifications on photographs in anteroposterior and lateral projections:
- - pineal gland;
- - bridle;
- - choroid plexus;
- — sickle around the sagittal sinus;
- - dura mater;
- - sickle (free edge)
- - tent;
- - petrosocuneiform ligament;
- - intersphenoid ligament;
- - pituitary gland;
- — internal carotid artery (cavernous part);
- - basal ganglia;
- - jagged nuclei.
Treatment of brain craniopharyngioma
Treatment of craniopharyngiomas consists of radical removal of pathological foci. Much depends on the location of the tumor, so the choice of treatment tactics depends on the individual characteristics of the patient’s diagnosis. The type of access is selected based on diagnosis and depends on the subtype of the tumor and its topographic and anatomical features. The main goal of surgical treatment is complete (total) removal of brain craniopharyngioma, but not in all cases the craniopharyngioma can be completely excised (subtotal excision).
Total removal of the tumor is called surgical treatment when no remnants of neoplasia are detected during a repeat control examination. Subtotal removal is considered a radical treatment in which it is impossible to remove the tumor completely or, after removal, parts of pathological tissue remain in the brain tissue. As a rule, with subtotal removal, the doctor is forced to leave parts of the neoplasia near the bottom of the third ventricle of the brain, on large vessels and other vital elements.
After removal
After removal of a brain craniopharyngioma, conservative treatment is carried out in the form of radiotherapy and chemotherapy, because treatment should always be comprehensive, which improves the overall outcome of therapy.
Radiation therapy is an auxiliary treatment. It is prescribed in the postoperative period or in the presence of relapses of neoplasia. Radiation has a number of side effects, for example, as a result of radiation treatment, mental development may suffer, endocrine pathologies may increase, vision problems, dementia and other negative phenomena may occur.
Chemotherapy consists of prescribing cytostatic drugs to stop protein synthesis in atypical cells, and some of them die. After tumor removal, the patient may be prescribed glucocorticoids. Treatment with them helps reduce negative signs and swelling. As the condition improves, they are gradually canceled.
Choroid plexuses
Choroid plexuses can calcify in all ventricles, most often this occurs in the vestibular part of the lateral ventricles (the connection of the body of the lateral ventricle with the posterior and temporal horns), projecting in the lateral view approximately 2-3 cm behind and slightly below the epiphysis. In the anteroposterior view, plexus calcifications project approximately 3 cm from the midline and are usually symmetrical, although some disparity in size between different sides is sometimes present. The amount of calcification can vary significantly and is not clinically significant. Widespread plexus calcifications may be found in neurofibromatosis.
MRI of pineal cyst
Cyst-like transformation of the epiphysis is a rare pathology. The frequency of occurrence is one and a half percent among all brain diseases. Benign formation is determined by the absence of damage to surrounding tissues. Repeated MRI reveals cyst growth at distant intervals. Severe damage to the hemispheres is rarely observed, so early diagnosis of the pathology is difficult.
Dynamic growth of an epiphysis cyst is rarely observed. Within a year, two magnetic resonance scans of the brain are sufficient to determine changes. Education rarely has a negative impact on the functioning of the pineal gland.
Causes of development of cystic cavities of the pineal gland:
- Parasitic (echinococcosis, alveococcosis);
- Congenital (with toxicosis of pregnant women);
- Local hemorrhage.
Echinococcosis is a helminthiasis that occurs after ingestion of parasites with food. The helminth, entering the hemispheres of the pineal gland, is limited by a protective capsule, which protects against the damaging effects of immune factors. The vital activity of the worm is accompanied by the formation of a large amount of toxic products and tissue decay substances. Exposure to chemical compounds leads to an increase in the size of the cystic cavity. Over the course of a year, cystic growth can double in size.
Little knowledge of the structure of the epiphysis during a cyst does not allow clearly verifying pathological changes against the background of the existence of a cystic cavity. The asymptomatic course of the pathology does not allow timely diagnosis. Only large hydatid cysts can provoke clinical symptoms:
- Headache;
- Overwork;
- Stress;
- Impaired coordination of movements.
Head pain syndrome with cystic transformation is not associated with specific causes and occurs suddenly. Pathological changes are combined with other clinical conditions:
- Damage to visual function;
- Double vision of objects;
- Hydrocephalus (dropsy);
- Vomiting and nausea.
The increase in intracranial pressure is caused by compression of the excretory duct by a large formation, leading to cerebral hypertension.
Echinococcal cysts are characterized by intoxication and febrile manifestations. An increase in temperature leads to an acceleration of biochemical reactions, an increase in heart rate and respiratory activity. The nosology of parasitic etiology is accompanied by a number of additional clinical signs:
- Dementia;
- Depressive syndrome;
- Epilepsy seizures;
- Rave.
Microcystic transformation of the epiphysis on magnetic resonance imaging is characterized by the appearance of a heterogeneous signal due to cavity inclusions. Asymmetry of the lateral ventricles indicates possible hydrops.
Normal sizes of the pineal gland on MRI:
- Symmetry of the lateral ventricles;
- Lateral ventricle index – 18-22;
- Anterior horns on the right and left – 0.8-1 cm;
- Absence of periventricular infiltration;
- Exclusion of pathological formations of the cerebellopontine angle;
- Maintaining patency of the ear canals;
- Chiasmal region – without features;
- The location of the tonsils is at the level of the foramen magnum.
Microcysts of the epiphysis are often combined with mixed hydrocephalus.
Hydrocephalus occurs against the background of blockade of the ventricles and subarachnoid spaces. The complication requires surgical intervention to eliminate the cause of cerebrospinal fluid microcirculation disorders. The frequency of dangerous consequences of the pathology is quite low.
MRI of pineal cyst
Calcification of the dura mater
Calcification of the dura, skull and/or tentorium occurs in approximately 10% of cases, and each variant has its own characteristic features. Calcification of the dura mater around the sagittal sinus appears V-shaped at the apex in the anteroposterior view. Calcifications in this area can sometimes be caused by calcified pachyonic (arachnoid) granulations (diverticulum-like protrusions of the arachnoid space that pierce the dura mater and project into the lumen of the main sinuses and adjacent venous lakes).
Symptoms of craniopharyngiomas
With the formation and growth of a tumor, characteristic clinical signs of three types are formed:
- Hormonal and metabolic, which causes the development of diabetes insipidus, hypogonidism, impaired lipid metabolism, developmental delays or, conversely, increased body weight growth, enuresis, abnormalities of puberty, weakening of muscles, decreased performance, disruption of the reproductive system of various types.
- Visual – characteristic of craniopharyngiomas. They are among the first to appear (in 50% of cases these are the very first symptoms of the presence of pathology).
- Dictated by intracranial hypertension, which is more typical for tumors localized in the cavity of the third ventricle of the brain.
The note. The nature and intensity of the symptoms depends on the location of the tumor and its size. If it is large and puts pressure on neighboring areas, clinical signs will be more varied.
Calcifications of the falx
Normally they are located anteriorly and are clearly visible as linear stripes or plates on one or both leaves of the falx. On photographs in the anteroposterior projection, calcifications along the free edge of the tentorium have the shape of an inverted letter “V”. The amount of calcification of the dura mater, falx and tentorium is usually of no clinical significance, especially when the calcification is more or less diffuse.
Falx and dura calcifications are found in two thirds of patients with basal cell nevus (Gorlin-Goltz) syndrome, and widespread dural calcifications are mentioned in pseudoxanthoma elasticus.
From the book “Brain Tumors. CT and MRI diagnostics.” View/order
Calcification of the falx cerebri can lead to the formation of local large calcifications and bone density, which over time can acquire the structure of spongy bone (arrowhead in Fig. 1041, 1042). Calcification can also be an elongated form creeping along the dura mater (arrows in Fig. 1044) with MR signal characteristics similar to diploic substance (Fig. 1044-1045). In addition, dysembryogenetic fat may occur along the falx cerebri (arrows in Fig. 1043), as evidenced by negative density on CT. Petrification of the dura mater appears with age and can occur years after surgery (Fig. 1046), reflecting blood impregnation and encrustation of the dura.
MRI of the pineal gland for cysts, calcifications, tumors
The pineal gland is located between both hemispheres (right and left).
The organ controls the functioning of the hypothalamic-pituitary system and melatonin. The pineal gland controls the sleep-wake cycle. Regulation of the circadian rhythm under the control of the organ ensures optimal development of the body. Most gland diseases pass without clinical symptoms. They are detected by chance after performing magnetic resonance imaging.
List of pathologies of the pineal gland detected by MRI of the brain:
- Combination of depression with delusional disorders, hallucinations;
- Unsteadiness of gait, incoordination of walking;
- Vestibular pathology;
- Frequent vomiting, nausea;
- Increased intracranial pressure;
- Increased skull size due to dropsy (hydrocephalus).
Magnetic resonance imaging of the pineal gland reveals three main nosological forms:
- Calcifications;
- Cysts;
- Benign and malignant neoplasms.
Calcinosis develops due to the accumulation of calcium salts. Places of calcification lose functionality. The larger the lesion, the brighter the symptoms.
Cystic transformation involves the formation of cavities with limited contours and liquid internal contents. The danger of pathology is blockage of the excretory duct. Violation of secretion drainage causes hormonal disorders, a list of signs for which neurologists send for an MRI of the epiphysis of the brain.
Cysts can have a congenital etiology or be caused by acquired factors (alveococci, echinococci, fungal infections). Severe cystic transformation of the pineal gland leads to psycho-emotional disorders. Changes in behavioral reactions and incoordination when walking cause disability.
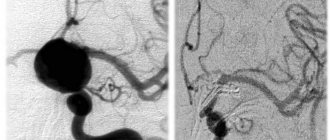
Detection of a pineal gland tumor involves the use of contrast tomography - MR angiography. The procedure involves intravenous administration of an enhancement drug followed by a scan. A series of images is processed by software capable of creating a three-dimensional model of the object.
Arteriosclerotic calcifications
Arteriosclerotic calcifications of the internal carotid artery are often visible along its passage through the cavernous sinuses. Such calcifications can vary in size from small flakes to complete visualization of the carotid siphon. On lateral views, such calcifications are superimposed on the image of the sella turcica, whereas ring-shaped calcifications may be visible on one side of the sella on anteroposterior views.
Cytohistological features
Structurally, craniopharyngiomas are divided into tumors consisting of dense tissue and containing cysts. The latter can be from two to five centimeters in diameter, in rare cases larger cysts form. They are characterized by slow growth.
As a rule, areas of cystic craniopharyngioma of the brain contain up to 50 cysts, but sometimes their number can reach two hundred. In appearance, these formations are yellow or clay-colored, with a dense capsule, well associated with the brain tissue and its vessels (the tumor is supplied with blood from the cerebral vascular basin).
Note. Over time, the tissue structure and morphological features of craniopharyngioma may change.
As it develops or when the tumor has been present for a long time, necrosis may form, which leads to cyst-forming processes. Cysts are filled with fluid with a large amount of lipids (up to 100%), the exudate may also contain fatty acids and cholesterol crystals. Salt deposits often form on the outside of the capsules.
The cytological structure of craniopharyngioma is represented by epithelial tissue with cells of varying degrees of differentiation. Depending on the structure, there are two types:
- Adamantine-like craniopharyngioma of the brain is diagnosed most often (about 85% of all tumors in this group). The tumor is more typical for childhood. Its tissues consist of the remains of embryonic tissues. Neoplasms of this type are characterized by polymorphism. They are compact (10% of cases), cystic (25-32%) and mixed (up to 60% of cases).
- Papillary craniopharyngioma of the brain is more typical for adults (30-40 years old); it is extremely rarely diagnosed in children. They account for approximately 15%. Cytologically it is represented by metaplastic cells. As a rule, neoplasias are solid, petrification is insignificant or absent.
In addition to cells of epithelial origin, craniopharyngiomas can be represented by epidermal epithelium. In tumors of this type, various degenerative processes, cysts, or stromal ossifications form. The tumor capsule is formed by connective or hyal tissue. Different types of histological structures can be considered as phases of craniopharyngiomas.
Calcifications of the basal ganglia
Basal ganglia calcifications are found in many diseases, but are most often discovered incidentally in healthy adults. They have no clinical significance. Calcifications vary in size from punctate to fused opacities with a characteristic location: on photographs in the anteroposterior projection, calcifications are located symmetrically parasagittally, while on photographs in the lateral projection they can take on a slightly curved shape and are approximately located parallel to the scaly suture. Sclerosis along the squamous suture on photographs in the lateral projection sometimes has the appearance of a stripe-like darkening and should not be confused with calcifications of the basal ganglia.
Calcifications in the dentate nucleus of the cerebellum are less common than in the basal ganglia, but are found in the same conditions. On a lateral view of the skull, such calcifications are often masked by mastoid air cells, but they are best seen in the occipital (Towne) projection as symmetrical crescentic opacities.
Epidemiology and embryology
Among the total number of primary brain tumors, craniopharyngiomas account for 1.2-4.6%. In patients under 16 years of age, the incidence of tumors ranges from 5-10%, and in adults it can reach up to 60%. There are two age peaks for the high probability of developing craniopharyngiomas: in children from 6 to 16 years and in adults from 48 to 75 years. Every year, from 0.5 to 2 cases of this type of tumor are diagnosed per 1 million population.
The note. Most neoplasms of this type are diagnosed in China (up to 6.5% of cases), least of all in Australia (up to 1.5%).
According to the theory proposed by Erdheim (it has greater scientific weight), craniopharyngiomas in the brain are formed from the remnants of the tissue structure of the epithelial embryonic tissue of Rathke's pouch, which is an invagination of the primary oral tube. From this structure, at the initial stages of embryogenesis, the anterior lobe of the pituitary gland, as well as its tuberal region, is formed.
Folk remedies to help
Treatment with folk remedies is one of the ways to correct the disease and stabilize the level of calcium in the blood. Calcification is a consequence of the failure of metabolic processes occurring in the body. This is why it is quite logical that without a proper diet this cannot be advice.
The patient should limit the consumption of foods rich in this mineral. It should be excluded from the daily diet:
- dairy products;
- Herbs and most vegetables;
- Spicy dishes;
- smokes;
- sweets;
- cocoa;
- yeast products;
- Spices and spices.
The diet consists of consuming foods rich in magnesium. These:
- Porridge - buckwheat, oatmeal, barley, millet
- Leggear Boats - peas, beans.
- Brussels sprouts.
- Nuts - cashews, pine nuts, hazelnuts, peanuts.
Eating suitable foods helps reduce calcium levels and indicate balance.
Therapeutic infection can be used to clear plaque from blood vessels:
- Chamomile, English herbs and birch donuts will be needed for preparation. All 100 grams. All ingredients are crushed and mixed.
- Take 500 ml of boiling water and 1 tablespoon of this herbal harvest and mix everything.
- Leave this “cocktail” for 30 minutes. It is then filtered and divided into half: drink 1 tablespoon in the morning and evening. The duration of treatment is 14 days.
Prerequisites for the development of the disease
The following factors contribute to the occurrence of this disease:
- Unstable functioning of the parathyroid glands;
- renal dysfunction;
- severe intestinal diseases;
- rheumatism of the heart;
- altered pH level;
- hormonal imbalance;
- genetic predisposition;
- metabolic disorders.
Additional reasons for the development of this disease:
- high levels of vitamin D;
- cancerous tumors;
- bad habits;
- obesity;
- stress;
- injuries;
- diabetes;
- hypertension;
- atherosclerosis;
- abnormalities in the structure of blood vessels and heart muscle.
The formation of calcifications can also be facilitated by a severe form of dystrophy with profound changes in the structure of vital organs.
Life prognosis after surgery
Patient survival depends on the effectiveness of treatment, stage, presence of metastases and relapses. The location of the tumor is of no small importance. The sooner a pathological neoplasm is identified and surgical treatment is performed, the better the prognosis.
With the classic type of tumor of the 2nd degree of malignancy in patients under 40 years of age after surgery and complex treatment, the prognosis is favorable: the average period without relapse is 5 years, and the ten-year survival rate remains at 35%. About 30% of patients will survive more than 5 years after the initial diagnosis. The prognosis worsens in proportion to the worsening degree of malignancy.