Vascular diseases of the brain are among the most serious medical and social problems of our time, which is due to their significant share in the structure of morbidity, disability and mortality of the population. The prevalence of cerebrovascular diseases in all regions of the world is so great that at the end of the 20th century they became one of the main causes of mortality in industrialized countries, including Russia, and in some countries they occupy third and even second place.
Among vascular diseases of the brain, the most common and severe in its outcome is stroke. Every year, about 6 million cases of stroke are registered worldwide - 0.2% of the world's population; During the same time, according to the World Health Organization, 4.6 million people die from stroke, which is 9-12% of all mortality. Moreover, in recent years, these cases of cerebral strokes have been steadily increasing. In the structure of cerebral strokes, the leading place is occupied by ischemic disorders of cerebral circulation. In most developed countries of the world, the proportion of various types of stroke is: ischemic stroke - 80-85%; intracerebral hemorrhages - 10%; subarachnoid hemorrhages - 5%.
It should be emphasized that in a significant number of people, acute cerebrovascular accidents develop during the period of creative activity and professional skill, i.e., their significant “rejuvenation” is noted. The development of acute cerebrovascular accidents (stroke) is associated with cerebral hemorrhage (hemorrhagic stroke) or ischemic brain damage (ischemic stroke or cerebral infarction). There are also transient cerebral circulatory disorders in which neurological symptoms persist for no more than a day.
Ischemic brain lesions
The main cause of ischemic stroke is a decrease in cerebral blood flow due to stenotic and occlusive lesions of the great vessels of the neck and arteries of the brain.
In the development of ischemic stroke (cerebral infarction), an important role is played by the blockage of cerebral vessels by microthrombi, which are formed as a result of atherosclerotic plaques breaking off and moving through the vessels.
The main etiological factors leading to damage to both extracranial and intracranial vessels include atherosclerosis, hypertension, and rheumatism. Much less often, the cause of obstruction of the patency of the carotid arteries is cicatricial traumatic and inflammatory extravascular lesions, fibromuscular dysplasia resulting from radiation therapy, as well as pathological bends of blood vessels.
The clinical picture of cerebral infarction depends on the location of the lesion, and the severity and persistence of symptoms depends on the size and condition of the collateral systems. Thrombosis of the internal carotid artery is characterized by decreased visual acuity or blindness on the affected side and hemiparesis or hemiplegia on the opposite side. With arterial stenosis, these disorders can be temporary,
Risk group
The risk group includes people with infectious pathologies during the neonatal period. The likelihood of developing vascular diseases of the brain increases significantly with hemolytic anemia, surgery and head injuries. The mother’s poor lifestyle (abuse of alcohol and tobacco products) can also negatively affect the condition of the child’s brain. A family history of cardiovascular pathologies (for example, myocardial infarction or arterial hypertension in close relatives) doubles the risk of developing cerebrovascular diseases.
Hemorrhagic stroke
Intracerebral hemorrhages are most common, subarachnoid hemorrhages are less common, and subdural hemorrhages are even less common.
In 60-70% of patients, the cause of hemorrhage was arterial hypertension, in 20% of cases - arterial aneurysm and arteriovenous malformation, in others - various diseases associated with atherosclerosis.
Among the reasons that determine the development of hemorrhagic stroke, the main place is occupied by hypertension and atherosclerosis.
Hemorrhagic stroke develops predominantly acutely, often without warning. It is characterized by a sudden loss of consciousness, sometimes after one or more vomitings. The patient's face becomes bluish-red, the pulse is tense and slow, breathing is loud and bubbling, the body temperature soon rises, the head and eyes are often turned to the side. Focal symptoms are primarily characterized by motor disturbances in the form of paresis and paralysis of the limbs on the side opposite to the hemorrhage, which arise as a result of compression of the internal capsule or vessels supplying it with blood by the hematoma.
How vascular lesions affect the brain
For proper functioning of the brain, it is important to maintain cerebral blood flow at a constant level. That is why this organ has a fairly intense blood supply. Blood flows to the brain through four main vessels in the neck: two carotid and two vertebral arteries. They connect at the base of the brain, forming the so-called Circle of Willis. From it, many smaller vessels diverge to different parts of the brain. This is a defense mechanism in case a catastrophe occurs in one of the four main vessels. The problem is that vascular diseases also affect smaller vessels that supply blood to distant parts of the brain and do not have collaterals (side or bypass blood flow paths) and compensatory mechanisms.
Intracranial arterial aneurysms
Arterial aneurysms are a limited protrusion of the wall of an arterial vessel, looking like a thin-walled sac, in which a bottom, middle part and neck are distinguished. There is no muscle layer in the wall of the aneurysm, and in the bottom area the wall is noticeably thinner and can rupture. Most aneurysms are located in the arteries of the base of the brain, mainly in the vessels of the arterial circle of the cerebrum (Circle of Willis). The sizes of arterial aneurysms vary - from a few millimeters to giant ones, with a diameter of over 2.5 cm.
During aneurysmal disease, three periods are distinguished: pre-hemorrhagic, hemorrhagic and post-hemorrhagic.
In the pre-hemorrhagic period, which often lasts for years, the course of the disease is asymptomatic or nonspecific transient symptoms appear (headache, sometimes migraine-like in nature, temporary diplopia, dysfunction of the cranial nerves).
During the hemorrhagic period, the aneurysm ruptures with intracranial hemorrhage.
The clinical picture of the hemorrhagic period is largely determined by the size and location of the hemorrhage, repeated hemorrhages, and accompanying local and general symptoms of cerebrovascular accident.
In the posthemorrhagic period, clinical signs of an aneurysm may disappear or their severity may weaken, especially with spontaneous thrombosis of the aneurysm. Often, in the posthemorrhagic period, persistent general cerebral and focal symptoms remain, and a wide variety of visceral disorders are also added.
Repeated ruptures of arterial aneurysms are observed in more than half of patients; they can occur after several months or even years.
Classification of vascular diseases of the brain
There are two main groups of vascular pathologies: acute and chronic cerebrovascular accidents. The first group is divided into three subgroups: transient cerebrovascular accidents, cerebral strokes, mixed strokes. Transient disorders of cerebral circulation include transient ischemic attacks and hypertensive crises. Brain strokes are ischemic and hemorrhagic. Hemorrhagic strokes are divided into subarachnoid hemorrhage, parenchymal-subarachnoid hemorrhage, and ventricular-parenchymal-subarachnoid hemorrhage. Ischemic strokes, in turn, are divided into lacunar, atherothrombotic, cardioembolic and hemodynamic stroke.
The second group includes: chronic subdural hematoma, initial manifestations of cerebrovascular insufficiency, subcortical vascular dementia, discirculatory encephalopathy. The initial manifestations of cerebrovascular insufficiency are divided into two stages. The first stage is characterized by the absence of neurological manifestations. At the second stage, neurological manifestations are clearly expressed. Discirculatory encephalopathy is the most common among chronic cerebrovascular accidents. It is divided into three main stages:
- The first stage is moderately severe, characterized by diffuse symptoms. The patient may complain of short-term headaches, periodically suffer from sleep disorders and increased irritability.
- The second stage is more pronounced; clinical manifestations form in it. The person often experiences surges in blood pressure, loss of space, and cognitive impairment. As a rule, at this stage the disease is most often diagnosed.
- The third stage is pronounced, during which irreversible changes occur in the body. Serious disturbances in memory and cerebral circulation in general appear. In rare clinical situations, complications in the form of strokes are observed (in the absence of timely consultation with a doctor).
Arteriovenous malformations
An arteriovenous aneurysm (malformation) is a congenital malformation of cerebral vessels in which arterial blood is directly discharged into the venous bed, bypassing the capillary network. Such aneurysms consist of a dilated adductor arterial vessel, a tangle of vessels forming an arteriovenous shunt, and one or more sharply dilated efferent veins. The walls of the tangle of vessels of arteriovenous malformation are thinned, and it is almost impossible to determine their arterial or venous origin.
Since in arteriovenous malformation there is no capillary network, part of the blood entering the cerebral hemispheres does not take part in tissue metabolism, so-called hemorrhagic stealing of the brain occurs. This causes persistent cerebral ischemia and causes psychopathological disorders, as well as progressive brain atrophy.
The clinical picture of arteriovenous malformation is varied and depends on its location. Often, arteriovenous malformations are clinically manifested by epileptic seizures or spontaneous intracranial hemorrhages.
The prehemorrhagic period may be asymptomatic or manifest itself as epileptic seizures
Prevention of vascular diseases of the brain
Vascular diseases of the brain are easier to prevent than to cure. To do this, experts recommend leading a healthy lifestyle: engaging in moderate sports, drinking about 1-1.5 liters of water per day (to avoid dehydration), eating properly and following a diet. The diet involves limiting table salt and foods containing large amounts of animal fats (for example, sour cream and fatty meats). Fresh vegetables and fruits should prevail in the daily diet. A split diet is recommended (4-5 meals per day).
The intake of alcoholic beverages should be minimized (or completely abandoned). The emotional component is the key to good health, so you should not be exposed to stressful situations. Sleep should be complete (at least 7 hours of sleep per day are required). Moderate physical activity should be regular; it significantly improves the condition of the body. These include: swimming, yoga, Pilates, cycling.
Exercising and proper nutrition help prevent the appearance of excess weight, while they train the cardiovascular system. At least once a year it is required to undergo a study of the state of cerebral circulation (especially for those who are at risk). This will allow timely detection of pathology.
In order to prevent the progression of multi-infarction conditions, patients are prescribed combination therapy (antiplatelet and anticoagulant). The most suitable anticoagulants are selected depending on blood clotting parameters. If any signs of bleeding appear, it is important to contact a specialist promptly.
Vascular diseases of the brain are often accompanied by dizziness. To prevent them, doctors prescribe medications that affect the autonomic nervous system. To prevent cognitive impairment (memory deterioration, increased inattention), drugs that improve metabolism are prescribed. In the presence of movement disorders, therapeutic exercises, physiotherapy, massage and other methods of rehabilitation therapy are useful.
Aneurysms of cerebral vessels of various locations
The hemorrhagic period is characterized by rupture of pathologically thinned vessels and is clinically manifested by the syndrome of subarachnoid, intracerebral or mixed hemorrhage. It should be noted that with arteriovenous malformation, hemorrhages occur earlier (at the age of 20-30 years) than with saccular aneurysms (at 35-50 years), and repeated bleeding in the early stages after the first rupture of the aneurysm is much less common.
The posthemorrhagic period proceeds relatively favorably. Quite often, after the first hemorrhage, clinical recovery occurs; relapses of hemorrhage are observed after a long time and have a more benign course; Deaths due to relapses are relatively rare. Sometimes patients complain of pulsating noise in the head, exophthalmos, pulsation of the jugular veins, expansion of the saphenous veins of the head are possible, and the level of intelligence often decreases.
Symptoms
The first signs of vascular damage to the brain may appear already at a young, working age. In this case, patients tend to ignore painful symptoms and not consult a doctor. And even when visiting a therapist or neurologist, the condition often remains unrecognized.
Among the early signs:
- absentmindedness;
- memory loss;
- fatigue;
- decreased performance;
- headache;
- noise in the head;
- episodes of dizziness;
- weather sensitivity.
Signs of circulatory problems may appear one by one. Young patients often associate them with overwork, as they believe that it is too early for them to be sick.
Over time, negative lifestyle factors lead to a deterioration of the condition - normal activities begin to suffer, severe weather sensitivity worries, and a person’s character “deteriorates.”
But sometimes the situation changes dramatically. In such cases, they speak of acute cerebrovascular accidents. How to recognize typical vascular diseases?
Encephalopathy
This diagnosis has already become “the talk of the town”: it is used to scare patients with hypertension, and it is “gifted” to old women who make scandals in pharmacies, clinics and on the street. And no wonder. The first symptoms of the disease are often noticeable behavioral, emotional and volitional disturbances. Thus, patients experience:
- irritability;
- emotional lability;
- sleep disorders;
- fatigue;
- depressive symptoms.
Relatives may notice that such a relative has become angry, sensitive to changes in weather, and his personality traits have become “sharpened.” Sentimental people become whiny, punctual people become pedantic, thrifty people become frankly stingy.
Over time, productivity begins to suffer: memory and attention deteriorate. The person becomes absent-minded, “constantly writes down so as not to forget,” but still forgets. Episodes of inappropriate, rude behavior are possible.
Discirculatory encephalopathy progresses, the course can be uniform or with sudden episodes of deterioration. It cannot be cured, you can only slow down the development of the disease. Severe encephalopathy is characterized by the development of dementia. Such a patient has completely lost self-care skills, in some cases cannot control physiological functions, and needs constant care and supervision.
Osteochondrosis often provokes or intensifies the manifestations of encephalopathy, as it impairs blood flow to the brain due to narrowing of the lumen of the vertebral arteries. Slow personality changes due to vascular damage also occur in systemic diseases accompanied by vasculitis.
Stroke
Stroke is one of the most common causes of death in people around the world. In fact, this is an acute circulatory disorder in the cerebral vessels, in which the entire brain lesion dies. According to the mechanism of development, there are 2 types of strokes: ischemic and hemorrhagic.
In ischemic stroke, the lumen of the vessel is blocked. Brain cells are very sensitive to hypoxia. At first, they try to provide for themselves through anaerobic glycolysis; within a few hours, the pathological processes are reversible. But decay products gradually accumulate, and the pH of the tissue changes to the acidic side. Neurons swell, their membranes cease to perform their functions and are destroyed. The final formation of the stroke focus occurs within 2-7 days; specialist assistance is most effective during the first 3-6 hours.
With a hemorrhagic stroke, the integrity of the vessel is compromised. Blood pours under the membranes, into the parenchyma (tissue) of the brain, and breaks into the ventricles. The cause of such a catastrophe is changes in the structure of the vascular wall and fluctuations in blood pressure. Congenital or acquired cerebral aneurysm can cause sudden death or severe disability. Until it reaches a large size, there is no pressure on the brain, and there are no clinical manifestations. The condition may worsen acutely, the patient is concerned about:
- headache;
- nausea;
- double vision;
- convulsions;
- disturbances of consciousness.
A special place is occupied by transient ischemic attacks, or as they say - micro-strokes. The name “microstroke” is unscientific; it reflects the reversibility of what occurs in the patient’s tissues. Some people who have had ischemic attacks are not aware of this. Thus, patients are greatly surprised to learn about them when describing a routine computed tomography or magnetic resonance imaging. (“I thought it was a simple hypertensive crisis!”)
Symptoms and prognosis for cerebrovascular accidents depend on the volume and location of the lesion. It is worth recalling obvious signs, the detection of which requires immediate medical attention:
- severe headaches, often with dizziness, tinnitus;
- asymmetry of the face, it is impossible to raise your hands, smile, show your teeth;
- weakness, numbness in the arms and legs, unsteadiness of gait;
- violation of pronunciation and perception of addressed speech;
- nausea and vomiting;
- disturbance, loss of consciousness.
Carotid-cavernous anastomosis
Among the various types of cerebral vascular pathology, carotid-cavernous (carotid-cavernous) connections (ostia) are often found, which are formed as a result of damage to the internal carotid artery in the place where it passes through the cavernous sinus.
Damage to the artery can be caused by traumatic brain injury. Much less often, such compounds arise spontaneously, as a result of an infectious process, atherosclerosis, or vascular abnormalities. Violation of the integrity of the artery occurs in the places of its branches or in the places of attachment of connective tissue strands to it. Blood under high pressure enters the cavernous sinus and further through the veins flowing into the sinus - against the flow of venous blood. Over time, blood circulation shifts more and more towards the pathological connection. Through the veins flowing into the sinus, a retrograde flow of arterial blood occurs into the corresponding veins of the eye. The venous outflow is disrupted, and stagnation forms in the orbit. The sinus itself noticeably stretches and increases in size, the cranial nerves (III, IV, VI and the first branch of the V (trigeminal nerve) pairs passing through it) are compressed.
The carotid-cavernous junction is characterized by headache, dizziness, synchronous pulse noise in the head, often reminiscent of the noise of a train, which is difficult for patients to tolerate. The murmur is heard over the orbit, temporal area and mastoid process. It disappears when the carotid artery is compressed in the neck on the affected side. There are pulsating exophthalmos, which is quite well defined by palpation of the eyeball, and pronounced dilatation of the veins in the forehead and eyelids. Intraocular pressure increases, sometimes acute glaucoma develops, which can lead to decreased visual acuity and blindness. Due to damage to the oculomotor nerves, the range of movements of the eyeball decreases. Cerebrovascular accidents often lead to decreased memory, work ability, and even mental disorders.
Due to increased pressure in the veins flowing into the cavernous sinus, bleeding from the vessels of the eyeball and nose may occur. An ophthalmoscopic examination reveals dilation of the retinal veins, often their pronounced pulsation, and in some cases, swelling of the optic discs and even hemorrhages in the fundus.
Causes of pathology
Vascular diseases of the brain can occur for a number of reasons. As a rule, several reasons lead to the appearance of pathology. The most common ones include:
● genetic predisposition;
● narrowing and hardening of intracerebral arteries (with hypertension);
● multiple focal and/or diffuse brain lesions;
● long-term somatic diseases of the expectant mother (and during pregnancy);
● atherosclerosis of cerebral vessels;
● rheumatic lesions;
● disturbances in the functioning of the respiratory system (for example, pulmonary edema);
● abuse of alcohol and tobacco products during pregnancy;
● disturbances in metabolic processes;
● increased blood viscosity;
● fractures of the skull bones;
● heart rhythm disturbance (with atrial fibrillation, blood hemodynamics are disrupted);
● serious abnormalities in the nervous system (increased anxiety, chronic stress);
● serious abnormalities of the endocrine system (diabetes mellitus, obesity);
● development of intrauterine infections;
● difficult long labor (with injuries);
● hypertension;
● hypercholesterolemia;
● various anomalies of the cardiovascular system (for example, hypoplasia of cerebral vessels, mitral valve prolapse).
Diagnostics
Accurate and objective diagnostic information plays an important role in choosing a treatment method, especially surgical, the place and time of its implementation. The therapeutic and diagnostic capabilities of modern neurosurgery are increasing rapidly thanks to new diagnostic equipment. At the same time, traditional diagnostic methods also remain relevant.
Diagnostic lumbar puncture is an informative method for determining subarachnoid hemorrhage, which often occurs when an intracranial aneurysm ruptures. Using echoencephalography (EchoEG), when an aneurysm ruptures with the formation of a hematoma, the side of its location is specified based on the pronounced (more than 4-6 mm) displacement of the M-echo.
Doppler ultrasound allows you to non-invasively determine the linear speed and direction of blood flow, the degree and level of circulatory disorders in the main arteries. Duplex (double) ultrasound scanning makes it possible to simultaneously determine changes in blood flow and obtain an image of the vessel itself, identify carotid artery stenosis (less than 50%), as well as the location and structure of the atherosclerotic plaque.
Changes in cerebral blood flow and cerebral vascular tone can be judged from the data of rheoencephalography, impedance rheoplethysmography and telethermography.
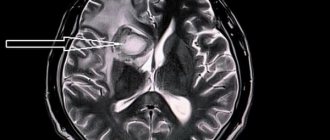
The study of regional cerebral blood flow using the clearance of a radioactive isotope (rXe) allows us to determine the degree of reduction in cerebral circulation. Computed tomography (CT) allows one to differentiate focal cerebral ischemia from hemorrhage. The size and location of the intracranial hematoma and the focus of cerebral infarction, as well as the state of the surrounding brain space, are clearly determined. Magnetic resonance imaging (MRI) makes it possible, even without the use of a contrast agent, to evaluate not only anatomical structures, but also the level of energy, enzymatic and metabolic processes in the brain. Non-invasive nuclear magnetic resonance angiography has even greater diagnostic capabilities, which allows you to obtain angiograms in any projection and identify not only aneurysms, but also atherosclerotic plaques in the arteries.
Recently, nuclear magnetic resonance spectroscopy has been used, which makes it possible to draw conclusions about the dynamics of focal brain lesions both in areas of irreversible changes and in the “ischemic penumbra” zone.
Treatment in each case is selected individually, depending on the cause and location of the damage.
Diagnosis of pathology
If the symptoms described above appear, it is recommended to immediately consult a cardiologist or neurologist. During the initial examination, the specialist collects an anamnesis of the patient’s life, asks in detail about his complaints (how long ago and under what circumstances they appeared), about diseases of the cardiovascular system of his closest relatives. Based on these data, further examination is prescribed.
To diagnose vascular diseases of the brain, they resort to laboratory and instrumental diagnostics. First of all, the patient is prescribed a general and biochemical blood test to determine the level of cholesterol, glucose, triglycerides, lipoproteins and prothrombin index (PTI). These substances affect the functioning of the heart and blood vessels. Biochemical indicators are very important in making a diagnosis. An increased level of leukocytes indicates the presence of an inflammatory process in the body. Among the instrumental diagnostic methods, the following are in particular demand:
● electrocardiography (ECG). This is a simple technique that does not require additional preparation. The essence of an ECG is to record the electrical potentials of the heart, due to which it is possible to detect changes in rhythm, electrolyte deficiency and other initial signs of cardiovascular pathologies;
● Doppler ultrasound of the vessels of the neck and brain (USDG). This is a modern, highly informative diagnostic method. It is used to determine damage to the arteries and indicates insufficient blood supply to the brain. With its help, it is possible to assess blood flow in the vessels of the neck and head;
● duplex scanning of blood vessels. Thanks to color contrast of flows during duplex scanning, it is possible to more clearly distinguish between moving and stationary objects (blood and vessels, respectively);
● ultrasound examination of the heart (ultrasound). This technique makes it possible to visually view the contractions of the heart muscle, assess the condition of its valves, and diagnose heart failure;
● echocardiography (EchoCG). Sometimes specialists prescribe echocardiography in addition to an ECG. This is a highly accurate examination method, with its help it is possible to assess the condition and determine the size of the valves;
vascular magnetic resonance imaging (MRI). This is a completely safe technique for the body (there is no radiation), it shows the lumen and patency of large vessels, and makes it possible to detect abnormalities in vascular development.
Treatment
The basis of treatment for this pathology is lifestyle adjustments. This means:
- lipid-restricted diet,
- rejection of bad habits,
- physical activity regimen,
- avoiding stress,
- treatment of chronic diseases.
The focus of drug therapy is the use of lipid-lowering drugs, antiplatelet, antihypertensive and antioxidant drugs, drugs to improve microcirculation and symptomatic therapy. Therapy, as a rule, takes a very long time and depends on the stage at which it was started.
In case of severe stenotic processes, surgical treatment is recommended for the patient. Most often, surgical intervention is performed on the internal carotid arteries. Source: E.A. Shirokov. Stenosing atherosclerosis of the cerebral arteries: modern strategies for diagnosing and treating patients // Consilium Medicum, vol. 18, no. 9, 2021, pp. 37-42.
Treatment for this disease is aimed at ensuring that metabolic processes are restored, and harmful cholesterol no longer settles on the walls of blood vessels. At the same time, attention is also paid to restoring blood circulation and normalizing the nutrition of brain tissue.
Drug therapy
This is the most important part of the comprehensive treatment of atherosclerosis. Patients may be prescribed several groups of medications:
- Statins - reduce the size of cholesterol plaques, reduce the risk of narrowing of the main arteries of the brain, and stop the growth of plaques.
- Antiplatelet agents – reduce blood viscosity and prevent blood clots.
- Fibrates are similar in action to statins, but do not affect the size of plaques, but lower the triglyceride content in the blood.
- Means for restoring vascular function.
- Bile acid sequestrants prevent cholesterol from being absorbed from food.
- Nootropics and medications that improve metabolic processes in nervous tissue.
- Hypotensives that stabilize blood pressure and help prevent stroke.
- Vitamin and mineral complexes to improve the general condition of the body. They must contain vitamins A, C, group B and nicotinic acid.
Medicines are taken in long courses, and most of them are taken for life with periodic dosage adjustments.
Surgical treatment
Operation is a last resort, indications for it:
- narrowing of the lumen of the carotid artery by 70% or more;
- condition after a minor stroke;
- recurrent ischemic attacks.
Surgical options:
- bypass - the formation of a vessel bypassing the one affected by cholesterol deposits;
- endarterectomy - a procedure to remove cholesterol plaques along with a small amount of tissue that lines the vessel from the inside;
- stenting using endoscopic technology - an expanding structure impregnated with a composition that dissolves cholesterol is installed in the vessel.
Operations can be performed under general anesthesia or local anesthesia. An anesthesiologist is consulted before the operation. The length of hospital stay varies depending on the technique, as do recommendations for the recovery period. SM-Clinic doctors inform patients in detail about all the nuances and are ready to answer any questions related to treatment at the initial consultation. Consultation on the operation is free of charge.
You can find out more about discounts on preoperative examinations by following the link.