Now this word is on everyone's lips. But what is the role of antibodies in protecting the body? Does an antibody test really eliminate all questions about whether you have been exposed to the virus? How accurate is it? Why might antibodies make the disease worse? Read in our analysis
Short
Antibodies are created by immune cells to fight a specific pest: virus, bacteria or parasite.
They do not appear immediately, because the body needs time to study the pest (pathogen).
The more antibodies, the stronger the protection. Over time, they may disappear, but cells are able to create them again when faced with a familiar danger.
There can be many antibody variants for one pathogen. Not everyone can “see” tests, so their accuracy is not absolute.
The virus can mutate, and then the old antibodies will not be able to recognize it. Or, having recognized it, they will not be able to neutralize it and themselves will become its conductors into the cells.
How are antibodies related to immunity?
This is one of its main tools in the fight against threats. Antibodies are not independent cells, but protein structures that are created by protective cells (lymphocytes) for a specific target. It happens that it turns out to be completely harmless substances - for example, pollen or chicken egg whites. This is how an allergic reaction occurs. But most often, antibodies fight viruses, bacteria, parasites and other “saboteurs”.
Antibodies can also be produced against the body’s own cells—they are called autoimmune. Each cell of the body has special protein molecules - identification marks that say that it is “our own”. But if the cell has grown old, died or degenerated into a malignant one, an “order” for destruction is also sent against it.
General information
IgG makes up up to 80% of all immunoglobulins contained in serum, and up to 20% of its total proteins. They produce IgG plasma cells (mature B lymphocytes).
Class G immunoglobulins provide the body's secondary humoral response to infection. That is, first, class M immunoglobulins (“alarm antibodies”) are produced in response to foreign cells in the body, and only after 5 days do G antibodies (IgG) appear. Their half-life is 23-25 days. This means that throughout this time the body is actively “fighting” the disease, as a result of which its resistance to the disease increases.
That is, antibodies destroy viruses and bacteria?
Not really. The purpose of antibodies is to neutralize the “intruder” so that it cannot reproduce, or to mark it for destruction. For example, they stick to viral particles, preventing them from entering the cell. Since the virus is unable to reproduce outside cells, it dies. Antibodies can also clump bacteria together into clumps, which are then devoured by phagocytes, or activate a system of immune proteins that will break through the bacterial membrane and kill it.
An antibody works like a molecular master key: it is born already tailored to a certain structural feature of a foreign body. For example, this could be a site (spike) on the surface of a viral particle through which it binds to a cell. The antibody blocks the spike and the virus cannot infect the cell. Related viruses may have similar structural elements, and then antibodies to one member of the family will be effective against another. For example, some people who have had SARS in the past (caused by the SARS-CoV-1 virus) already have effective antibodies against its relative, SARS-CoV-2, which causes COVID-19 infection.
Why are antibodies not immediately formed during illness?
To create the right antibody, the immune system first needs to study the offender. To achieve this, different “departments” cooperate in the body. First, interceptor cells (macrophages) absorb and digest foreign particles. Then they are introduced to their structure of “laboratory” cells (B-lymphocytes). They, in turn, form many copies of themselves with different variants. The “memory” of immunity is not based on antibodies alone. Cells also have it. Lymphocytes that produce antibodies remain dormant until they encounter the pest again. At the right moment, they can quickly create new “shells”. True, such preparation also has a downside, which prevents the creation of effective vaccines against some viruses.
When faced with a familiar virus, the body first throws into battle the cells that were trained to attack it. He suspends the development of new antibodies to save energy. But the virus can mutate in such a way that its vulnerabilities are protected, and the immune system does not recognize this. Even worse: the virus can use the antibody attached to it to enter an immune cell and infect it.
Reduced IgG
Deficiency of this class of antibodies is detected in the following cases:
- viral diseases in chronic form;
- allergic diseases, including atopic dermatitis;
- deficiency of vitamin B12 in the body;
- chronic inflammatory processes in the large intestine (ulcerative colitis, Crohn's disease);
- human immunodeficiency virus (HIV infection);
- nephrotic syndrome (damage to the glomeruli of the kidneys);
- leukemia (blood cancer);
- surgery to remove the spleen (splenectomy);
- general variable immunodeficiency (a disease in which there is a violation of the production of immunoglobulins);
- Bruton's disease (immunodeficiency due to gene mutation). In this case, there is a congenital deficiency of immunoglobulin G;
- hypogammaglobulinemia (B-lymphocyte deficiency);
- hyper-IgM syndrome (immunoglobulin deficiency caused by a hereditary disorder of the immune system);
- Louis-Bar syndrome (immune T-cell deficiency);
- Wiskott-Aldrich syndrome (a genetically determined recessive disease characterized by the presence of eczema);
- exposure of the patient to ionizing radiation;
- muscular dystrophy (genetic).
How is an antibody test done?
To detect antibodies, tests use antigens - areas on the surface of the virus to which these same antibodies bind. They are fixed in the wells of special tablets, or dies, and the patient’s blood is added to the wells. Staining then reveals the antibodies that would have attached to the antigens. If the sample changes color, this should mean that antibodies are present.
Rapid antibody tests are typically used to provide a simple yes/no result. They have two lines, like a pregnancy test. There are also those who look separately for proteins of classes M (which are formed during illness) and G (which remain in the blood after recovery). In this case, there are already three stripes in the test.
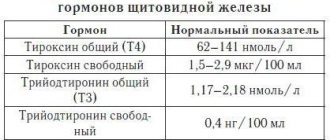
There are also quantitative tests. They already make it possible to determine not only the presence of antibodies, but also their concentration. It can be used to judge both the state of the immune system and the stage of the infectious process: is it in an acute form or is it heading towards recovery. To conduct quantitative tests, developers build on the established antibody norm, which corresponds to different stages.
Interpretation of antibody test results
Only a doctor can correctly interpret the results of an immunoglobulin test. It takes into account not only the indicators in the study form, but also the patient’s condition, the presence or absence of symptoms of the disease, and data from other studies.
Each laboratory uses its own test systems, therefore the results of tests carried out in different diagnostic centers may vary. The limits indicated below are indicative.
IgA
Total IgA standards for children:
- up to three months - from 0.01 to 0.34 g/l;
- from three months to a year - from 0.08 to 0.91 g/l;
- from one to 12 years:
- for girls - from 0.21 to 2.82 g/l;
- for boys - from 0.21 to 2.91 g/l.
Standards for immunoglobulin A levels for women:
- 12–60 years – from 0.65 to 4.21 g/l;
- over 60 years old - from 0.69 to 5.17 g/l.
Class A antibody concentration standards for men:
- 12–60 years old - from 0.63 to 4.84 g/l;
- over 60 years old - from 1.01 to 6.45 g/l.
The content of IgA in the blood increases during acute and chronic bacterial, including parasitic, infections, malignant neoplasms, lymphomas, systemic connective tissue diseases, cystic fibrosis, liver damage and other rarer pathologies. Also, antibodies of this type can be actively produced in autoimmune diseases.
A decrease in the concentration of antibodies occurs in atopic dermatitis, some diseases of the blood and lymphatic system, including congenital and acquired immunodeficiency conditions. And also in case of disruption of the synthesis of protein molecules, their excessive loss in the urine in kidney diseases and while taking certain medications.
IgM
The IgM content in the blood serum of newborns should be in the range of 0.06–0.21 g/l.
For children:
- from three months to a year:
- for girls - from 0.17 to 1.50 g/l;
- for boys - from 0.17 to 1.43 g/l;
- from one to 12 years:
- for girls - from 0.47 to 2.40 g/l;
- for boys - from 0.41 to 1.83 g/l.
For women - from 0.33 to 2.93 g/l.
For men - from 0.22 to 2.40 g/l.
IgM increases with inflammation, pneumonia, sinusitis, bronchitis, intestinal and stomach diseases and other infections in the acute stage. If the concentration indicator goes beyond the upper limit of normal, this may indicate liver damage, parasitic diseases, autoimmune pathologies, cystic fibrosis, as well as myeloma and lymphocytic leukemia. A decrease in IgM levels is observed with disorders of protein synthesis or damage to the immune system. This often happens after removal of the spleen, significant loss of protein in the urine, during treatment with cytostatics and other drugs that suppress the immune system, with lymphoma, as well as with some congenital immunodeficiency conditions.
IgG
Unlike previous immunoglobulins, IgG levels fluctuate less throughout life.
For women, its norms are:
- at the age of up to a month - from 3.91 to 17.37 g/l;
- from a month to a year - from 2.03 to 9.34 g/l;
- at the age of one or two years - from 4.83 to 12.26 g/l;
- after two years - from 5.52 to 16.31 g/l.
For the strong half of humanity:
- at the age of up to a month - from 3.97 to 17.65 g/l;
- from a month to a year - from 2.05 to 9.48 g/l;
- at the age of one or two years - from 4.75 to 12.10 g/l;
- after two years - from 5.40 to 16.31 g/l.
IgG concentrations may increase in chronic infections, autoimmune diseases, parasitic diseases, sarcoidosis, cystic fibrosis, liver damage, myeloma, chronic lymphomas and lymphocytic leukemia, infectious mononucleosis and granulomatosis. Also, the content of antibodies of this class usually increases with multiple sclerosis, neurosyphilis and AIDS.
The level of IgG may decrease with oncology of the hematopoietic and lymphatic systems, with muscular dystrophy and some other diseases.
But, for example, with HIV infection, the level of IgG can be both extremely high and extremely low - it all depends on the stage of the disease and the state of the immune system.
It is important
To determine the amount of antibodies to COVID-19, you can also take an immunofluorescence test. In this case, the test will show the presence of immunoglobulins M and G. And if, for example, the level of IgM is below 1 g/l, and IgG - up to 10 g/l, then this means that the person has not encountered the virus. And in the case when the content of class M antibodies is below 2 g/l, and class G is higher (or equal) to 10 g/l, it can be assumed that the subject has had a coronavirus infection[1].
Rh antibodies
With the indicators of antibodies to the Rh factor, everything is a little simpler. Normally they should not exist[2]. If antibodies are detected, it means that immunization occurred during a previous pregnancy or through a transfusion of donor Rh-positive blood.
Autoantibodies
These antibodies are also absent in the blood of a healthy person. Their presence indicates the development of autoimmune diseases, when the immune system attacks its own tissues, most often connective, muscle, cartilage, serous, and vascular walls. Thus, the level of these immunoglobulins can increase in rheumatoid arthritis, multiple sclerosis, vasculitis, type 1 diabetes mellitus, scleroderma, systemic lupus erythematosus, psoriasis and others.
Should you always trust test results?
The result largely depends on the set of antigens that the developers used. If the selected antigens are not specific enough, proteins produced in response to other pathogens, such as related coronaviruses that cause the common cold, will latch on to them. In this case, the test gives a false positive result.
There are also false negative results - when a person has antibodies to an antigen that is not presented in the test. For example, this happens with viruses that have been discovered recently, as in the case of SARS-CoV-2. A false negative result can also occur when the blood was taken too early and there are not enough antibodies in it yet.
How to choose a quality antibody test?
Look at the sensitivity and specificity rates. Sensitivity is the agreement between positive test results and actual diagnoses. Specificity is the ability of a test to detect exactly those antibodies that relate to a specific pathogen. A test that is not sensitive enough may miss some cases, while a test that is not specific enough may suspect the virus in those who do not have it.
According to the results of a recent meta-analysis, the ELISA test, an enzyme-linked immunosorbent test, turned out to be the most reliable in determining antibodies to SARS-CoV-2. Its specificity is 99% and sensitivity is 90–94%. It is done in a laboratory and takes one to two days. The ICA (immunochromatographic) rapid test is less accurate, but it takes about ten minutes. Sensitivity/specificity may be different for different types of antibodies.
It is important to remember that the antibody test does not show the presence of the virus, but only the body’s possible reaction to it. The WHO (World Health Organization) considers the PCR test to be the most accurate and reliable method for diagnosing a viral infection. It allows you to detect the presence of genetic material of the virus in the blood. Remember that in making a final diagnosis, it is not the test that is decisive, but the clinical picture.
Immunoglobulin G antibodies are elevated
Antibodies during HIV infection in the blood of a sick person can be increased or greatly decreased, and a state of severe immunodeficiency develops. Malignant tumors in the patient's body also lead to a state of immunodeficiency or hyperimmunoglobulinemia. Immunoglobulin G is significantly elevated in autoimmune diseases. Immunoglobulin is responsible for the body’s memory of past diseases: chickenpox, cytomegalovirus, measles, rubella, Epstein-Barr virus and other types of infection.
An increase in the level of immunoglobulin G in the blood indicates the development of an acute or exacerbation of a chronic infectious process in the body. Immunoglobulin G is elevated in the following pathological processes:
- for scarlet fever, diphtheria, whooping cough;
- during chickenpox, measles, rubella;
- for influenza, pneumonia, acute bronchitis;
- for tuberculosis, mononucleosis;
- with hepatitis, cirrhosis of the liver;
- for rheumatoid arthritis, lupus erythematosus, rheumatic fever;
- when infected with worms;
- with the development of a severe allergic reaction;
- with the development of malignant tumors, AIDS, HIV and other diseases.