What is pancytopenia?
Pancytopenia is a descriptive term for a combination of low levels of all types of blood cells, including red blood cells (anemia), white blood cells (leukopenia), and platelets (thrombocytopenia). Often, symptoms such as fatigue, infections and bruising occur as a result of decreased levels of these cells.
There are a number of different conditions that can cause pancytopenia, including bone marrow diseases, some types of cancer, and some infectious diseases. Medical conditions such as chemotherapy can also cause pancytopenia.
Treatment options for pancytopenia depend on the specific cause and typically focus on increasing cell levels to improve symptoms while treating the underlying cause.
Symptoms of pancytopenia - deficiency of morphotic blood elements
There are three main groups of blood cells in the blood: red blood cells, which deliver oxygen to all tissues, white blood cells, which fight infection and form our protective barrier, and platelets, which are responsible for stopping bleeding and closing wounds.
Symptoms of pancytopenia occur due to too few of these cells and hence their dysfunction. Due to the complex nature of this disease, a range of symptoms may be experienced and may vary in severity.
About
Blood cells affected by pancytopenia
Specifically, pancytopenia refers to a deficiency of:
- Red blood cells (erythrocytes): Red blood cells are cells that bind and carry oxygen to body tissues.
- White blood cells (leukocytes). There are several types of white blood cells, which are further broken down into granulocytes (including neutrophils, eosinophils and basophils) and agranulocytes (including lymphocytes and monocytes). These cells are responsible for fighting infections among other functions.
- Platelets: Platelets are responsible for blood clotting.
Description of Low Blood Cell Count
These terms are used for lower levels of blood cells:
- A low level of red blood cells is called anemia. It is important to note that there are different forms of anemia. One form is low red blood cell count, but it can also be due to blood loss, low hemoglobin levels, vitamin B12 deficiency, and other causes.
- Low levels of white blood cells are referred to as leukopenia (you may also have heard of neutropenia, which refers to low levels of a certain type of white blood cell known as neutrophils).
- Low platelet levels are called thrombocytopenia, and there is immune thrombocytopenia or chemotherapy-induced thrombocytopenia.
Pancytopenia and blood cell deficiency
Red blood cells have a longer lifespan (approximately 120 days) compared to other blood cells, so we can say that there are “more” of them in the body. For this reason, symptoms of red blood cell deficiency (anemia) appear no later than before and often go unnoticed.
On the other hand, platelets, which are really just fragments of cells, are the least durable. Low platelet levels occur most quickly, so symptoms of thrombocytopenia appear early and can be dangerous. The most serious of these include bleeding of the retina and brain, which can lead to permanent blindness or death.
As the disease progresses, the white blood cell count begins to decline slightly later than the platelet count, leading to recurring and difficult-to-treat infections. At first these are common colds, but over time they can develop into severe systemic infections. Patients with bone marrow damage should be especially careful with the medications they take (even over-the-counter medications) because many medications used to treat even mild infections can worsen pancytopenia due to their harmful effects on the bone marrow.
Lab tests
Pancytopenia is usually diagnosed by a complete blood count (CBC).
In pancytopenia, the CBC will show insufficient levels of all types of blood cells, including:
- The red blood cell count is less than 4.2 million cells per cc in women or less than 4.7 million cells per cc in men (this may also be described by low hemoglobin levels).
- The leukocyte count is less than 4,000 leukocytes per cubic cm (normally, a person has from 4,000 to 10,000 leukocytes per cubic cm).
- Platelet count is less than 150,000 cells per cubic cm (normally from 150,000 to 400,000 cells per cubic cm).
Causes of pancytopenia
Pancytopenia can be caused by anything that prevents blood cells from being made in the bone marrow or from appearing in the bloodstream (for example, if they are retained by the spleen).
This may include destruction of the bone marrow by toxins, suppression of the bone marrow, such as during chemotherapy, or the replacement of bone marrow cells with others that interfere with the production of blood cells, during treatment for certain cancers. Destruction or suppression can occur as a result of inflammation, infection or autoimmune diseases.
Most of these conditions are acquired later in life, but some are inherited and passed on from birth. In at least 50 percent of cases, there is no obvious cause—what doctors call an “idiopathic” cause. Some of the possible causes of pancytopenia may be:
- chemotherapy caused by bone marrow suppression;
- induced drugs: drugs other than chemotherapy have been cited as causes, ranging from antibiotics to drugs used for cardiovascular disease;
- infections such as infectious mononucleosis and HIV, as well as suppressive infections (sepsis);
- aplastic anemia;
- splenic sequestration (holding of blood cells by the spleen so they can travel to the rest of the body);
- toxins and chemical exposures, such as exposure to arsenic or benzene;
- blood cancer in the bone marrow, such as leukemia, lymphoma, myeloma, or metastatic bone marrow cancer;
- metastasis of some solid tumors to the bone marrow, especially breast cancer, prostate cancer, colon cancer, gastric cancer and melanoma. In bone marrow metastases, the most common symptom is anemia followed by thrombocytopenia;
- myelodysplastic syndromes of “precancerous” conditions of the bone marrow;
- autoimmune disorders such as lupus erythematosus;
- radiation sickness;
- hereditary syndromes such as Fanconi anemia and Diamond-Blackfan anemia.
Most common reasons
A 2014 study aimed to determine the most common causes of pancytopenia in people who had not yet been diagnosed with the disease. For example, none of these adults had received chemotherapy or had an obvious cause of pancytopenia. Of these people:
- more than 60 percent had some type of blood cancer. The most common were acute myeloid leukemia, myelodysplasia, non-Hodgkin's lymphoma, hairy cell leukemia, and acute lymphocytic leukemia;
- among those whose blood cancer was not associated with a cause of pancytopenia, diagnoses included aplastic anemia, pernicious anemia, and HIV.
Thrombocytopenia
Thrombocytopenia - what is it?
We will talk about a violation of hemostasis, more precisely, its platelet component, which is characterized by the fact that the number of platelets per unit volume of blood decreases.
Occurs:
- High bleeding from the skin and mucous membranes;
- Bruises and hemorrhagic rashes form;
- Bleeding.
In order to eliminate the problem, it is necessary to resort to drug therapy, splenectomy, and extracorporeal blood purification.
Why do pathologies appear?
All causes of pathologies are divided into two groups:
- Congenital;
- Purchased.
If the pathology is congenital, then it is part of hereditary syndromes, for example, Wiskot-Aldrich syndrome.
With the development of pathology in these cases, as a rule, qualitative changes in platelets also occur.
The causes of acquired pathology are quite diverse: lymphomas, sarcoidosis, portal hypertension, splenic tuberculosis, alcoholism, etc.
The most significant group includes pathologies caused by increased platelet destruction. Moreover, they develop both as a result of the mechanical destruction of platelets and the immune component.
- Alloimmune pathology is provoked by transfusion of blood of a different group;
- Transimmune pathology occurs due to the fact that maternal antibodies penetrate to the fetus through the placenta;
- Autoimmune pathology is a consequence of the production of antibodies to one’s own unchanged antigens;
- Heteroimmune pathology occurs due to the fact that antibodies act against foreign antigens that are fixed on the surface of platelets.
- Drug-induced pathology is a consequence of taking sedatives, antibacterial or sulfonamide drugs, and some others.
Note that a slight decrease in the number of platelets can be caused by vaccination or viral infections.
Pathologies that arise due to platelet deficiency develop when there is an insufficient number of stem cells, and thrombocytopenia occurs. This condition may be affected by:
- Aplastic anemia;
- Leukemia;
- Myelofibrosis;
- Presence of metastases in the bone marrow;
- Chemotherapy treatment, some other things.
There are indicators of the severity of thrombocytopenia:
- First stage (satisfactory hemostasis). With it, the platelet count is 150-50x109/l;
- Second stage (sharp decrease in indicator - 50-20 x109/l). This may be the result of a minor injury that causes intradermal hemorrhages or prolonged bleeding from wounds;
- Stage three (platelet count is minimal – 20x109/l). Spontaneous internal bleeding is to be expected here.
Below we will talk about thrombocytopenia, which manifests itself moderately, sharply and severely.
Causes of moderate thrombocytopenia
- Excessive alcohol consumption;
- Pregnancy period;
- Liver pathologies;
- Use of a number of medications;
- DIC syndrome;
- Lupus erythematosus and systemic vasculitis;
- Heart failure;
- Consequences of radiation therapy.
Causes of severe thrombocytopenia
- Systemic lupus erythematosus;
- Significant DIC syndrome;
- Acute leukemia;
- Hemolytic disease of the newborn.
Causes of severe thrombocytopenia
- Acute radiation sickness;
- Overdose of cytotoxic drugs;
- Severe course of acute leukemia.
Symptoms
The manifestations of thrombocytopenia depend entirely on the underlying disease, but it is worth talking about the general signs. Among them:
- Bruises appear inexplicably on the skin;
- The blood slowly stops at the cut sites;
- Often the nose bleeds;
- The oral mucosa bleeds;
- Increased risk of internal bleeding;
- There is a risk of cerebral hemorrhage.
As soon as general symptoms appear, you should consult a doctor. Thrombocytopenia is treated in most cases on an outpatient basis.
Stenosis
If the pathology is severe, the patient must be placed in an intensive care unit. The treatment strategy itself is determined by the underlying disease.
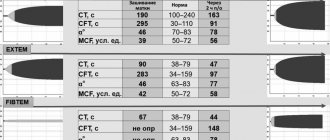
Diagnostic measures
Any increased bleeding is a reason to visit a hematologist. The doctor will prescribe the necessary tests. Among which:
- General blood analysis;
- Hemostasiogram;
- Ultrasonography;
- Radiography;
- Enzyme immunoassay blood test.
The latest tests are indicated if necessary, this is already decided by the doctor.
Pathology in cancer
Thrombocytopenia is very common in cancer patients. This is not by chance, of course, chemotherapy and radiation therapy cause its appearance. Some drugs have a detrimental effect on platelets.
On the other hand, the pathology can be caused by some types of cancer, for example, lymphoma.
If a patient develops a pathology in which the platelet level drops, the doctor is obliged to consider all possible causes, even those not related to cancer treatment.
Thrombocytopenia makes the condition of an oncology patient complex, which means that the doctor faces difficulties in treating him. He must keep in mind that:
- If platelet counts are low, chemotherapy and radiation therapy must be carried out very carefully, as the risk of bleeding increases;
- A decrease in the rate of <50x109 per liter leads to an increased risk of heavy bleeding during surgery;
- A decrease <10x109 per liter significantly increases the risk of spontaneous bleeding.
Treatment of thrombocytopenia in cancer patients
There are recognized methods of treating pathology in cancer patients. They boil down to the following:
- It is necessary to adjust the therapeutic program;
- If necessary, transfuse platelet mass to the patient when there is a risk of bleeding or before a course of chemotherapy;
- It is necessary to transfuse platelet mass under the close supervision of a hemotransfusiologist and a nurse.
There are simple recommendations on how to avoid bleeding:
- Using an electric razor instead of a razor;
- Avoiding injury;
- Using a toothbrush with soft bristles;
- Rejection of drugs that reduce blood clotting, etc.
The Onco.Rehab Integrative Oncology Clinic is glad to see its patients who are not burdened by pathologies and their complications. We fight for your health, so that your days are filled with the joy of life.
Symptoms and signs
Symptoms of pancytopenia may include a weak or enlarged spleen, in addition to symptoms and signs associated with a deficiency of specific blood cells. Some of these symptoms include:
- symptoms associated with anemia (low red blood cell count), including pallor, fatigue, fast heartbeat (tachycardia), and shortness of breath;
- symptoms associated with leukopenia or neutropenia (low white blood cell count), including fever and signs of infection such as cough or pain when urinating;
- symptoms associated with thrombocytopenia (low platelet levels), including easy bruising and heavy bleeding (see photo above).
Diagnostics
Pancytopenia can be detected by a complete blood count (CBC). The first step in assessing low levels of all cells is to repeat a complete blood count. A peripheral blood smear is then taken to further look at each of the different cell types.
If a repeat CBC confirms that you do have pancytopenia, the second step is to perform a bone marrow biopsy.
Bone marrow aspiration and biopsy examine components of the bone marrow, which include hematopoietic stem cells (cells that differentiate into all the different types of blood cells), blood cells at various stages of maturation, and materials used to make blood cells, such as iron and vitamin B12 .
In addition to testing the level of B12 in the blood, special tests and tests are done on the cells to look for changes such as chromosomal and genetic changes that are common in leukemia.
Diagnosis of pancytopenia – morphology and bone marrow biopsy
If pancytopenia is suspected due to alarming symptoms, the first test is a blood test.
According to the guidelines, a doctor may suspect pancytopenia if the number of red and white blood cells and platelets is below normal. As a result, low hemoglobin, low hematocrit, and granulocyte deficiency may occur.
If the suspicion of pancytopenia is confirmed, your doctor may order additional tests to determine the exact cause, ranging from more detailed blood tests to taking a bone marrow sample.
Bone marrow biopsy is usually performed to rule out neoplastic infiltration in patients in whom the cause of pancytopenia is difficult to determine.
Treatment of pancytopenia
The goal of treating pancytopenia is to identify and treat the underlying cause. If the cause is unknown or expected, such as with chemotherapy, treatment is aimed at minimizing symptoms associated with a blood cell deficiency. Some treatments that may be used include:
- Bone marrow stimulating drugs. For neutropenia caused by chemotherapy and some other causes, the growth factors Leukine, Neupogen or Neulasta can be used to stimulate the production of white blood cells. To treat anemia caused by chemotherapy, there are also some medications that can be used by doctors.
- Blood transfusions.
- Immunosuppressants if the condition is associated with an autoimmune disease.
- Bone marrow or stem cell transplant.