© Author: A. Olesya Valerievna, candidate of medical sciences, practicing pathologist, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Brain death means a complete and irreversible cessation of its vital activity, when the heart continues to beat and breathing is maintained through artificial ventilation (ALV).
Unfortunately, the number of patients who have irreversible events in the brain is large. Their treatment is carried out by resuscitation specialists, ensuring the maintenance of the main life support systems - breathing and circulation. From a medical and ethical point of view, it is always difficult to establish the fact of irreversibility of brain death, because this means declaring a person dead, although his heart continues to contract.
The brain lives after a person’s death for about five minutes, that is, after cardiac arrest, it is still able to maintain its activity for some time. During this period, it is very important to have time to carry out resuscitation, then there will be a chance for a full life. Otherwise, irreversible neuronal death will be fatal.
For relatives and friends, the issue of recognizing a sick relative as non-viable due to brain death is very difficult: many believe that a miracle will happen, others believe that doctors are not making enough efforts to “revive” the patient.
There are frequent cases of litigation and disputes when relatives consider the disconnection of the ventilator to be premature or erroneous. All these circumstances force us to objectify the data of symptoms, neurological and other types of examinations, so that an error is excluded, and the doctor who turned off the ventilator does not act as an executioner.
In Russia and most other countries, brain death is identified with the death of the whole organism, when maintaining the vital functions of other organs through medication and hardware treatment is impractical, which distinguishes brain death from a vegetative state and coma.
As already mentioned, under normal conditions, brain death occurs 5 minutes after breathing and heartbeat stop, but at low temperatures and various diseases this period can be lengthened or shortened. In addition, resuscitation measures and treatment can restore cardiac activity and provide ventilation of the lungs, but brain function cannot always be returned to its original state - comas, a vegetative state, or irreversible death of nervous tissue are possible, requiring different approaches from specialists.
Brain death established through clear criteria is the only reason when a doctor has the right to turn off all life support devices without the risk of being held legally liable. It is clear that such a formulation of the question requires compliance with all diagnostic algorithms for this condition, and an error is unacceptable.
Stages of diagnosing brain death
To accurately determine whether the brain is alive or whether irreversible and incompatible changes have already occurred in it, clear recommendations have been developed that should be followed by every specialist who encounters a patient in serious condition.
Diagnosis of brain death includes several stages:
- Accurate determination of the cause of the pathology.
- Exclusion of other brain changes that are clinically similar to his death, but under certain conditions can be reversible.
- Establishing the fact of cessation of activity of the entire brain, and not just its individual structures.
- Accurate determination of irreversibility of brain damage.
Based on clinical data, a doctor has the right to make a diagnosis of brain death without using additional instrumental diagnostic methods, since the developed criteria make it possible to determine the pathology with absolute accuracy. However, in our time, when the conclusion about any disease is based on a variety of objective results, instrumental and laboratory tests are involved in the diagnostic process.
brain perfusion on MRI is normal (left), with brain death (center), with a vegetative state (right)
Additional examinations are not excluded from diagnostic algorithms for brain death, but are not strictly required. Their purpose is to speed up the establishment of the fact of brain death, especially in clinically complex cases, although it is quite possible to do without them. In Russia, only electroencephalography and angiography of the carotid and vertebral arteries are allowed as the only reliable ones in determining signs of irreversibility of brain disorders.
Research on the effects of alcohol on brain activity
To prove that alcohol kills brain cells, scientists from Germany conducted an unusual experiment involving guinea pigs. Each animal was given a fairly large portion of ethyl alcohol (about the amount contained in 2 glasses of wine). As a result, the level of ethanol in the blood of guinea pigs increased by 0.05%.
Drunk test subjects were studied using magnetic resonance spectroscopy. It was found that within a few minutes after the introduction of alcohol, changes began in brain cells. The level of creatine, a compound that provides the organ with energy, decreased in neurons. Instead, alcohol molecules accumulated in the cells.
The researchers also noticed a decrease in choline in cell membranes. This substance is equivalent to vitamins. Without it, it is impossible for signals to pass through neuron fibers. With a lack of choline, mental activity immediately decreases. This negatively affects intellectual abilities.
Some people think that the experiment concerns only guinea pigs and has nothing to do with people. This is wrong. The brain of these animals works in a similar way to that of a human. This means that the frightening test results can be safely extrapolated to humans.
Features and criteria for declaring brain death
In medicine, the concepts of clinical and biological death refer to the entire body, implying the reversibility or irreversibility of changes occurring. Applying this parameter to nervous tissue, we can speak of clinical brain death in the first 5 minutes after breathing stops, although the death of cortical neurons begins already in the third minute. Biological death characterizes a total disorder of brain activity that cannot be reversed by any resuscitation or treatment.
The need to assess the state of the brain usually arises in comatose and similar conditions, when the patient is unconscious, contact with him is impossible, hemodynamics and heart function may be unstable, breathing is usually supported by a device, the pelvic organs are not controlled, there is no movement and sensitivity, reflexes and muscle tone fades away.
How long does the brain live after cardiac arrest?
Most studies have shown that the process of brain activity after the heartbeat stops is individual for each person. Although the cessation of oxygen flow is almost instantaneous, there is no specific duration of clinical death at which a functioning brain clearly dies. The most vulnerable cells are neurons, which suffer fatal damage in just 10 minutes without oxygen. However, the damaged cells do not actually die for a very long time. If resuscitation is successful, some areas may resume operations. Find out more. what happens to the brain at the moment of cardiac arrest can be found here - https://reactor.space/news/chto-proisxodit-s-mozgom-v-moment-ostanovki-serdca/.
Assessment of causes of brain death
A doctor has the right to begin diagnosing biological brain death only when the causative factors and mechanisms of changes in nervous tissue are precisely known. The causes of irreversible brain disorders can be primary, caused by direct damage to the organ, and secondary.
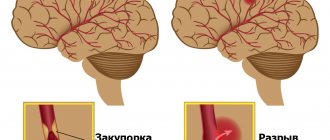
Primary brain damage leading to brain death is provoked by:
- Severe traumatic brain injuries;
- Hemorrhages, both traumatic and spontaneous;
- Cerebral infarctions of any nature (atherosclerosis, thromboembolism);
- Oncological diseases;
- Acute hydrocephalus, edema;
- Previous surgical operations inside the skull.
Secondary irreversible damage occurs due to pathology of other organs and systems - cardiac arrest, shock, severe hypoxia against the background of systemic circulatory disorders, severe infectious processes, etc.
An important diagnostic step is the exclusion of all other pathological conditions that could manifest symptoms similar to brain death, but which, nevertheless, are potentially reversible with proper treatment. Thus, the diagnosis of brain death should not even be assumed until a specialist makes sure that there are no influences such as:
- Intoxication, drug poisoning;
- Hypothermia;
- Hypovolemic shock due to blood loss, dehydration;
- Coma of any origin;
- The effect of muscle relaxants, anesthetics.
In other words, an indispensable condition when diagnosing brain death will be the search for evidence that the symptoms are not caused by drugs that depress the nervous tissue, poisoning, metabolic disorders, or infections. In case of intoxication, appropriate treatment is carried out, but until its signs are eliminated, a conclusion about brain death is not considered. If all possible causes for the lack of brain functioning are excluded, then the question of its death will be raised.
When monitoring patients with brain disorders potentially associated with other causes, the rectal temperature is determined, which should not be less than 32 C, the systolic blood pressure is not less than 90 mm Hg. Art., and if it is lower, vasopressors are administered intravenously to maintain hemodynamics.
Clinical data analysis
The next stage in diagnosing brain death, which begins after establishing the causes and excluding other pathologies, will be the assessment of clinical data - coma, absence of brainstem reflexes, inability to spontaneously breathe (apnea).
Coma is a complete absence of consciousness. According to modern concepts, it is always accompanied by total atony of the muscular system. In a coma, the patient does not react to external stimuli, does not feel pain, changes in the temperature of surrounding objects, or touch.
Brainstem reflexes are determined in all patients without exception with possible brain death, while the following signs are always taken into account to verify the diagnosis:
- There is no response to sufficiently intense pain effects in the areas of exit of the branches of the trigeminal nerve or the absence of other reflexes, the arcs of which close above the cervical part of the spinal cord;
- The eyes do not move, the pupils do not react to a light stimulus (when it is clearly established that there is no effect of medications that dilate them);
- Corneal, oculovestibular, tracheal, pharyngeal and oculocephalic reflexes are not detected.
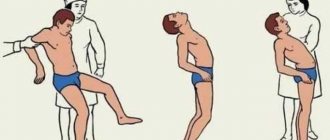
The absence of oculocephalic reflexes is determined by turning the patient's head to the sides with raised eyelids: if the eyes remain motionless, then there are no reflexes. This symptom is not assessed for cervical spine injuries.
checking oculocephalic reflexes
connection of oculocephalic and oculovestibular reflexes with brain stem vitality
To determine oculovestibular reflexes, the patient's head is raised, and cold water is pumped into the ear canals using a thin catheter. If the brain stem is active, the eyeballs will deviate to the sides. This symptom is not indicative of injury to the eardrums with a violation of their integrity. Pharyngeal and tracheal reflexes are checked by displacing the endotracheal tube or inserting a bronchial suction catheter.
One of the most important diagnostic criteria for brain death is the inability to breathe independently (apnea). This indicator is the final one at the stage of clinical assessment of brain functioning and can be determined only after checking all of the above parameters.
To determine whether a patient is able to breathe on his own or not, it is unacceptable to simply disconnect him from the ventilator equipment, since sudden hypoxia will have a detrimental effect on the already suffering brain and myocardium. Disconnection from the equipment is carried out on the basis of an apneic oxygenation test.
An apneic test involves monitoring the gas composition of the blood (the concentration of oxygen and carbon dioxide in it), for which a catheter is installed in the peripheral arteries. Before disconnecting the ventilator, ventilation of the lungs is carried out for a quarter of an hour under conditions of normal CO2 content and high oxygen pressure. After these two rules are observed, the ventilator is turned off, and humidified 100% oxygen is supplied to the trachea through the endotracheal tube.
If spontaneous breathing is possible, then an increase in the level of carbon dioxide in the blood will lead to activation of the stem nerve centers and the appearance of spontaneous respiratory movements. The presence of even minimal breathing serves as a reason to exclude brain death and immediately return to artificial ventilation of the respiratory system. A positive test result, that is, absence of breathing, will indicate irreversible death of the brain stem structures.
At all times, states that border between being and non-being are of great interest - lethargy, some amazing “coma-like” stages of self-hypnosis of Indian yogis, etc. What is human death, when and how does it occur and, most importantly, is the doctor always right when declaring the death of a patient?
In the mid-50s of the twentieth century there was a huge leap in resuscitation - synchronized artificial ventilation (ALV) and drugs to maintain blood pressure and cardiac activity appeared. In 1959, the so-called “exorbitant coma” (coma depasse) was described in 23 patients. With the heart beating and mechanical ventilation, a coma was observed without reactions to external stimuli, with total areflexia and an isoelectric electroencephalogram (EEG). All patients died within a short time [26].
The study of this condition began not only from a medical, but also from a philosophical and religious point of view. By 1968, it was accepted that in the case of isolated brain death, a person ceases to exist as an individual and this condition becomes the equivalent of human death. The first clinical signs of human death based on the diagnosis of brain death (BM) were published - the so-called Harvard criteria [11]. At the same time, the possibility of stopping further resuscitation and organ collection for subsequent transplantation in SM was postulated. By the beginning of the 80s, the first and so far only clinical multicenter study (The Collaborative Study of Cerebral Death) was completed and processed in the USA, which determined the main clinical and some instrumental signs of SM [13].
According to the international definition, SM is an iatrogenic condition characterized by complete and irreversible cessation of all brain functions during a beating heart and mechanical ventilation.
The results of modern research indicate that the pathogenesis of brain death is extremely complex and includes reversible and irreversible stages. Clinical signs of SM include lack of response to any sensory stimulation, absence of spontaneous breathing and any spontaneous motor phenomena, the occurrence of bilateral mydriasis with absence of pupillary response to light, and a rapid drop in blood pressure (BP) when cardiopulmonary bypass is stopped. However, it should be noted that in isolation, none of these clinical criteria is pathognomonic for SM. On the one hand, spinal reflexes can be detected some time after documented SM; on the other hand, all the signs that were considered undoubted symptoms of SM are in fact not such and do not always reflect the biological death of a person.
Thus, from the doctor’s perspective, the death of a person is not a cardiac arrest (it can be “started” again and again and maintained, saving the patient’s life), not a cessation of breathing (a quick transfer of the patient to a ventilator restores gas exchange), but a cessation of cerebral circulation. The vast majority of researchers around the world believe that if the death of a person as an individual, and not as an organism, is inextricably associated with brain death, then SM is practically equivalent to the cessation and non-resumption of cerebral perfusion. One of the pioneers of the study of SM, A. Walker, in the monograph “Brain Death” [10] gives the following definition: “Brain death is the complete and irreversible loss of all its functions, an iatrogenic condition that arose in connection with the development of methods for reviving and maintaining basic vital functions, characterized by a lack of blood flow into the vessels of the brain, i.e. a deceased individual with a beating heart and a ventilator.”
Mechanisms of development of brain death
The pathogenesis of SM development has been studied quite fully. Significant anatomical damage to the brain occurs with severe traumatic brain injury (TBI), as well as as a result of hemorrhage into the substance of the brain or under the meninges. The period of apnea, which almost always accompanies severe injuries or acute vascular events, also contributes.
Complete failure of arterial oxygenated blood to enter the cranial cavity within 30 minutes leads to irreversible damage to neurons, the restoration of which becomes impossible [10]. This situation occurs when there is a sharp increase in intracranial pressure to the level of systolic arterial pressure and when cardiac activity stops and inadequate chest compressions are performed during the above period of time. To understand the process of development of SM in the case of increased intracranial pressure (ICP) or transient anoxia, it is necessary to dwell in more detail on the formation and maintenance of intracranial homeostasis.
According to the Monroe-Kelly doctrine, formulated more than 200 years ago, there is a physiological system involved in maintaining equilibrium in the volume of intracranial contents.
The total volume of the contents of the skull can be expressed by the formula:
Vtotal=Vblood+Vcf+Vbrain+VH2O+Vx,
where Vtotal is the volume of the contents of the skull at the current time; Vblood - the volume of blood located in the intracerebral vessels and venous sinuses; Vcf—volume of cerebrospinal fluid (CSF); Vbrain is the volume of brain tissue; VH2O—volume of free and bound water; Vx is a pathological additional volume (tumor, hematoma, etc.), normally absent in the cranial cavity [26].
Normally, all these components are in dynamic equilibrium and create a constantly pulsating ICP of 8-10 mm Hg within insignificant limits. In a closed bone structure of the skull, the left side of the formula is a constant value, while the right components can change dynamically. Constant pulsatile changes in ICP can be measured using an invasive immersion method [23] or using echoencephaloscopy (Echo-ES) [6]. An increase in the volume of one of the variables in the right half of the formula leads to an inevitable decrease in the others. The volumes of water and CSF change most rapidly, and to a lesser extent - blood.
Gradually increasing changes in CSF volume and pressure may not be clinically manifested, and after reaching an individually defined critical point, clinical decompensation and a sharp increase in ICP occur. The mechanism for the development of dislocation syndrome as a result of the absorption of a large volume of CSF with an increase in ICP is described. Such a large amount of absorbed CSF causes difficulty in venous outflow due to compression of the venous collectors by brain matter, slowing down the evacuation of fluid from the cranial cavity, which leads to brain dislocation.
ICP can increase so much that it begins to exceed blood pressure. In such observations, a model of the so-called precerebral reverberant blood flow, pathognomonic for SM, is recorded. Blood from the heart enters the aorta, then into the common carotid arteries (CCA), slowing down, reaching the bifurcations, and then, being unable to “break through” into the brain through the internal carotid arteries (ICA), moves back and forth and/or partially discharged into the external carotid arteries (ECA). In other words, all internal organs continue to receive their portion of hemoglobin, and the brain is bleeding.
The process of progressive increase in ICP when blood flow is stopped was demonstrated in experiments on dogs back in the 80s [1]. The experimental part was carried out in the artificial heart laboratory of the All-Union Research Institute of Transplantology and Artificial Organs of the USSR on 10 dogs. The first group of animals (5 dogs) underwent cardiac arrest by applying a direct current voltage of 2 V, followed by restoration of its activity using a mechanical cardiac massager. The second group of animals (5 dogs) had their ICP increased until cerebral blood flow ceased, i.e. created an experimental model of SM.
Adult dogs weighing 10 to 15 kg were anesthetized by injecting a 5% sodium etaminal solution. To measure arterial and venous pressure, catheterization of the corresponding vessels was performed. CSF pressure was measured by puncture in the cistern magna and subarachnoid space at the lumbar level. Registration of arterial, venous and liquor pressures was carried out on a 4-channel polygraph using mercury electromanometers. An increase in ICP was achieved by introducing a warm isotonic sodium chloride solution: into the cistern magna in 2 animals, and into the subarachnoid space at the lumbar level in 3 animals using the Bobrov apparatus. Blood flow in the internal carotid arteries and jugular veins was studied using an ultrasonic flowmeter percutaneously and on exposed vessels, in the vertebral arteries - percutaneously. Volumetric blood flow in the exposed internal carotid artery was measured with an electromagnetic flowmeter. The pulsation of the M-echo signal was assessed using an echoencephaloscope.
As a result, it was revealed that in 5 animals of the first group, during the cessation of cardiac activity for 5-10 minutes, there was no blood flow in the main arteries of the head and internal jugular veins, and M-echo pulsation was not detected. After 20-30 minutes of cardiac massage, the studied hemodynamic parameters practically reached the norm and remained so throughout the rest of the experiment; the M-echo pulsation coefficient was also within the normal range (10-20%). Thus, precerebral blood flow, echopulsation, and ICP did not change noticeably before cardiac arrest and after cardiac arrest. In animals of the second group it was revealed that when ICP rises to 30-35 mm Hg. There were no significant changes in linear blood flow velocity (LBV) in the main arteries of the head and volumetric blood flow velocity in the internal carotid arteries - they remained the same or increased slightly. The M-echo pulsation coefficient gradually increased to 40-50%.
Thus, an increase in ICP to a certain level is not accompanied by a significant change in both precerebral and, probably, intracerebral arterial blood flow, which is apparently associated with the preservation of autoregulation of cerebral blood flow. At the same time, already at this stage of the experiments, a pronounced increase and asymmetry of the venous signal was noted, which confirms the opinion about the greater sensitivity of cerebral phlebocirculation to ICP fluctuations. A further increase in ICP to the level of arterial diastolic pressure (60-65 mm Hg) caused a decrease in the average BFV, mainly due to a decrease in diastolic velocity, which was graphically expressed by a corresponding decrease in the BFV components on Dopplerograms, with the diastolic component directly approaching the isoline. This correlated with a decrease in volumetric blood flow along the ICA. The M-echo pulsation coefficient changed noticeably, but ambiguously: in 2 animals it increased to 80-90%, in the other 3 it decreased to 10-15%.
With a subsequent increase in ICP and its approach to the value of the average systemic blood pressure (75-100 mm Hg), the animals developed bradyarrhythmia, dilated pupils, strabismus, and respiratory impairment occurred until it stopped completely. With the appearance of respiratory arrhythmia, all dogs were started on mechanical ventilation, which was continued for 2-5 hours until death. Along with the cessation of breathing, the animals experienced a sharp drop in blood pressure, which then, despite the periodic administration of 0.3 ml of a 0.2% norepinephrine solution, which caused a short-term rise to 200/120 mm Hg, could only be maintained at a level of 60/ 35—90/60 mm Hg. This situation most likely represented SM with still ongoing, but sharply weakened cardiac activity.
An echopulsographic examination revealed the absence of pulsations of the ventricular system. On Dopplerograms of the internal carotid and vertebral arteries, a negative pathological wave appeared in the diastolic period of blood flow, which reflected the cessation of cerebral perfusion. Graphic and digital registration of instantaneous volumetric blood flow velocity in the ICA gave equal values of blood volume in the positive and negative phases of circulation; thus, the averaged volumetric blood flow was zero. An angiographic study demonstrated a stop phenomenon at the level of the vertebral arteries. It is interesting that if the increase in blood pressure after the administration of norepinephrine was very short-term (5-7 minutes) and practically did not change the Dopplerogram pattern and volumetric blood flow indicators, then a decrease in ICP by 20-30 mm Hg. soon after the cessation of cerebral perfusion was recorded on Dopplerograms of the main arteries of the head as a physiological model of blood flow, which again became reverberant with a subsequent increase in ICP. When signs of SM appeared, the venous signal sharply decreased in parallel with the arterial signal.
Pathophysiology of changes in internal organs associated with brain death
The absence of the descending regulatory influence of the brain on all organs and tissues of the body transforms metabolism. These changes become most important during the conditioning of a potential donor, when the question arises of maintaining the good functioning of the organs intended for transplantation.
The death of hypothalamic neurons and compression of the pituitary stalk as a result of herniation of the diencephalon leads to cessation of the secretion of a number of hormones. Antidiuretic hormone has a short half-life, and if it does not enter the blood, its concentration drops significantly within 15 minutes, and after 4 hours even trace amounts of the hormone are not detectable in plasma. This is manifested by the clinical appearance of diabetes insipidus in 77% of cases of SM [19]. Current recommendations for conditioning bodies with SM include mandatory administration of vasopressin, which helps stabilize the condition.
The adenohypophysis, due to its anatomically precise correspondence to the sella turcica, is rarely damaged as a result of the action of a traumatic agent. At the beginning of research, it was noted that with established SM, the hormonal function of the anterior pituitary gland is often preserved, which was used as an argument against the concept itself. Currently, this phenomenon is associated with the characteristics of the blood supply to the pituitary gland [16].
The main result of changes in thyroid hormone metabolism that develop as a result of the death of the hypothalamus is a progressive decrease in the level of triiodothyronine (T3). Currently, triiodothyronine infusion is included in the protocols for the management of such patients in most scientific centers. However, precise determination of the indications, duration and required concentrations of hormones administered is the goal of ongoing and future research.
Often, with established SM, hyperglycemia is observed, which requires correction. It can be caused not only by dysfunction of the pituitary gland [24]; perhaps, disruption of the functioning of insulin receptors also plays a role [28].
Massive release of catecholamines in response to TBI or other brain injury can manifest as a hypertensive crisis in pheochromocytoma and lead to myocardial damage in 42% of cases due to vasoconstriction, as determined by ECG in the immediate hours after the event. This mechanism, similar to the development of Prinzmetal's angina, can explain changes in coronary angiograms and the frequent development of acute hypotension even in young patients. Loss of baroreceptor sensitivity and the development of heart rate and blood pressure variability as a result of the disappearance of the parasympathetic and adrenergic influence leads to the development of hypotension, requiring correction with vasopressors [28].
Thus, activation of the sympathoadrenal system has a damaging effect on the myocardium and can cause pulmonary edema, while having little effect on other organs. Hemodynamics are disrupted as a result of loss of vascular tone and the development of hypovolemia against the background of damage to the hypothalamic-pituitary system. As a result of ongoing irreversible changes, inevitable asystole occurs.
Pathological anatomy of brain death
As soon as the blood supply to the brain tissue stops, the processes of necrosis and apoptosis begin. Autolysis develops most rapidly in the diencephalon and cerebellum. As mechanical ventilation is carried out when cerebral blood flow has stopped, the brain gradually becomes necrotic, and characteristic changes appear that directly depend on the duration of respiratory support. Such transformations were first identified and described in patients who were on mechanical ventilation for more than 12 hours in an extreme coma. In this regard, in most English and Russian language publications this condition is referred to as “respiratory brain” (RM).
In Russia, a large research work that revealed a correlation between the degree of changes in brain tissue and the duration of mechanical ventilation in bodies meeting the criteria for SM was carried out by L.M. Popov [4]. The duration of mechanical ventilation until the development of asystole ranged from 5 to 113 hours. According to the duration of stay in this state, 3 stages of morphological changes in the brain, characteristic specifically for RM, were identified. The picture of RM was complemented by necrosis of the two upper segments of the spinal cord, which was an obligate sign.
In the 1st stage, corresponding to a duration of SM of 4-5 hours, morphological signs of brain necrosis are not detected. However, already at this time, characteristic lipids and blue-green fine-grained pigment are detected in the cytoplasm. Necrotic changes are observed in the inferior olives of the medulla oblongata and the dentate nuclei of the cerebellum. Circulatory disorders develop in the pituitary gland and its funnel.
In the 2nd stage (12-23 hours SM), in all parts of the brain and I-II segments of the spinal cord, signs of necrosis are revealed without pronounced decay and only with initial signs of reactive changes in the spinal cord. The brain becomes more flabby, and initial signs of disintegration of the periventricular sections and hypothalamic region appear. After isolation, the brain is spread out on the table, the structure of the brain hemispheres is preserved, while ischemic changes in neurons are combined with fatty degeneration, granular decay, and karyocytolysis. In the pituitary gland and its funnel, circulatory disorders increase with small foci of necrosis in the adenohypophysis.
The 3rd stage (extraordinary coma 24-112 hours) is characterized by increasing widespread autolysis of necrotic brain substance and pronounced signs of demarcation of necrosis in the spinal cord and pituitary gland. The brain is flabby and does not hold its shape well. The affected areas - the hypothalamic region, the uncinates of the hippocampal gyri, the cerebellar tonsils and periventricular areas, as well as the brain stem - are in the stage of decay. Most neurons in the brainstem are missing. The arteries and veins of the surface of the brain are dilated and filled with hemolyzed red blood cells, which indicates a cessation of blood flow in them. Characteristic is the detection in the subarachnoid and subdural space of the spinal cord of microparticles of necrotic cerebellar tissue, which is carried by the CSF flow to the distal segments.
As already noted, different parts of the brain are not destroyed simultaneously. Often, autopsy reveals a typical picture of PM in the area of blood supply to the vertebrobasilar region, while in other areas of the brain the changes are much less pronounced. Apparently, this is due to the anatomy of the circle of Willis. In such situations, it is sometimes possible to record the residual bioelectrical activity of the least damaged areas of the brain in the clinical picture of SM.
The maximum duration of observation of bodies with established SM, who underwent mechanical ventilation and measures to maintain hemodynamics, was 32 days. At autopsy, in this and other cases of long-term (more than 14 days) conditioning of bodies with SM, the brain completely lost its structural integrity and poured out of the cranial cavity.
It should be noted that RM has now become an extremely rare find. A series of 12 autopsies carried out in 2008 on bodies with SM never revealed signs of RM [30]. This is due to a significant reduction in observation time after the first establishment of the SM clinic and before disconnecting the body from mechanical ventilation.
Clinical signs of brain death
Through long-term observation and multicenter studies, a set of clinical signs reliably corresponding to SM was obtained. The basis for diagnosing SM is coma, the absence of any reflexes that close at the level of the brain stem, and persistent apnea.
Coma
is one of the main signs of severe brain damage. Traditionally, the Glasgow Coma Scale (GCS) is used to determine its depth, but the uncertainty of its interpretation in intubated patients and especially in the presence of spinal automatisms limits the use of GCS in cases of suspected SM.
Developed in 2005 at the Mayo Clinic, the FOUR scale is significantly better suited for assessing the depth of coma in intensive care unit patients (Table 1),
| Table 1 |
since it allows one to evaluate brainstem reflexes, does not depend on speech contact, and makes it possible to correctly evaluate spinal automatisms.
This scale was validated in a large multicenter study and is becoming increasingly widespread around the world [21, 29]. Brainstem areflexia
. The diameter of the pupil is dynamically maintained due to the impulse of parasympathetic neurons, which are located in the nuclei of the brainstem and sympathetic ones, localized in the cervical segments of the spinal cord. When brain stem cells die, the reflex constriction of the pupil to direct bright light disappears, and it expands, becoming 4 to 6 mm in diameter. A Japanese study of 3 cases of SM found that pupil diameter may change slowly [20]. We have repeatedly observed pupils with a diameter of 4 mm in bodies with SM, and then in cadavers after the development of asystole [9].
With SM, any eye movements should be absent. First of all, during examination it is necessary to exclude any spontaneous movements, any type of nystagmus. In addition, it is necessary to ensure that there are no induced movements of the eyeballs. Two tests are used for this - the oculocephalic reflex and the caloric test. Limitations for their implementation are trauma to the neck and base of the skull. Our group has developed a portable digital device for galvanic vestibular stimulation, which may well replace these tests, especially in the case of temporal bone and cervical spine fractures [8].
The study of the function of the V and VII nerves involves applying strong pressure to the exit points of the trigeminal nerve and the area of the temporomandibular joint on both sides simultaneously. In this case, there should be no response motor reactions, including in the muscles whose innervation is closed at the level of the spinal cord. It is also necessary to check the corneal reflex, the structure of which includes branches of both the trigeminal and facial nerves.
By examining the function of the IX, X and XI nerves, the tracheobronchial tree is sanitized. The absence of any movements during this procedure indicates a total loss of reflexes.
Apneic oxygenation test (AOT)
. Despite its widespread prevalence, to date there has not been a single large prospective study that would determine all the parameters of TAO. The procedure for conducting it has been developed empirically and the vast experience of conducting the test around the world has not been generalized [28].
Attitudes towards the apnea test itself remain ambiguous. As is known, TAO is carried out after the fact of loss of brain function has been established. Opponents of its implementation in its present form provide several arguments. Thus, not a single case of survival or transition to a vegetative state of a patient with an established complete loss of brain function, but respiratory movements that appeared during the test, was registered. Thus, the outcome of the condition is already predetermined and there is no need to subject the terminal patient to a difficult procedure. It is known that TAO can provoke the development of hypotension and hypoxemia. In this regard, organs suitable for transplantation may be damaged. Interpretation of TAO can be very difficult in patients with chest trauma, contusion, and pulmonary edema. There is also an opinion that TAO itself can cause the death of potentially viable neurons. Complications of TAO develop in more than 60% of cases, including acute arterial hypotension (12%), acidosis (68%) and hypoxemia (23%). Cases of the development of pneumothorax and pneumoperitoneum during TAO have been described.
On the other hand, supporters of TAO provide the following arguments [28]. This test is the only clinical way to check the functioning of the medulla oblongata. With proper preparation for the test, it is completely safe, and the number of complications does not exceed 15%: 14% are hypotension and 1% are arrhythmia [15]. The main vital indicators for TAO safety are: 1) intracardiac temperature ≥36.5 °C; 2) systolic blood pressure level ≥90 mm Hg; 3) absence of hypovolemia for more than 6 hours; 4) рО2≥200 mm Hg; 5) рСО2≥40 mm Hg. Art.
Our experience of performing TAO in 330 patients since the beginning of 2007 has shown that the number of fatal complications is 3%. At the same time, a significant number (more than 11%) are cases where we were unable to start the test due to the inability to select the blood gas composition to start it. Most often, the cause was uncorrectable hypoxia in patients with aspiration syndrome or prolonged mechanical ventilation, less often - the inability to reduce the pCO2 level to 45 mm Hg. in patients with a history of chronic obstructive pulmonary disease (COPD) [9].
Thus, to date, no clear opinion has been developed on the necessity and safety of conducting TAO. Most researchers tend to perform TAO after a neurological examination at the end of the observation period. Unlike Russia, in the USA and many Western European countries it is legally established that if complications develop during TAO, it can be replaced by one of the diagnostic tests confirming the diagnosis of SM.
Duration of observation
According to our legislation, in cases of primary brain damage, the period of persistence of clinical signs of SM should be at least 6 hours from the moment of their establishment. In case of secondary brain damage, observation is extended to 24 hours. Observation time can be shortened by performing double panangiography [2]. However, due to the invasiveness and unsafety of the procedure, it is used quite rarely.
In addition, the time spent on transportation, handling and evaluation totals close to a 6-hour observation period, which makes the process meaningless in the routine diagnosis of SM [9]. A study published in early 2011 analyzed 1229 cases of SM in adults and 82 cases in children in 100 US hospitals [22]. The authors showed that there is no need at all for a second examination if SM is suspected, since positive dynamics in the clinical and instrumental picture have never been recorded. Despite this, the average duration of observation of the body from the moment the first signs of SM were established and until the start of the organ harvesting operation or the development of asystole was 19.9 hours. In 12% of cases, asystole developed during the 6-hour observation period specified in the recommendation of the American Academy of Neurology.
Factors that complicate the clinical diagnosis of brain death
Spontaneous and reflex movements
. Spontaneous or stimulus-induced movements often observed in MS are called “Lazarus symptoms,” the most dramatic of which is flexion of the torso 40-60° and folding of the arms in a praying position.
Complex spinal automatisms are most often caused not so much by painful stimuli as by irritation of proprioceptors. It is especially worth noting forced turns of the head when studying oculocephalic reactions and inducing tendon reflexes [27] (Table 2).
| Table 2 |
| ]]> |
According to our data, various types of spinal activity in brain-dead bodies are observed in 44%. This introduces significant difficulties in interpreting the clinical picture and requires additional methods to assess the bioelectrical activity of the brain and cerebral blood flow. The Lazarus symptom makes a particular impression on nursing staff in intensive care units. To avoid misunderstandings, this necessarily requires clarification from the head of the department and the doctors participating in the consultation.
Intoxication
. Substances that depress the activity of the central nervous system can cause a picture of intoxication that mimics the clinical picture of SM. In intensive care for conditions that potentially cause deep coma, such medications are used very widely. There are also cases of suicide attempts in which tricyclic antidepressants, antipsychotics and antiepileptic drugs are used. If intoxication is suspected, a toxicological examination is carried out. Diagnosis of SM does not begin until its signs completely disappear [2].
Metabolic disorders
. In the differential diagnosis of deep coma, which may look like SM, we must not forget about the potential presence of severe metabolic disorders, accompanied by almost the same clinical picture. A distinction must be made between acute metabolic disorders, which lead to irreversible destruction of the brain as a result of edema and demyelination, and deep coma caused by systemic disorders. SM can occur as a result of the acute development of fulminant liver failure, acute ketoacidosis during hyperglycemic coma, and demyelination during pontine myelinolysis [3].
Hypothermia
. The recent increase in the number of patients with this pathology forces us to pay close attention to it. Potentially severe hypothermia can simulate SM. With SM, as a result of the destruction of the hypothalamus, in which the thermoregulation centers are located, a gradual decrease in body temperature often occurs. This sign is not obligate, but is very common. Hypothermia in such patients requires correction by warming and is not an exclusive factor in determining SM [12, 31].
Thus, there are many conditions that make an accurate and unambiguous clinical diagnosis of SM impossible. In such cases, various paraclinical methods are traditionally used.
Paraclinical methods for diagnosing brain death
To confirm SM, additional studies are used, which can be divided into three groups: 1) direct methods confirming the cessation of biological activity of neurons - EEG, multimodal evoked potentials (EP); 2) indirect methods confirming the cessation of intracranial blood flow and cerebrospinal fluid pulsation - selective carotid cerebral angiography (CA), transcranial Dopplerography (TCD), echoencephalopulsography (Echo-ES), cerebral scintigraphy with 99mTc pertechnetate, magnetic resonance imaging (MRA) and computed tomography ( CTA) angiography; 3) indirect methods showing metabolic disorders of the dead brain - determination of oxygen tension in the bulb of the jugular vein, infrared cerebral oximetry. This also includes telethermography (TSG), since the temperature of various parts of the body reflects the level of metabolism of the underlying organs and tissues.
Methods for confirming SM should ideally meet certain requirements: 1) their feasibility directly at the patient’s bedside; 2) the examination should not take much time; 3) must be safe for the subject and potential recipient of donor organs, as well as for the medical personnel performing them; 4) be as sensitive, specific, reproducible and protected from external factors as possible. At the moment, only two methods for confirming SM have been legalized in Russia - superselective CA to reduce observation time and EEG if it is impossible to clinically evaluate oculocephalic and oculovestibular reactions.
EEG was the first method used to confirm the diagnosis of death. The phenomenon of bioelectrical silence was clearly regarded as a sign of the death of all neurons in the brain. There have been many studies examining the sensitivity and specificity of the method, and a general review analysis conducted in 1990 found it to be in the range of 90%. Such relatively low indicators are explained by the low noise immunity of the EEG, which is especially pronounced in intensive care units. The EEG specificity determined in prospective studies reduces the phenomenon of its inhibition in response to intoxication and hypothermia. Despite this, EEG remains one of the main confirmatory tests and is widely used in many countries, including Russia. Since many different methods for recording bioelectrical brain activity have been described, the American Electroencephalographic Society has developed recommendations that include the minimum technical standards for EEG recording necessary to confirm SM [17]. In recent years, there have been more and more reports of false-negative EEG results in the clinical picture of SM confirmed by angiography. The inability to study the bioelectrical activity of the brainstem, high sensitivity to drug intoxication, metabolic disorders and artifacts allowed one of the experts to call EEG “the worst method for confirming brain death” [18].
The VP method began to be studied and used in the 50s of the last century. Somatosensory (SSEP), acoustic brainstem (ASEP) and visual (VEP) evoked potentials are used to confirm the diagnosis of SM. The studies carried out to determine their information content revealed ambiguity for each type of VP. Currently, the VP method is included in the list of tests in the legislation of almost all European countries and the USA.
In addition, the method of galvanic vestibular stimulation (GVS) is of particular interest, which consists of bilateral stimulation of the mastoid region with a direct current of 1 to 3 mA and a duration of up to 30 s. Direct current irritates the peripheral part of the vestibular analyzer, causing nystagmus, which is similar in mechanism of development to caloric nystagmus. Thus, the GVS method may be an alternative to performing a caloric test for injuries to the external auditory canal.
CA was one of the first methods proposed to ascertain the arrest of intracranial blood flow. Despite the use of the method since the 60s of the last century, large multicenter studies that accurately demonstrated the sensitivity and specificity of angiography have not been conducted to date [28]. However, it is included as one of the confirmatory tests in most national recommendations, mainly as an alternative to a long period of observation.
Observation and proof of irreversibility of pathology
In the absence of breathing, we can talk about the loss of vital activity of the entire brain; the doctor can only establish the fact that this process is completely irreversible. The irreversibility of brain disorders can be judged after a certain period of observation, depending on the cause of the pathology that caused the death of the nervous tissue.
If primary brain damage has occurred, then to establish brain death, the duration of observation must be at least 6 hours from the moment when the symptoms of the pathology were first recorded. After this period, a repeat neurological examination is performed, and the apnea test is no longer necessary.
Previously, it was recommended to observe the patient for a minimum of 12 hours, but now in most countries of the world the time has been reduced to 6 hours, since this time interval is considered sufficient to diagnose brain death. In addition, reducing observation time plays an important role when planning organ transplantation from a brain-dead patient.
In case of secondary damage to the nervous tissue, a longer observation is required to make a diagnosis of brain death - at least a day from the moment of the initial symptoms of the pathology. If there is reason to suspect poisoning, the time is increased to 72 hours, during which neurological monitoring is carried out every 2 hours. If the results are negative, brain death is declared after 72 hours.
Based on the stated diagnostic criteria, during observation of the patient, undoubted signs of brain death are recorded - the absence of reflex and brainstem activity, a positive apneic test. These parameters are considered absolutely indicative and reliable, not requiring additional examination, and therefore are used by doctors all over the world.
Thiamine deficiency and Korsakoff-Wernicke disease
If a person systematically drinks alcohol, without control over the amount he drinks, and this lasts for quite a long time, then he has every chance of developing brain dysfunction or damage to his cells. Moreover, this can be caused by the consumption of large amounts of alcohol, or there may be serious disturbances in the liver due to chronic alcohol dependence.
For example, most people suffering from chronic alcohol addiction have a lack of thiamine in their bodies, or as it is also called vitamin B1. It may be lacking due to poor nutrition, metabolic disorders in the body and, of course, due to the abuse of alcoholic beverages. It plays an indispensable role in the metabolism of carbohydrates, lipids, and proteins. It supports the normal functioning of the cardiovascular system, digestive tract, and nervous structures.
Most people suffering from chronic alcohol addiction are deficient in vitamin B1. And this can lead to such a serious illness as Korsakoff-Wernicke syndrome, or more precisely, Wernicke syndrome and Korsakoff syndrome.
Wernicke's disease is characterized by paralysis of the eye muscles, disturbance of consciousness and impaired coordination of movements. Sometimes a patient with a similar syndrome cannot independently find the door of the room to leave, he cannot move without someone else's help. If at least one of the signs of the disease appears, you need to urgently seek medical help.
Most people suffering from alcohol dependence, along with Wernicke's syndrome, experience Korsakoff's syndrome, which is also called alcohol paralysis. With this disease, memory impairment is observed, when he forgets everything that happened to him before the disease, but can describe in great detail the events that took place several years before.
In addition, he remembers well everything that happens to him after his illness. The patient begins to invent non-existent events, or talk about those that really happened, but at the same time greatly distorts the facts. All this is accompanied by disorientation. The patient ceases to navigate the world around him and himself. Sometimes, even after seeing his reflection in the mirror, the patient does not realize that it is him.
Call us now:
+7 (812) 454-00-50
Prices for Ultramed clinic services
Additional examinations
Of the additional examinations that may affect the diagnosis, electroencephalography (EEG) and angiography are permitted. EEG is indicated for those patients for whom it is difficult to determine reflexes - in case of injuries or suspected injuries of the cervical spinal column, ruptured eardrums. An EEG is performed after all tests, including apnea. In brain death, it shows the absence of any electrical activity in the nerve tissue. If the indicators are questionable, the study can be repeated or using stimuli (light, pain).
non-collapsed cerebral vessels are normal on angiography
If EEG is indicated in clinically complex cases and does not affect the duration of general observation, then panangiography of the carotid and vertebral arteries is designed to shorten this time as much as possible. It is carried out at the final diagnostic stage and confirms the irreversibility of the cessation of brain activity.
For example, in case of possible intoxication, the patient should be observed for at least three days, but brain death can be determined early if, immediately after the appearance of signs of loss of its functions, the main arteries of the brain are examined twice with an interval of at least half an hour. In the absence of contrasting of the arteries, we can talk about a total and irreversible stop of cerebral blood flow, and further observation becomes impractical.
Video: example of an EEG to confirm brain death
Clinical diagnosis of biological brain death is labor-intensive, requires constant monitoring and maintenance of vital functions, so for many years the search has been underway for another method that would allow us to establish a reliable diagnosis with no less accuracy than the clinic. However, no matter how hard the experts try, none of the proposed methods is comparable in accuracy and reliability to a clinical assessment of the state of the brain. Moreover, other techniques are more complex, less accessible, invasive or not specific enough, and the result is greatly influenced by the experience and knowledge of the doctor.
The desire to speed up the process of ascertaining brain death is largely due to the rapid development of a new branch of medicine - transplantology. Considering the diagnosis of brain death from this position, we can say that the price of a conclusion about brain death may be not one, but several lives - both of the potential donor and of other people in need of organ transplants, therefore haste or non-compliance with the observation algorithm is unacceptable.
When deciding to declare brain death, the doctor must remember the ethical side of the issue and the fact that the life of any person is priceless, therefore strict compliance of his actions with the established rules and instructions is mandatory. A possible mistake increases the already high degree of responsibility, forcing you to repeatedly play it safe and doubt, double-check and weigh every step.
The diagnosis of brain death is established jointly by a resuscitation specialist and a neurologist, and each of them must have at least five years of work experience. If additional examination is necessary, specialists of other profiles are involved. Transplantologists and other persons involved in the collection and transplantation of organs cannot and should not participate in or influence the process of diagnosing brain death.
The effect of alcohol on the female brain?
Complications caused by drinking alcoholic beverages are more serious in the fairer sex than in men.
It has been experimentally proven that ethanol behaves much more aggressively towards the cells of a woman’s body than towards the cells of a man. Organs and their functions are more susceptible to the negative effects of alcohol. The destruction of the liver, damage to the heart muscle and cells of the nervous system occurs faster.
Having carried out a comparative analysis of the results of studies of the human brain using MCT, scientists have established the fact that the negative effects of ethanol manifest themselves in the fact that the brain decreases in size.
The degree of such a decrease is the main indicator that organic changes are present in the brain cells. And the longer the experience of drinking alcohol, the higher these indicators.
In addition, the results of the experiments showed that both women and men who suffer from alcohol addiction face certain problems when they have to learn something or remember any information. All this occurs due to frequent consumption of alcoholic beverages.
Note that the male representatives who participated in such an experiment had twice as much experience of regular consumption of large amounts of alcohol than the fairer sex.
It turns out that the negative effects of ethanol on both the male and female brains manifest themselves in the same ways. But it is necessary to take into account that women took exactly half as much alcohol. From all this we conclude that ethanol has a stronger effect on the female brain.
In contrast, two articles were recently published in an American publication discussing the role of gender in the effects of ethyl alcohol on the body.
The authors came to the opposite conclusion, that is, according to them, ethanol has the same effect on everyone without exception. This means that experiments of this kind need to be continued in order to find out the specific effects of ethyl alcohol on a woman’s brain cells.
After diagnosis...
Once brain death has been confirmed by all clinical data, doctors have three options. In the first case, they can invite transplantologists to decide on the issue of organ collection for transplantation (this mechanism is regulated by the legislation of a particular country). In the second, talk to your family, explain the essence of the pathology and the irreversibility of brain damage, and then stop artificial ventilation. The third option, the most economically unprofitable and impractical, is to continue maintaining the functioning of the heart and lungs until they decompensate and the patient dies.
***
The problem of brain death with intact cardiac activity is not only of a medical nature. It has a significant moral, ethical and legal aspect. Society as a whole knows that brain death is identical to the death of the patient, but doctors have to make serious efforts, tact and patience when talking with relatives, deciding on transplantation issues and determining the final option of their actions after making a diagnosis.
Unfortunately, cases of distrust in doctors, unjustified suspicions of unwillingness to continue treatment, and accusations of negligence in their duties are still common. Many people still think that with a superficial assessment of the patient’s condition, the doctor will simply turn off the ventilator without making sure that the pathology is irreversible. At the same time, delving into the diagnostic algorithms, one can imagine how long and difficult the path to the final diagnosis is.
Literature:
- Sytinsky, I.A. Alcohol and the brain. - Baku: Society "Knowledge" of the AzSSR, 1981. - 38 p.
- Etin G. M. Alcohol and the brain: lecture notes. - M.: Center of the Scientific Research Institute of Health Education of the USSR Ministry of Health, 1967. - 23 p.
- Popova E. N. Brain, alcohol and offspring. - Kazan: Kazan University Publishing House, 1994. - 147 p.
- Popova E. N. Ultrastructure of the brain, alcohol and offspring. - M.: Scientific world, 2010. - 155 p.
Need some advice?
OR CALL A DOCTOR
CALL!
+7