Hypertension is a symptom of significantly increased blood pressure. Bradycardia is a symptom in which the heart rate decreases to sixty beats per minute. The combination of the two is rare because with high blood pressure, the heart is more likely to speed up to supply oxygen to the entire body rather than slow down. Therefore, it is difficult to choose drugs for hypertension and bradycardia - most drugs, on the contrary, slow down the heart rate in people with hypertension.
The mechanism of bradycardia in hypertension
The human heart is a complex system that is controlled by the sinoatrial node. This is where signals coming from the brain are interpreted, and problems with it lead to bradycardia. The signals are not read correctly and the heart beats slower. The reasons for this are different.
Depending on them, bradycardia can be:
- Medicinal - occurs after taking glycosides, antiarrhythmic drugs, beta-blockers and many other drugs;
- neurogenic - caused by a contraction of the nervous system, causing peptic ulcers, depression, neurosis, obsessive-compulsive states or hypertension;
- endogenous - formed as a result of an increase in the amount of oxygen, calcium or potassium in the blood;
- toxic - occurs as a result of infection, such as influenza, sepsis, typhoid fever;
- cardiogenic - develops as a symptom of cardiovascular diseases such as coronary heart disease or cardiosclerosis;
- senile - develops as a result of deterioration of the heart apparatus.
There is also an idiopathic form - it develops in addition to hypertension for unclear reasons.
Factors contributing to the development of bradycardia and arterial hypertension are similar:
- elderly age;
- abuse of bad habits;
- physical inactivity;
- bad eating habits, stress, lack of sleep or too much sleep.
Due to the rarity of this combination, it is difficult to treat.
Frequently asked questions about bradycardia
What medications can be taken for bradycardia?
If you begin to notice a slowing of your heartbeat, then rush to see a doctor to determine the cause. Medicines are prescribed depending on the origin and type of pathology. Do not try to stop a sudden attack of acute bradycardia on your own. Better call an ambulance.
What causes bradycardia?
There may be several reasons for a decrease in heart rate. The leading place among them is occupied by organic heart lesions. Disorders of the nervous system, diseases of the thyroid gland and stomach, and the use of certain drugs can also provoke a slowdown in heart rate. Sometimes bradycardia is accompanied by severe poisoning.
What to take if your heart rate is low?
For mild sinus bradycardia, it is enough to drink “Zelenin Drops” 2-3 times a day, 20-30 drops with water. If bradycardia is accompanied by painful symptoms and does not go away, then you cannot do without medical help.
How dangerous are these two diseases?
First of all, the general well-being of a person simultaneously suffers from the presence of high blood pressure and bradycardia. He becomes irritable, cognitive functions suffer, and he has difficulty concentrating. Headache. Shortness of breath appears - first during activity, then at rest.
To make matters worse, complications begin to develop over time:
- heart disease - hypertension and bradycardia develop, for example, heart failure;
- nervous system disorders - endogenous depression, cerebral hemorrhages;
- eye disease that can lead to complete blindness;
- diabetes, which seriously impairs quality of life;
- Morgagni-Adams-Stokes syndrome - affects brain cells, the patient may experience sudden attacks of seizures, accompanied by convulsions, which can lead to death;
- Sudden cardiac arrest syndrome is a classic complication of bradycardia that occurs because the body cannot function normally with a heart rate below forty beats per minute.
And, of course, complications include heart attack and stroke, which are often fatal.
What is its danger?
Due to the weakening of the contractile function of the myocardium and the slowing of blood circulation, the brain, which experiences hypoxia (oxygen starvation), reacts first. Therefore, bradycardia can lead to attacks of loss of consciousness and convulsions, which can last from several seconds to 1 minute. This is one of the most dangerous conditions with bradycardia, which requires emergency medical measures. If assistance is not provided in a timely and correct manner, respiratory activity may stop.
Characteristic symptoms and signs
The patient's diagnosis of a combination of bradycardia and arterial hypertension can be identified by symptoms. This includes:
- chronic fatigue - constant craving for sleep;
- dizziness - intermittent, usually due to physical exertion;
- general weakness - it is difficult for the patient to concentrate, it is difficult to perform actions that previously did not cause problems in a healthy state;
- shortness of breath - initially occurs only during physical activity, progresses over time and even occurs at rest.
Occasionally, the patient experiences attacks that are accompanied by an increase in blood pressure along with bradycardia. The pulse slows down and breathing becomes difficult. Sharp stabbing pain in the left side of the chest may spread to the arm.
She may be confused and may not respond if asked how she is doing.
A blood pressure diary, which is recommended for everyone over the age of 50, can also be used to track disease combinations. If measurements show that your blood pressure is constantly or frequently elevated, consult your doctor.
Diagnostic methods
To make a diagnosis, the doctor must perform several diagnostic procedures:
- Obtain a medical history. The patient should be asked about symptoms, whether he has previously had high blood pressure, whether there are any concomitant diseases or allergies.
- Exam. The doctor listens and taps on the chest - if a person is sick, the sound will be different from normal.
- Echocardiogram and ultrasound. Allows you to get a complete picture of the condition of the heart.
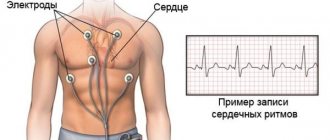
- Cardiogram. Allows you to find out how the heart works, whether there are any malfunctions. It is there that the presence of bradycardia in a patient can be detected.
- Angiography. This allows you to find out the condition of the blood vessels.
In addition, if the doctor sees such a need, he can put a device on the patient that will monitor heart rate and blood pressure throughout the day. Test results will help make a diagnosis.
Diagnosis of bradycardia
When diagnosing bradycardia, use:
- physical diagnostic methods (examination, palpation, percussion, auscultation)
- electrocardiographic examination
- 24-hour ECG monitoring
- Ultrasound of the heart
- load bicycle ergometry
- transesophageal electrophysiological study of cardiac conduction tracts. Using this examination, it is possible to determine whether bradycardia is organic or functional in nature.
Another way to detect arrhythmia is to measure pressure using an electronic tonometer. Modern electronic tonometers, as well as Microlife tonometers, have a pulse measurement sensor.
Advantages of treating bradycardia in hypertension with medications
Many older people are afraid to take blood pressure pills. They all seem to be made up of terrible chemicals and have devastating side effects on the body. In fact, it is almost impossible to treat hypertension with bradycardia without medications.
They have several positive effects:
- Inotropic effect - under the influence of the drug, the heart begins to contract more strongly, and thus the effect of bradycardia is reduced;
- chronotropic effect - as a result of taking drugs, the heart begins to beat faster
- dromotropic effect - provides a higher speed of impulse that travels through the nervous system from the brain to the heart and signals the need for contraction
- butotropic effect - increases the sensitivity of the heart to nerve impulses.
There are also additional effects. For example, strengthening blood vessels or increasing oxygen levels in the blood. Although a different lifestyle can achieve a lot, pills are necessary.
List of tablets for high blood pressure: names and properties
If you have high blood pressure and bradycardia, you shouldn't take all the medications—only those that won't slow your heartbeat.
- Alpha adrenergic blockers. These drugs are universal because they do not slow down the heart rate, but increase it. They reduce the tone of peripheral vessels, reduce the load on the heart muscle and reduce the heart's need for oxygen, which leads to a gradual decrease in blood pressure. Their active ingredients are different. The most common are prazosin (found in Polpressin), doxazosin (found in Zoxon, Artesin) and Terazosin (found in Hytrin).
- ACE inhibitors. An increase in the amount of an enzyme in the blood that replaces another enzyme that increases blood pressure. They do not affect heart rate. Examples are enalapril, lisinopril, quinapril, ramipril, perindopril.
In addition, the treatment regimen includes diuretics, which remove excess water from the body and thereby reduce blood pressure. Among them, loop groups (furosemide), thiazide and thiazide (hypothiazide) and potassium-sparing (spironolactone) groups are used.
Also - Atropine, a drug recommended for seizures. At home it is taken in tablets, in the hospital - intravenously. The dose is always the same - five milligrams.
If the attack resulted in loss of consciousness—which can happen if the heart rate drops below forty beats per minute—the patient called an ambulance and received emergency treatment:
- Position them so that their head is above their feet;
- unbutton tight clothes, open the window in the room;
- turn the patient's head to the side so that he does not choke on vomiting if it occurs.
If the pulse stops before the ambulance arrives, chest compressions may need to be started. All drugs should be selected only with a doctor - the treatment regimen for patients with arterial hypertension is complex and depends on concomitant diseases, allergies, age and personal preferences. Self-prescription and dosing mean an unnecessary risk to your health.
Preventive methods to combat the disease
And, of course, we should not forget that no treatment for bradycardia and high blood pressure will help if we do not change our lifestyle. These changes should be comprehensive and start with the daily routine:
- Sleep at least eight hours a day, this time should be at night - at night, in the dark, the body recovers best;
- You need to go to bed and get up at the same time so that the body can get used to it;
- The daily routine should include a half-hour or even longer walk, which can be taken at a leisurely pace in the nearest park;
- The daily routine should include time for quiet rest without any irritants - sit in a chair for ten minutes with your eyes closed and not think about anything.
You must give up bad habits. Alcohol worsens high blood pressure because it worsens blood vessels and retains water in the body. Tobacco also negatively affects blood vessels and helps reduce the overall immunity of the body.
Don't forget about food - the diet should be simple and healthy. To do this you need:
- Eliminate foods containing a lot of animal fat - full-fat milk, butter, cottage cheese, fatty parts of red meat;
- exclude fast food - they contain harmful additives, are too high in calories and generally have a negative effect on health;
- Reduce the consumption of fried, fatty, smoked, salty, spicy foods - you don’t need to give up your favorite foods, but you need to control their consumption, otherwise hypertension will clearly progress;
- Increase your consumption of white meat and vegetables - they can be eaten boiled, stewed, baked, or even fried in a little oil;
- increase the consumption of low-fat dairy products - you can drink kefir or milk, eat cottage cheese or yogurt, eat processed and hard cheeses;
- Try to eat a variety of low-fat foods whenever possible.
Recommendations for lifestyle changes associated with this disease can also be used to prevent serious cardiovascular diseases, not just bradycardia associated with hypertension.
Sinus bradycardia
The incidence of sinus bradycardia is unknown, given that most cases of sinus bradycardia are normal.
Typically, sinus bradycardia is an incidental finding in healthy people, especially young people, athletes, or is recorded during sleep. Other causes of sinus bradycardia are associated with increased vagal tone.
Physiological causes of increased vagal tone include bradycardia, as seen in athletes. Pathological causes include heart disease (myocardial infarction, rheumatism, viral myocarditis), poisoning, taking various medications, electrolyte disorders, infections (diphtheria), sleep apnea, hypoglycemia, hypothyroidism, increased intracranial pressure.
The most common drugs that cause bradycardia include cardiac glycosides, beta blockers, calcium channel blockers, lithium, fentanyl, and clonidine. To a lesser extent, bradycardia is caused by class 1 antiarrhythmic drugs, amiodarone.
Sinus bradycardia is also observed after bariatric surgery. About 121,000 bariatric surgical procedures are performed annually. There are reports of sinus bradycardia after significant weight loss associated with surgery, but no systematic studies have been conducted to date.
Sinus bradycardia can also be caused by sick sinus syndrome (SSNS), which is associated with an impairment of the sinus node's ability to generate and/or transmit an action potential. SSS combines a whole spectrum of arrhythmias, including sinus bradycardia, sinus arrest, sinoatrial block and paroxysmal supraventricular tachyarrhythmias, followed by periods of bradycardia and/or asystole (tachy-brady syndrome). Sick sinus syndrome most often occurs in elderly patients with underlying cardiovascular disease.
Symptoms of sinus bradycardia may include causeless weakness and fatigue, dizziness, shortness of breath, chest pain, cognitive dysfunction, and emotional lability. As bradycardia increases, cerebral symptoms become more pronounced (the appearance or intensification of dizziness, momentary memory loss, paresis, “swallowing” of words, insomnia, memory loss). The most common complaints include a feeling of dizziness, severe weakness, even fainting (Morgagni-Edams-Stokes attacks). Fainting of a cardiac nature is characterized by the absence of an aura and convulsions.
Laboratory tests may be helpful in suggesting that the cause of bradycardia is due to electrolyte abnormalities, medications, or poisoning. In cases of sick sinus syndrome, routine laboratory tests are rarely of much value. Reasonable screening tests may include electrolytes, glucose, thyroid hormones, thyroid-stimulating hormone, cardiac troponins, and various toxicology tests.
On an ECG with sinus bradycardia, a P scar is recorded (normal in terms of shape and amplitude), and the presence of sinus bradycardia in itself does not cause changes in the QRS complex and T wave.
The consequences and prognosis of sinus bradycardia are related to its etiology, namely:
- Patients with sinus bradycardia associated with toxicity from a substance (drug or toxin) have a good prognosis once the exposure is stopped (eg, the offending drug is stopped).
- Patients with sick sinus syndrome have a relatively poor prognosis for 5-year survival (ranging from 47 to 69%). However, it is unclear whether this mortality rate is a consequence of factors inherent to the bradycardia itself or is a consequence of the heart disease itself. Patients with sick sinus syndrome may develop atrial fibrillation, which can be treated with medication and does not require a pacemaker.
Treatment approaches
At the prehospital stage, it is necessary to ensure the availability of venous access, oxygen therapy, and ECG monitoring. In rare cases, transcutaneous cardiac pacing may be required even in the prehospital setting. For symptomatic sinus bradycardia (eg, syncope), intravenous atropine may be required.
In the emergency department, the principles and methods of treatment are similar to those used in the prehospital stage (monitoring, administration of atropine, placement of a temporary pacemaker (pacemaker).
In hemodynamically stable patients, the primary focus should be on determining the cause of bradycardia.
For SSSS, drug therapy has little effect—although atropine temporarily helps some patients by eliminating or reducing bradycardia, most ultimately require a pacemaker. In adult patients with persistent sinus bradycardia, pacing is indicated if there are symptoms that result from sinus bradycardia. The absolute indications for pacemaker placement are Morgagni-Adam-Stokes attacks (even a single history), bradycardia less than 40 beats/min and/or pauses of more than 3 seconds, the presence of signs of coronary insufficiency, symptomatic sinus bradycardia resulting from the necessary drug therapy.
In patients with sinus bradycardia secondary to cardiac glycosides, beta blockers, or calcium channel blockers, simple discontinuation of the drug along with ECG monitoring is often the only treatment necessary, but even in such cases, intravenous atropine or temporary pacing may sometimes be necessary. .
Treatment of post-infectious bradycardia usually requires placement of a permanent pacemaker (pacemaker).
In patients with hypothermia, pacing and atropine are generally not recommended. Warming measures in this case are the basis of therapy. Sinus bradycardia may occur in patients undergoing therapeutic hypothermia. Treatment may include vasopressors, atropine, and pacemaker.
Sleep apnea and associated bradycardia are usually treated with weight loss, nasal positive airway pressure (BiPAP), and sometimes surgery: surgery to widen the airways by moving the jaws closer together (orthognathic facial surgery) or uvulopalatoplasty.
Once the patient's condition has stabilized, inpatient care should be directed toward identifying the cause of sinus bradycardia.