Clinical picture
Manifestations of cardiopathy differ depending on its form. The following symptoms are characteristic of the stagnant variety of the disease:
- painful sensations of a pressing and aching nature in the chest, not relieved by Nitroglycerin;
- the appearance of signs of cyanosis on the face (blue skin);
- deformation of the chest due to cardiac hypertrophy (appearance of a “heart hump”).
Signs of congestive cardiopathy progress extremely quickly. Gradually, the disease leads to limited ability to move.
The restrictive form of the pathology is manifested by the following symptoms:
- pain in the heart area;
- shortness of breath with any physical activity;
- swelling of the face;
- belly growth.
The restrictive variety of the disease is diagnosed mainly in the tropics. The patient's physical activity is significantly reduced due to the worsening condition.
The hypertrophic type of the disease has pronounced symptoms:
- sharp chest pain;
- manifestation of arrhythmia;
- constant shortness of breath;
- loss of consciousness;
- dizziness.
Gradually developing heart failure aggravates the patient's condition. In advanced cases, even with light physical activity, death is possible.
Ischemic cardiopathy is characterized by the following symptoms:
- arrhythmia;
- pain in the heart;
- frequent shortness of breath;
- general weakness;
- lack of oxygen;
- excessive sweating;
- paleness of the skin;
- loss of consciousness.
Symptoms become more pronounced with physical activity. Heart failure due to ischemia progresses rapidly and can lead to thrombus rupture and death.
The manifestation of the secondary type of pathology depends on the localization and severity of the primary pathological process. Most often it is expressed by the following symptoms:
- excessive sweating;
- swelling;
- feeling of squeezing in the heart area;
- cough;
- frequent shortness of breath.
Secondary cardiopathy in children usually progresses as the primary disease develops. During diagnosis, doctors see it as a violation of the integrity of the myocardium.
The functional variety is manifested by signs of vegetative-vascular dystonia:
- fainting state;
- attacks of shortness of breath;
- arrhythmias (mainly tachycardia, extrasystoles);
- excessive sweating.
The development of the disease depends on the degree of overload of the child. If the problem is not identified in a timely manner, it will not be possible to avoid serious pathological changes in the myocardium.
It is difficult to detect cardiopathy in both newborns and adolescents. Symptoms characteristic of the disease are most often attributed to other pathologies of the cardiovascular system. A doctor can make an accurate diagnosis only with the help of a comprehensive instrumental examination.
Complications
A minor anomaly in the development of the heart (cardiopathy) is dangerous not only for its manifestations, but also for its complications. They can form due to late diagnosis and lack of treatment. With dysplastic cardiopathy, the following consequences are possible:
- angina pectoris;
- cardiac ischemia;
- arterial hypertension;
- pericarditis;
- pulmonary edema;
- arrhythmia;
- thrombosis;
- chronic heart failure.
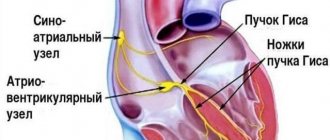
The most common complication is arrhythmia. It appears in almost 10% of the total number of sick children. Cardiopathy leads to disruption of the normal conduction of electrical impulses in cardiomyocytes. As a result, heartbeats become irregular. Most often there is an acceleration in the number of beats per minute.
When the ventricles dilate, when the disease lasts for a long time, the blood in the cavities stagnates. Conditions are created for the formation of clots.
The greatest danger is represented by blood clots that enter the bloodstream (emboli) and over time they can penetrate into narrow-diameter vessels. This feature is characteristic of lung and brain tissue. Blockage of the lumen in them will lead to throboembolism.
Causes
Cardiopathy in children mainly develops for the following reasons:
- Genetics. Cardiomyocytes (heart cells) are made of proteins. They take part in all processes performed by the heart muscle. Information about the structure of heart cells is stored at the genetic level. If the baby has a defective gene, then there is a possibility of improper development of the main organ. In this case, we are talking about the primary form of cardiopathy.
- Infectious or toxic nature. The development of cardiopathy can be influenced by toxins and infections that enter the body. They are not detected immediately due to the frequent absence of pronounced symptoms. No abnormalities of the valves or coronary vessels are detected.
- Autoimmune failures. Immune system dysfunction is mainly caused by infections, toxins and hormonal surges. The body begins to destroy its own cells, thereby causing secondary pathologies.
- Fibrosis (cardiosclerosis). Replacement of heart tissue with connective fibers leads to impaired contractility due to loss of elasticity. Fibrosis most often occurs after a myocardial infarction, so its nature is predominantly secondary.
The listed cases are considered the main ones, but doctors can only stop their manifestations. It is virtually impossible to eliminate the causes due to the lack of effective treatments.
Among the pathologies of the cardiovascular system that influence the development of cardiopathy, the most basic can be identified:
- hypertonic disease;
- cardiac ischemia;
- amyloid dystrophy (failure of protein metabolism);
- disorders in the endocrine system;
- poisoning by toxins;
- connective tissue diseases.
Characteristics of the disease
The main function of the heart muscle is to contract rhythmically, which pushes blood through the vessels and fills the cavities of the organ. This ability is provided by cardiomyocytes. Their continuous functioning maintains metabolism at the level necessary for work.
Under the influence of unfavorable factors, over time the processes presented are disrupted. This is manifested by the formation of structural changes, which ends with a weakening of contractility.
Functional cardiopathy
If the mitral valve sagging and there is an abundance of tendon threads, the doctor diagnoses functional cardiopathy. Such structural abnormalities are abbreviated as MARS (minor anomalies of the heart). They contribute to the occurrence of arrhythmia attacks during physical activity. If the child continues to overexert himself (in physical education, when playing with friends, in classes), then heart failure will begin to develop over time.
A cardiologist will need to draw up a treatment regimen if the child has persistent arrhythmia and manifestations of mitral regurgitation (backflow of blood). The doctor will prescribe magnesium-based medications and antiarrhythmic drugs as treatments. It is equally important to create a daily schedule to eliminate heart-straining activities.
When functional cardiopathy is detected, regardless of its severity, parents must protect their child from physical and mental overload and follow all the recommendations of the cardiologist. It is unacceptable to use medications to correct heart rhythm on your own, or to increase or decrease the dosages indicated in the treatment regimen. The child’s heart muscle has not yet fully strengthened, and the presence of pathological changes in the structure of the myocardium only aggravates the situation, so only a doctor can prescribe a course of therapy and change it.
To saturate the heart with useful substances, you will need to change the child’s diet. It is advisable to remove sweets, fast food and other unhealthy foods from it in favor of vegetables and fruits rich in vitamins and microelements.
What it is?
The term “dysplastic cardiopathy” refers to a group of disorders in the heart muscle of non-inflammatory origin.
Pathology is formed when there is insufficient metabolism in the myocardium. Cardiopathy is often diagnosed in the presence of mitral valve disease or the detection of an additional chord (tendon) in the left ventricle. The elastic fibers of the heart wall are gradually replaced by connective tissue that does not have this ability. The disease is accompanied by functional and structural changes in the myocardium.
Pathologies of the coronary arteries, valve leaflets and arterial hypertension are not observed in the initial stage. Over time, as the compensatory capabilities of the myocardium weaken, complications arise.
Secondary form of the disease
Secondary cardiopathy in children is a consequence of another pathological process. Often the cause of its development is the following body conditions:
- hormonal changes;
- metabolic disorders;
- poisoning with toxic substances.
Treatment of the secondary form of pathology is prescribed by the attending physician after an examination, the purpose of which is to determine the true cause of the development. The essence of therapy will be based on correcting nutrition, reducing stress on the heart and eliminating the underlying pathological process.
Our capabilities
If atypical ventricular chord is suspected or previously identified, the following examinations are recommended:
- Echocardiography is the most informative method for diagnosing various heart pathologies. During the study, the doctor evaluates the structure and contractility of the myocardium, the functioning of the valves, the movement of blood in the chambers of the heart and other indicators.
- A resting ECG is a basic test for assessing heart rhythm. Does not require special training.
You can undergo all diagnostic tests at any KinderKlinik department with subsequent consultation with a specialist.
Need some advice?
Sign up
Callback form
Application has been sent, we will contact you soon
Forecast
Cardiopathy in children has a favorable prognosis only if detected early. Stopping the pathological process in a timely manner will allow the child to live to old age, but he will have to follow the recommendations of specialists and lead a healthy lifestyle. If cardiopathy is detected late, complications may develop, leading to disability and death.
Surgical treatment (if successful) prolongs the patient’s life and can eliminate the main cause of cardiopathy. The disadvantage of the operation is the high risk of death. According to statistics, every 6 people die on the operating table during heart surgery.
Cardiopathy has been diagnosed more and more often in recent years. Experts say that the blame lies with the deteriorating environment and the consumption of unnatural products. In childhood, it can be stopped without fatal complications for the body if treatment is started in a timely manner. The basis of therapy is antiarrhythmic and magnesium-containing drugs and lifestyle correction. Severe cases require surgery.
Connective tissue dysplasia syndrome of the heart in children
In recent years, there has been an increase in the number of congenital malformations and hereditary diseases, as well as an increase in the prevalence of various variants of connective tissue dysplasia due to the deterioration of the environmental situation. According to modern concepts, connective tissue dysplasia syndrome is defined as an independent syndrome of a polygenic-multifactorial nature, manifested by external phenotypic signs in combination with dysplastic changes in connective tissue and clinically significant dysfunction of one or more internal organs (V. A. Gavrilova, 2002).
The term “cardiac connective tissue dysplasia” (CDTS) refers to an anomaly of tissue structure, which is based on a genetically determined defect in collagen synthesis. DSTS syndrome was identified as an independent nosological form at a symposium in Omsk (1990), dedicated to the problem of congenital connective tissue dysplasia. The problem of DSTS syndrome attracts attention due to the high risk of developing complications such as cardiac rhythm and conduction disturbances, infective endocarditis, thromboembolism of various vessels and sudden cardiac death.
The high frequency of DSTS syndrome in various diseases indicates the systemic nature of the lesion, which is associated with the “omnipresence” of connective tissue, which makes up the stroma of all organs and tissues.
Dysplastic heart is a combination of constitutional, topographical, anatomical and functional features of the heart in a person with connective tissue dysplasia (CTD). In Western literature, the term “myxoid heart disease” is used (Morales AB, Romanelli BEA, 1992), but this formulation is used mainly by foreign authors.
The incidence of dysplastic heart is 86% among individuals with primary undifferentiated DST (G. N. Vereshchagina, 2008).
According to modern concepts, DSTS syndrome includes prolapses of the heart valves, aneurysms of the interatrial septum and sinuses of Valsalva, ectopically attached chords of the mitral valve and many others.
The pathology is based on the inferiority of the extracellular matrix and its collagen structures.
A dysplastic heart is formed by:
I. Constitutional features - “drip”, “hanging” heart, its rotation around the sagittal and longitudinal axis.
II. Bone-vertebral dysplasia and deformities with compression, rotation, displacement of the heart and torsion of large vessels: according to Urmonas V.K. et al. (1983). Deformations of the chest and spine lead to the development of thoraco-phrenic syndrome, which limits the functioning of all organs of the chest.
III. Features of the structure of the heart and blood vessels:
- redundancy of tissue of the mitral, tricuspid and aortic valves;
- prolapse of the mitral valve leaflets (MVP) with regurgitation;
- myxomatous degeneration of leaflets, chords, valve ring;
- valvular-ventricular dissociation;
- bicuspid aortic valve;
- elongation, excessive mobility of the chordae;
- ectopically attached chordae;
- increased trabecularity of the left ventricle (LV);
- open oval window;
- aneurysm of the interatrial septum (small);
- dilatation of the sinuses of Valsalva;
- ventriculoseptal features of the LV: transient systolic ridge of the upper third of the interventricular septum (IVS), S-shaped bend of the IVS;
- tortuosity, hypoplasia, aplasia, fibromuscular dysplasia of the coronary arteries;
- coronary artery aneurysms;
- myocardial bridges;
- anomalies of the conduction system;
- expansion of the proximal part of the aorta, pulmonary trunk;
- aortic hypoplasia, borderline narrow aortic root, pulmonary trunk hypoplasia;
- systemic failure of the venous wall - varicose veins of the upper and lower extremities, pelvis, vulva, varicocele.
IV. Pathology of the respiratory system with a decrease in vital capacity of the lungs:
- diffuse and bullous emphysema;
- multiple fistulas;
- repeated spontaneous pneumothorax;
- bronchiectasis;
- cystic hypoplasia of the lungs.
Myxomatous degeneration of valves, chords, subvalvular structures is a genetically determined process of destruction and loss of the architectonics of collagen and elastic structures of connective tissue with the accumulation of acidic mucopolysaccharides in the loose fibrous layer. In this case, there are no signs of inflammation. It is based on a defect in the synthesis of type III collagen, which leads to thinning of the fibrous layer, the valves are enlarged, loose, redundant, the edges are curled, and sometimes fringe is detected. The primary locus of autosomal dominant myxomatosis in MVP is localized on chromosome 16. Morales AB (1992) identifies myxoid heart disease.
In population studies, the phenomenon of MVP was detected in 22.5% of children under the age of 12 years. In children with CTD, MVP is found much more often - in 45–68%.
Clinical manifestations of MVP in children vary from minimal to significant and are determined by the degree of connective tissue dysplasia of the heart, autonomic and neuropsychiatric abnormalities.
Most older children complain of short-term chest pain, palpitations, shortness of breath, a feeling of interruptions in the heart, dizziness, weakness, and headaches. Children characterize heart pain as stabbing, pressing, aching and feel it in the left half of the chest without any irradiation. They arise in connection with emotional stress and are usually accompanied by autonomic disorders: unstable mood, cold extremities, palpitations, sweating, and disappear spontaneously or after taking sedatives. The absence in most cases of ischemic changes in the myocardium according to a comprehensive examination allows us to regard cardialgia as a manifestation of sympathalgia associated with the psycho-emotional characteristics of children with MVP. Cardialgia with MVP may be associated with regional ischemia of the papillary muscles when they are excessively tense. Neurovegetative disorders are also associated with palpitations, a feeling of “interruptions” in the work of the heart, “tingling”, and “fading” of the heart. Headaches often occur during overwork, anxiety, in the morning before school starts and are combined with irritability, sleep disturbance, anxiety, and dizziness.
On auscultation, characteristic signs of mitral valve prolapse are isolated clicks (clicks), a combination of clicks with late systolic murmur, isolated late systolic murmur, holosystolic murmur.
The origin of the noise is associated with turbulent blood flow associated with bulging of the valves and vibration of the tense chords. Late systolic murmur is heard better in the left lateral decubitus position and intensifies during the Valsalva maneuver. The nature of the noise may change with deep breathing. As you exhale, the noise intensifies and sometimes takes on a musical tone. Often, the combination of systolic clicks and late murmur is most clearly detected in an upright position after exercise. Sometimes, when systolic clicks are combined with a late murmur in a vertical position, a holosystolic murmur may be recorded.
Holosystolic murmur with primary mitral valve prolapse is rare and indicates the presence of mitral regurgitation. This noise occupies the entire systole and practically does not change in intensity when changing body position, is carried out in the axillary region, and intensifies during the Valsalva maneuver.
The main methods for diagnosing MVP are two-dimensional Echo-CG and Dopplerography. MVP is diagnosed when the maximum systolic displacement of the mitral valve leaflets beyond the line of the mitral valve ring in the parasternal longitudinal position is 3 mm or more. The presence of isolated displacement of the anterior leaflet beyond the line of the mitral valve annulus in the four-chamber apical position is not enough to diagnose MVP; this is the main reason for its overdiagnosis.
Echo-CG classification of myxomatous degeneration (MD) (G. I. Storozhakov, 2004):
- MD 0 - no signs.
- MD I - minimally expressed: thickening of the leaflets 3–5 mm, arched deformation of the mitral orifice within 1–2 segments. The closure of the valves is preserved.
- MD II - moderately expressed: thickening of the leaflets 5–8 mm, elongation of the leaflets, deformation of the contour of the mitral orifice, its stretching, impaired closure of the leaflets. Mitral regurgitation.
- MD III - pronounced: thickening of the leaflets is more than 8 mm, the leaflets are elongated, multiple ruptures of the chords, significant expansion of the mitral ring, there is no closure of the leaflets. Multivalve lesion. Dilatation of the aortic root. Mitral regurgitation.
The degree of regurgitation in MVP depends on the presence and severity of myxomatous degeneration, the number of prolapsed leaflets and the depth of prolapse.
Degrees of regurgitation:
- 0—regurgitation is not recorded.
- I - minimal - the regurgitant jet penetrates into the cavity of the left atrium no more than one third of the atrium.
- II - medium - the regurgitation jet reaches the middle of the atrium.
- III - severe - regurgitation throughout the left atrium.
At rest, mitral regurgitation (MR) of the first degree is diagnosed in 16–20%, the second degree in 7–10% and the third degree in 3–5% of children with MVP.
The prognosis of a patient with MVP determines the degree of mitral regurgitation. Moreover, any degree of prolapse leads to changes in myocardial perfusion, changes most often in the area of the anterior wall of the LV and the interventricular septum (Nechaeva G.I., Viktorova I.A., 2007)).
Severe complications from MVP in children are rare. They are: life-threatening arrhythmias, infective endocarditis, thromboembolism, acute or chronic mitral regurgitation, and even sudden death.
Acute mitral regurgitation occurs due to the separation of the tendon threads from the cusps of the mitral valve (loppy mitral valve syndrome); it is rarely observed in childhood and is mainly associated with chest trauma in patients with myxomatous chordae degeneration. The main pathogenetic mechanism of acute mitral regurgitation is pulmonary venous hypertension, which occurs due to a large volume of regurgitation into an insufficiently distensible left atrium. Clinical symptoms are manifested by the sudden development of pulmonary edema.
In children, mitral regurgitation with MVP is most often asymptomatic and is diagnosed by Doppler echocardiography. Subsequently, as regurgitation progresses, complaints of shortness of breath during physical activity, decreased physical performance, weakness, and retarded physical development appear.
Risk factors for the development of “pure” (non-inflammatory) mitral regurgitation in prolapse syndrome according to two-dimensional echocardiography are:
- Dilatation of the left atrioventricular orifice.
- Prolapse of predominantly the posterior mitral leaflet.
- Thickening of the posterior mitral leaflet.
MVP is a high risk factor for infective endocarditis. The absolute risk of the disease is 4.4 times higher than in the population.
Diagnosis of infective endocarditis in MVP presents certain difficulties. Since the valves during prolapse are excessively scalloped, this does not allow us to detect the beginning of the formation of bacterial vegetations according to echocardiography. Therefore, the main importance in the diagnosis of endocarditis is played by: 1) clinical symptoms of the infectious process (fever, chills, rash, and other symptoms), 2) the appearance of the noise of mitral regurgitation and the fact of detection of the pathogen during repeated blood cultures.
The incidence of sudden death in MVP syndrome depends on many factors, the main ones being electrical instability of the myocardium in the presence of long QT interval syndrome, ventricular arrhythmias, concomitant mitral regurgitation, and neurohumoral imbalance.
The risk of sudden death in the absence of mitral regurgitation is low and does not exceed 2:10,000 per year, while with concomitant mitral regurgitation it increases 50–100 times.
In most cases, sudden death in patients with MVP is of arrhythmogenic origin and is caused by the sudden onset of idiopathic ventricular tachycardia (fibrillation) or against the background of long QT interval syndrome.
In rare cases, sudden cardiac death in patients with MVP may be due to a congenital anomaly of the coronary arteries (abnormal origin of the right or left coronary artery), leading to acute myocardial ischemia and necrosis.
Thus, the main risk factors for sudden death in children with MVP syndrome are: ventricular arrhythmias of grade III–V according to Lown; prolongation of the corrected QT interval more than 440 ms; the appearance of ischemic changes on the ECG during physical activity; history of cardiogenic syncope.
DSTS are one of the unfavorable factors predisposing to the development of arrhythmic complications in childhood and adolescence, including hemodynamically significant ones. In the structure of rhythm disturbances in children with DSTS, supraventricular extrasystole in pathological quantities and ventricular extrasystole, interrelated with the degree of cardiac dysplasia, are more often detected (Gnusaev S. F., co-authors, 2006).
Morphological manifestations of DSTS syndrome in children with concomitant kidney pathology, according to Domnitskaya T. M., Gavrilova V. A. (2000), are: spherical or triangular shape of the heart, rounding of the apex of the heart, an increase in heart weight by 1.4–2. 5 times, thickening and shortening of the mitral valve chords, fan-shaped discharge of the chords, hypertrophy of the papillary muscles, funnel-shaped mitral valve, open oval window. Myxomatous degeneration of the atrioventricular valve leaflets was observed in the majority of patients with DSTS syndrome and diseases of the urinary system (its frequency ranged from 66.7% to 77%). Endocardial fibroelastosis was detected in 10 children of the analyzed group.
In the population of children, the most frequently detected displacement of the septal leaflet of the tricuspid valve into the ventricular cavity within 10 mm, impaired distribution of chords of the anterior leaflet of the mitral valve, dilatation of the sinuses of Valsalva, enlarged eustachian valve more than 1 cm, dilatation of the pulmonary artery trunk, MVP, diagonally located trabeculae in the cavity left ventricle.
The management tactics for children with primary MVP vary depending on the severity of leaflet prolapse and the nature of autonomic and cardiovascular changes. The main principles of treatment are: 1) complexity; 2) duration; 3) taking into account the direction of functioning of the autonomic nervous system.
It is mandatory to normalize work, rest, daily routine, adherence to the correct regime with sufficient sleep.
The issue of physical education and sports is decided individually after the doctor evaluates the indicators of physical performance and adaptability to physical activity. Most children, in the absence of mitral regurgitation, severe disturbances in the repolarization process and ventricular arrhythmias, tolerate physical activity satisfactorily. If they have medical supervision, they can lead an active lifestyle without any restrictions on physical activity. Children can be recommended swimming, skiing, skating, and cycling. Sports activities associated with jerky movements (jumping, karate wrestling, etc.) are not recommended. The detection of mitral regurgitation, ventricular arrhythmias, changes in metabolic processes in the myocardium, and prolongation of the QT interval in a child dictates the need to limit physical activity and sports. These children are allowed to engage in physical therapy under the supervision of a doctor.
Treatment is based on the principle of restorative and vegetotropic therapy. The entire complex of therapeutic measures should be built taking into account the individual characteristics of the patient and the functional state of the autonomic nervous system.
An important part of the complex treatment of children with DSTS is non-drug therapy: psychotherapy, auto-training, physiotherapy (electrophoresis with magnesium, bromine in the upper cervical spine), water procedures, acupuncture, spinal massage. The doctor's attention should be directed to the sanitation of chronic foci of infection; tonsillectomy is performed according to indications.
Drug therapy should be aimed at: 1) treatment of vegetative-vascular dystonia; 2) prevention of the occurrence of myocardial neurodystrophy; 3) psychotherapy; 4) antibacterial prophylaxis of infective endocarditis.
For moderate manifestations of sympathicotonia, herbal medicine with sedative herbs, tincture of valerian, motherwort, herbal collection (sage, wild rosemary, St. John's wort, motherwort, valerian, hawthorn), which simultaneously has a slight dehydration effect, is prescribed. If there are changes in the repolarization process on the ECG, or rhythm disturbances, courses of treatment are carried out with drugs that improve metabolic processes in the myocardium (panangin, carnitine, Kudesan, vitamins). Carnitine is prescribed at a dose of 50 mg/kg per day for 2–3 months. Carnitine plays a central role in lipid and energy metabolism.
As a cofactor for beta-oxidation of fatty acids, it transports acyl compounds (fatty acids) across mitochondrial membranes, prevents the development of myocardial neurodystrophy, and improves its energy metabolism. In our studies, 35 children with extrasystole (more than 15 per minute) included carnitine in complex therapy. At the end of treatment, extrasystole decreased significantly in 25 children, and was not detected in 10 children.
A beneficial effect has been noted from the use of the drug Coenzyme Q10®, which significantly improves bioenergetic processes in the myocardium and is especially effective in secondary mitochondrial failure.
Early diagnosis of CTD in children allows for appropriate rehabilitation therapy and prevention of disease progression. One of the most striking therapeutic results is the effective treatment of children with DST (mainly with MVP) using the magnesium-containing drug magnesium orotate - Magnerot®. The choice of the drug was due to the known properties of the magnesium ion, observed in class I and IV antiarrhythmic drugs (membrane stabilizing and calcium antagonists), as well as the absence of side effects that may appear when using traditional antiarrhythmic therapy. It was also taken into account that the active ingredient of the drug is magnesium orotate, which, by inducing protein synthesis and participating in the exchange of phospholipids, which are an integral part of cell membranes, is necessary for the fixation of intracellular magnesium (O. A. Gromova, 2007).
The drug Magnerot® was used as monotherapy at a dose of 40 mg/kg per day during the first 7 days of administration, then 20 mg/kg per day for 6 months. The result of treatment was a decrease in the depth of prolapse of the mitral valve leaflets by 20–25% and a decrease in the degree of regurgitation by 15–17%. Treatment with Magnerot® did not affect the size of the left chambers of the heart and myocardial contractility, the values of which were within normal limits before treatment.
Studies conducted by E. N. Basargina (2008) revealed the antiarrhythmic effect of the drug Magnerot®. During daily ECG monitoring in children of groups 2 and 3, a decrease in the number of ventricular complexes by 50% or more was noted in 18 (27.7%) patients. Moreover, in 6 children, the disappearance of ventricular arrhythmia or a decrease in the number of ventricular complexes to 30–312 per day was noted. In 14 (21.5%) children, the number of ventricular complexes decreased by at least 30%. In two patients, an increase in the number of ventricular extrasystoles was noted up to 30% of the initial level. Thus, the antiarrhythmic effectiveness of Magnerot® was 27.7%. Similar results were previously obtained in other studies (Domnitskaya T. M. et al., 2005).
At the same time, rare supraventricular and ventricular extrasystoles, if not combined with long QT interval syndrome, as a rule, do not require the prescription of any antiarrhythmic drugs.
Thus, children with DSTS syndrome require timely diagnosis using Doppler echocardiography, electrocardiography, and in some cases 24-hour ECG monitoring, individual therapy, and monitoring by a pediatric cardiologist.
Therapy with Magnerot® in children with DSTS syndrome leads to a decrease in signs of valve prolapse, the frequency of detection of mitral regurgitation, a decrease in the severity of clinical manifestations of autonomic dysfunction, the frequency of ventricular arrhythmias, and is accompanied by an increase in the level of intraerythrocyte magnesium.
Literature
- Zemtsovsky E. V. Dysplastic syndromes and phenotypes. Dysplastic heart. St. Petersburg: "Olga". 2007. 80 p.
- Gavrilova V. A. Cardiac connective tissue dysplasia syndrome in children with diseases of the urinary system. Author's abstract. diss. Doctor of Medical Sciences M., 2002.
- Morales AB, Romanelli B., Boucek RJ et al. Myxoid heart disease: an assessment of extravalvular cardiac pathology in severe mitrae valve prolapse // Hum.Pathol. 1992, v. 23, no. 2, p. 129–137.
- Vereshchagina G. N. Systemic connective tissue dysplasia. Clinical syndromes, diagnosis, treatment approaches. Methodological manual for doctors. Novosibirsk, 2008, 37 p.
- Urmonas V.K., Kondrashin N.I. Funnel chest. Vilnius: Mokslas, 1983, 115 p.
- Gnusaev S. F. The significance of minor cardiac anomalies in healthy children and in cardiovascular pathology. Author's abstract. diss. Doctor of Medical Sciences, M., 1996.
- Belozerov Yu. M., Gnusaev S. F. Mitral valve prolapse in children. M.: Martis, 1995. 120 p.
- Storozhakov G.I., Vereshchagina G.S., Malysheva N.V. Assessment of individual prognosis for mitral valve prolapse // Cardiology, 2004, 4, p. 14–18.
- Nechaeva G. I., Viktorova I. A. Connective tissue dysplasia: terminology, diagnosis, patient management tactics. Omsk: Publishing house "Typography Blankom", 2007. 188 p.
- Gnusaev S. F., Belozerov Yu. M., Vinogradov A. F. Clinical significance of minor cardiac anomalies in children // Russian Bulletin of Perinatology and Pediatrics. 2006, no. 4. pp. 20–24.
- Domnitskaya T. M., Gavrilova V. A. Cardiac connective tissue dysplasia syndrome in children with diseases of the urinary system / Materials of the Second Congress of Pediatric Nephrologists of Russia. M., 2000. P. 159.
- Gromova O. A, Gogoleva I. V. The use of magnesium in the mirror of evidence-based medicine and fundamental research in therapy // Farmateka. 2007, v. 146, no. 12, p. 3–6.
- Basargina E. N. Cardiac connective tissue dysplasia syndrome in children // Issues of modern pediatrics. 2008, vol. 7, no. 1, 129–133.
- Domnitskaya T. M., Dyachenko A. V., Kupriyanova O. O., Domnitsky M. V. Clinical evaluation of the use of magnesium orotate in young people with cardiac connective tissue dysplasia syndrome // Cardiology. 2005; 45 (3): 76–81.
S. F. Gnusaev, Doctor of Medical Sciences, Professor
State Educational Institution of Higher Professional Education Tver State Medical Academy of Roszdrav , Tver
Contact information about the author for correspondence
Diagnostic methods
If cardiopathy is suspected in a child, the doctor conducts a careful examination and asks the parents about the presence of symptoms. The initial examination is performed by a pediatrician, but a more thorough diagnosis is carried out under the supervision of a cardiologist.
Pediatric cardiology uses the following methods to diagnose cardiac pathologies:
- Echocardiography. The study consists of examining the chest using an ultrasound machine. With its help, the specialist determines the parameters of the heart muscle and its structural elements. Another name for the procedure is cardiac ultrasound. The procedure allows you to identify dysplastic pathology without the use of other methods.
- ECG. An electrocardiogram records the electrical signals produced by the heart. The device records the heart rate, describes the physical condition of the heart, and indicates the presence of arrhythmic movements.
- Phonocardiography. This method is in addition to ultrasound and ECG. It allows you to record the noise that appears during the work of the heart muscle.
Additionally, the child may be prescribed blood tests to determine genetic abnormalities. In some cases, it is necessary to determine the cause of the pathology. To do this, he is given a referral for a general blood test, CT scan, and MRI.