Learn more about neurological diseases starting with the letter “T”: Toxic encephalopathy; Torsion dystonia; Traumatic encephalopathy; Peripheral nerve injuries; Transient global amnesia; Transient ischemic attack; Cavernous sinus thrombosis; Tuberculous meningitis; Brain tuberculoma; Tuberous sclerosis.
Cavernous sinus thrombosis: what is it?
The disease is caused by blockage of the cavernous venous sinus of the brain with a blood clot. The clinical picture includes cephalgia, redness of the eye area, swelling, disturbances of brain functions of III, IV, V cranial nerves, chemosis, exophthalmos, and occasionally focal neurological symptoms. When making a diagnosis, it is necessary to compare the anamnesis, clinical studies and neuroimaging methods. Therapy includes an integrated approach: antibacterial and antithrombotic drugs and medications aimed at eliminating symptoms. Surgery is possible.
Thrombosis in children
Possible causes of blood clot formation in children:
- thrombophilia - congenital deficiency of anticoagulant blood factors;
- leukemia, other oncological diseases;
- cutaneous fulminant purpura, disseminated intravascular coagulation syndrome (develops with severe intoxication, inflammatory diseases: pancreatitis, peritonitis, etc.);
- the presence of antiphospholipid antibodies, lupus anticoagulant, and other autoantibodies (antibodies to one’s own cells).
Episodes of blood clots in a child should prompt a serious examination to determine the cause.
Causes
In most cases, this disease is secondary. Independent nosology includes only 10-20% of cases. The etiofactors are:
- Lesions of the central nervous system of a non-infectious nature - open and closed craniocerebral injuries, neurosurgical interventions, cancerous brain tumors, metastases.
- Infectious lesions. First of all, pathologies of the nose and eye orbits - retrobulbar abscess, orbital phlegmon, furunculosis, otitis, rhinosinusitis, mastoiditis. The root cause may be bacterial encephalitis and meningitis. Sometimes fungal infections, generalized viruses and septicemia can provoke thrombosis of the cavernous sinus.
- Venous thrombosis and hemodynamic disorders. Their development is promoted by heart failure, dehydration, and antiphospholipid syndrome. Long-term use of a central venous catheter can be dangerous. This leads to the formation of thrombotic masses.
- Hormonal imbalance, which can be caused by long-term use of oral contraceptives, pregnancy, and the postpartum recovery period.
- Collagenoses. In this case, TCS is the primary symptom of systemic connective tissue diseases. These are Sjogren's syndrome, systemic lupus erythematosus, Behçet's disease.
- Congenital thrombophilia contributes to the occurrence of thrombosis. It is caused by genetic abnormalities.
Difficulties in diagnosing thrombosis of the cerebral veins (CV) and venous sinuses (SV) are associated with the variety of clinical manifestations, the localization of thrombosis, the rate of its development, and the cause of the disease [1–3]. The MV and dural sinuses contain about 70% of the blood flowing to the brain, however, thrombosis of the MV and VS is much less common than arterial thrombosis. The course of thrombosis of MV and VS is extremely variable - from progressive and recurrent to benign and curable [4].
This disease has been known for more than 200 years - the first description of thrombosis of MV and VS was made by J. Morgagni in 1761 [5]. In 1825, the French physician M. Ribes [6] described a patient with headache, epileptic seizure and delirium, who was found to have thrombosis of the MV and VS.
Large epidemiological and clinical studies are limited by the small number of patients with CF and VS thrombosis. Most publications about this disease are casuistic reports. Results from multicenter studies have only been published within the last 15 years, including the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVDST) [7], based on 624 observations. The Italian registry includes data from 706 cases of MV and VS thrombosis [8]. One of the latest retrospective studies [9], including 152 patients with MV and VS thrombosis, was conducted in 2021.
Epidemiology
To date, there are no epidemiological studies on MV and VS thrombosis, so the exact incidence rate is unknown. The first data on the incidence of MV and VS thrombosis were obtained from autopsy results. H. Ehlers and C. Courville [10] in 1936, summarizing the results of 12,500 autopsies, identified 16 cases of thrombosis of MV and VS, but data from modern studies [4] indicate that the incidence is 10 times higher.
The prevalence of MV and VS thrombosis is heterogeneous. In most patients, the disease develops between the ages of 20 and 50 years. Children and elderly people also get sick. In this regard, the epidemiology of the disease is separately described for different age groups. According to ISCVDST, the incidence of thrombosis of MV and VS in adults is 3-4 cases per 1 million, and in children and newborns - 7 cases per 1 million child population. Until the mid-60s, the incidence of thrombosis of MV and VS in men and women was considered equal, however, according to recent reports [7], thrombosis of MV and VS occurs more often in women, especially in the age group from 20 to 35 years (male: female ratio equals 3:1). The high prevalence of the disease in women of childbearing age is most likely associated with pregnancy, the postpartum period, and the use of oral contraceptives [11]. According to a study conducted in the USA in 1993-1994, about 12 births out of 100,000 are complicated by the development of MV and VS thrombosis [7]. An increase in the proportion of women among patients with MV and VS thrombosis over the past decade has been shown; currently it is about 70%. The predominance of female patients is explained by hormonal factors. About 1/3 of women of childbearing age in Western countries use oral contraceptives, which accounts for approximately ½ of patients with MV and VS thrombosis [12].
There are no reliable data regarding geographic or ethnic differences in incidence, but several studies have reported noteworthy results. In 2021, data from a study were published in the Adelaide region (Australia) with an adult population of about 1 million. In a retrospective analysis of all cases of MV and VS thrombosis for the period 2005-2011. the incidence was 15.7 cases per 1 million population per year; an almost equal distribution of patients by gender was found (52% women, 48% men) [13]. Prevalence of MV and VS thrombosis in the Netherlands in 2008–2010. amounted to 13.2 cases per 1 million population; to Hamadan (Iran) in 2009-2015. — 13.5 cases per 1 million population [12].
Localization
Thrombosis is more often localized in the dural sinuses than in the M.V. The most common thrombosis is the superior sagittal, sigmoid and transverse sinuses, and then - in descending order: thrombosis of the cortical veins, cavernous sinus, cerebellar veins. Thrombosis of the superior sagittal sinus occurs in 46% of cases, sigmoid or transverse sinuses - in 32%, several sinuses - in 20%, superior sagittal sinus and superficial cerebral veins - in 40% of cases [4]. In 2/3 of cases, thrombosis is not limited to one sinus, but spreads to adjacent sinuses and veins. Isolated thrombosis of the superior sagittal sinus is observed in 13-55% of cases, sigmoid and transverse sinuses - in 10%; in 40% of cases, sinus hypoplasia is observed, which is difficult to distinguish from thrombosis [14].
In a retrospective study by J. Liang et al. [15] the following data were obtained: thrombosis of the superior sagittal sinus occurred in 72.7% of cases, left transverse sinus - in 43.2%, left sigmoid sinus - in 43.2%, right transverse sinus - in 36.4%, right sigmoid - in 36.4%, straight sinus - in 9.1%. In 47.7% of cases, thrombosis of the MV and VS was accompanied by secondary changes in the brain (infarctions were detected in 43.2% of cases, hemorrhages in 27.3%). Most often, secondary changes were localized in the frontal (31.8%) and parietal (36.4%) lobes. Subarachnoid hemorrhages occurred in 13.6% of cases, subdural hematomas - in 4.5%.
L. Zhou et al. [16] revealed thrombosis of the transverse sinus in 65.0% of patients, sigmoid sinus in 55.6%, and superior sagittal sinus in 54.7%. Secondary brain changes were found in 56.4% of patients. Edema of limited areas of the brain was observed in 30.8% of patients, massive edema - in 4.3%, intracranial hematomas - in 15.4%, subarachnoid hemorrhages - in 4.3%.
Risk factors
The diseases that are most often associated with thrombosis of the MV and VS include infections of the orbital region, mastoiditis, inflammatory diseases of the middle ear and face, and meningitis. Inflammatory processes in the area of the mastoid process or face are a predisposing factor for the development of thrombosis of the transverse and sigmoid sinuses. Cavernous sinus thrombosis is caused by infections of the paranasal sinuses (ethmoid and sphenoid) [3, 4]. S. Imam et al. [17] described thrombosis of MV and VS in a 39-year-old patient with chickenpox.
Risk factors for the development of aseptic thrombosis of MV and VS are taking oral contraceptives, pregnancy, the postpartum period, traumatic brain injury (including mild), implantation of a pacemaker or prolonged standing of a subclavian venous catheter with its thrombosis, tumors, collagenosis (systemic lupus erythematosus, disease Behçet, Sjogren's syndrome), blood diseases (polycythemia, sickle cell anemia, thrombocytopenia), antiphospholipid syndrome, thrombophilia (most often caused by mutations in the factor V Leiden and prothrombin genes, deficiency of antithrombin III, protein C), nephrotic syndrome. A history of indications of episodes of increased blood clotting (deep vein thrombosis, thromboembolism of the arteries of the pulmonary trunk system, stroke, myocardial infarction, multiple miscarriages) suggests a state of primary hypercoagulation. Conditions accompanied by secondary hypercoagulation include late pregnancy, childbirth, and the presence of a brain tumor. Hemodynamic disturbances include dehydration, anemia, and congestive heart failure. Changes in the vascular wall can occur as a result of injury, brain tumor, or viral encephalitis [3, 4]. In some cases, a connection between MV and VS thrombosis and temporal arteritis, Wegener's granulomatosis [18] and Churg-Strauss syndrome [19] has been suggested.
In obstetric and gynecological practice, thrombosis of MV and VS mainly occurs in the postpartum period, especially during the first 3 weeks after birth. Risk factors for the development of the disease include dehydration, anemia, cesarean section, arterial hypertension, infectious diseases, maternal age (15-24 years), thrombophilia [4]. Thrombophilia accounts for 34.1% of all causes of thrombosis of MV and VS [4]. Most often we are talking about an abnormality of factor V, which gives it resistance to activated protein C; mutations of the antithrombin III genes and proteins C and S are less common. Thrombosis can also be caused by a deficiency of factors of the anticoagulation system of the blood and resistance of factor V to protein C. In addition, hyperhomocysteinemia predisposes to thrombosis. According to a study by Y. Kapessidou et al. [20], hereditary and acquired forms of thrombophilia were the cause of thrombosis of MV and VS in 64% (7 out of 11) of cases, including protein S deficiency detected in 4 patients, idiopathic thrombocytopenic purpura - in 2 patients (in one case associated with systemic lupus erythematosus, in another - with antiphospholipid syndrome).
Based on the results of several case-control studies [21–23] and one meta-analysis [8], there is a strong association between the use of oral contraceptives and the development of MV and VS thrombosis. The risk of thrombosis may vary depending on the composition of the drugs. Third-generation oral contraceptives are characterized by an increased risk of developing the disease [21], and the risk of its development when using contraceptive patches is similar to the risk when taking oral forms [24]. In approximately 1/3 of the cases cited in the literature, the etiology of MV and VS thrombosis remains unclear [4].
Clinical picture
The clinical picture of MV and VS thrombosis is variable. The average period from the onset of symptoms to diagnosis is 7 days [7]. The most common initial symptom of thrombosis of MV and VS is a sudden intense headache, which, as a rule, is diffuse and difficult to relieve with analgesics. Its course can be acute (less than 48 hours), subacute (from 48 hours to 30 days) and chronic (more than 30 days). Then, focal and general cerebral symptoms such as depression or confusion, epileptic seizures (usually partial with secondary generalization and post-attack paralysis), hemiparesis, aphasia, congestive optic discs, and mental disorders occur. Neurological symptoms in thrombosis of MV and VS most often develop subacutely, in a period from several days to 1 month (in 50-80%), although an acute onset can also be observed (in 20-30%) [25].
The International Headache Society has defined diagnostic criteria for headache in thrombosis of MV and VS:
A. New-onset headache that meets criteria C and D.
B. Thrombosis M.V. and VS diagnosed using neuroimaging methods.
C. Simultaneous development of headache, focal neurological symptoms and thrombosis of the MV and VS.
D. Headache that regresses within 1 month after the start of specific treatment.
With thrombosis of the MV and VS, venous congestion develops in the brain due to obstruction of venous outflow. Irritation of the receptors located in the wall of the MV and the interoceptors of the meninges with increased pressure in the venous system of the brain causes the appearance of headaches. Disruption of venous outflow leads to an increase in intracranial pressure and the development of hypoxia, resulting in necrotic changes in brain tissue. About 90% of patients describe persistent intense headache, more pronounced in the morning, as the main complaint with thrombosis of MV and VS. Typically, pain increases when the patient is in a horizontal position [25, 26].
Headache due to thrombosis of MV and VS has no specific features. Its clinical manifestations depend on the location and severity of thrombosis, the age of the patient, and the time from the onset of the disease. It is less common in elderly patients than in young patients, which may be due to a lower incidence of intracranial hypertension and decreased activity of the pain perception system in the elderly [26].
Headache due to thrombosis in 50% of cases has a subacute onset, intensifies over several days, but can be paroxysmal in nature. In 10% of cases, a thunderclap headache occurs. Gradually, the pain becomes persistent, refractory to painkillers and persists at night, intensifying with physical activity and the Valsalva maneuver.
Subjective characteristics of headache have no diagnostic value. Diffuse, predominantly bursting, headache is more common, and local pain is less common (42%). The intensity of pain is usually moderate or high. In most cases, headaches worsen at night and early morning, accompanied by nausea, vomiting and phonophobia. It can imitate migraine, tension headache, cervicalgia and is in no way related to the localization of the pathological process [27].
Headache may be a consequence of the chronic course of thrombosis of MV and V.S. Its peculiarity is that there are no indications of an acute episode of headache or the occurrence of neurological symptoms, however, MRI in the venosinusography mode reveals signs of thrombosis of one of the V.S. The predominant type is a bilateral headache of a pressing or bursting nature with a tendency to persist, aggravated by physical stress or emotional experience [2].
A prospective study examined headache characteristics in 123 patients with MV and VS thrombosis. Patients with intracranial hypertension and meningitis were excluded from the study. It was shown that in 14% of patients, headache was the only manifestation of the disease. In 88% of patients, thrombosis involved the transverse sinuses, and almost all (except one) cases of unilateral venous thrombosis had ipsilateral headache. Patients often characterized the headache as constant, one-sided, of high intensity and pulsating in nature. In most cases, patients noted a sudden onset of the attack; 3 patients described the “thunderous” nature of the headache. The pain syndrome regressed within several days or weeks after the start of treatment for MV and V.S. thrombosis. The prognosis was favorable in all cases. The authors suggested that the pathogenesis of headache in the absence of intracranial hypertension is associated with irritation of nerve endings in the walls of occluded MVs and VSs [28].
Swelling of the optic discs is observed in 45-86% of patients with thrombosis of the MV and V.S. The initial manifestations may be epileptic seizures, the frequency of which ranges from 10 to 60%. Focal neurological symptoms (paresis, dysarthria, visuospatial disturbances, homonymous hemianopsia) occur in 15% of patients [7, 27].
The results of a three-year clinical study of patients with MV and VS thrombosis showed that 60% (29 out of 48) of patients developed headaches: migraine (14), tension-type headache (13), other types of headache (2). Upon further evaluation (mean period 44 months), chronic migraine was diagnosed in 25% (6 of 24) of patients. Microhematomas were detected in most patients. In a study by R. Cumurciuc et al. [29] in 30% of patients with thrombosis of MV and VS, chronic headache was observed within 3 months. In a retrospective study by L. Zhou et al. [16], which included 117 patients with thrombosis of the MV and VS, it was shown that headache was observed in 87.2% of patients, epileptic seizures - in 31.6%, focal neurological symptoms - in 29.9%, visual disturbances - in 26.5%, disturbances of consciousness - in 15.4%.
Diagnostics
Due to the absence of pathognomonic clinical symptoms, instrumental research methods are of utmost importance in the diagnosis of MV and VS thrombosis. In recent years, the improvement of neuroimaging technologies has opened up new opportunities for diagnosing the disease (MRI, MRI and CT venosinusography). Under K.T. and MRI in standard modes can reveal cerebral edema, foci of necrotic changes in brain tissue, a filling defect in the area of confluence of sinuses (“delta sign”), as well as signs of venous thrombosis (increased signal intensity from an altered VS in T1 and T2 modes, and also T2-FLAIR) [2, 3, 30].
If after MRI or CT the diagnosis remains unclear, it is possible to perform digital subtraction angiography, which can detect not only VS thrombosis, but also the rare isolated MV thrombosis. Also, during digital subtraction angiography, it is possible to detect dilated and tortuous veins, which is an indirect sign of V.S. thrombosis. At the same time, a careful assessment of neuroimaging data is necessary to exclude diagnostic errors that may be caused, for example, by hypo- or aplasia of the sinuses [2, 3]. In a recent study by J. Kang et al. [31] it was shown that the ASL perfusion method with MRI allows diagnosing MV and VS thrombosis with high accuracy.
If hereditary thrombophilia is suspected, the level of homocysteine, the concentration and activity of antithrombin III, proteins C and S, and thrombophilic mutations are determined: mutations in the methylenetetrahydrofolate reductase gene - C 677 T
;
mutations in the blood coagulation factor V gene - G 1691 A
(factor V Leiden);
mutation in the prothrombin gene - G 20210 A
[2, 3, 25].
When taking oral contraceptives and liver disease, the concentration of all three factors of the blood anticoagulation system decreases simultaneously, and during pregnancy, primarily proteins C and S. With nephrotic syndrome, the concentration of antithrombin III decreases, and proteins C and S increase. Disorders of the anticoagulation system of the blood are far from the only cause of thrombosis of MV and VS: the disease can be caused by antiphospholipid syndrome and coagulopathy. The diagnosis is confirmed by the study of lupus anticoagulant, antibodies to cardiolipin and β2-glycoprotein, blood clotting factors, and determination of von Willebrand factor.
Treatment
The main goal of treatment for thrombosis of MV and VS is to restore their patency. According to various studies, the use of direct anticoagulants in the acute period of thrombosis of MV and VS improves the prognosis and reduces the risk of disability. The effectiveness of heparin in therapeutic dosage has been proven in double-blind, placebo-controlled studies. The hemorrhagic component in thrombosis of MV and VS is not a contraindication to the administration of heparin in a therapeutic dose. The initial dose of heparin is 5000 units and is administered intravenously as a bolus, after which they switch to intravenous drip administration at a rate of 1000 units/hour. The average daily dose of the drug is 20,000-40,000 units. Activated partial thromboplastin time should be monitored every 3 hours; it should be doubled compared to the norm. If the desired result cannot be achieved, the heparin dosage is gradually increased every 6-8 hours by 100-200 units. Upon completion of the acute phase of the disease, it is recommended to transfer the patient to oral warfarin. In this case, while the administration of direct anticoagulants continues, warfarin is prescribed under the control of the international normalized ratio (INR) (INR 2-3), then heparin is discontinued, and oral administration of warfarin is continued for 8-12 months [4, 32].
In the ISCVDST study [7], 80 patients out of 624 with MV and VS thrombosis received low molecular weight heparins. 79% of them recovered, 8% had mild symptoms, 5% had significant neurological impairment, and 8% died. These data indicate the effectiveness and safety of the use of low molecular weight heparins in the acute period of thrombosis of MV and VS.
J. Scott et al. [33] were the first to report the effectiveness of local thrombolytic therapy (TLT) for MV and VS thrombosis. Along with drug TLT [34], in recent years, for thrombosis of the MV and VS, instrumental methods of removing blood clots from the sinuses of the dura mater have been used - thrombectomy [35] and decompressive craniotomy [30].
Mortality
The mortality rate for thrombosis of MV and VS is 5-10% [5, 30]. The decrease in mortality is due to an increase in the quality of hospital care and improved diagnosis of the disease [36], as well as a decrease in the incidence of traumatic brain injuries and severe infectious diseases. The use of anticoagulant therapy and decompressive craniotomy had a positive effect on patient survival [12, 30].
Recurrent course
The incidence of recurrence of MV and VS thrombosis remains unknown. In a study by P. Palazzo et al. [37], which included 187 patients, the average follow-up period was 73 months, the average duration of anticoagulant treatment was 14 months. Repeated thrombosis of MV and VS was diagnosed in 6 patients, extracranial venous thrombosis - in 19. The rate of recurrence of venous thrombosis after 1 year was 3%, after 2 years - 8%, after 5 years - 12%, after 10 years - 18%. According to the results of the ISCVDST study [7], the incidence of recurrent thrombosis of MV and VS was 2.2%, extracranial venous thrombosis - 3%; the observation period was 16 months.
Forecast
When treatment is started in the early stages of MV and VS thrombosis, the prognosis is favorable in more than 90% of patients. In the absence of treatment for thrombosis of MV and VS, the prognosis is unfavorable in 15% of cases, mortality reaches 10%, but even with significantly pronounced neurological disorders, complete spontaneous recovery is possible. Risk factors for the development of an unfavorable prognosis of the disease are the rapid progression of thrombosis with depression of consciousness, generalized epileptic seizures at the onset of the disease, childhood and old age of patients, localization of thrombosis (cerebellar veins and deep MVs) [4, 7].
The authors declare no conflict of interest.
Development mechanism
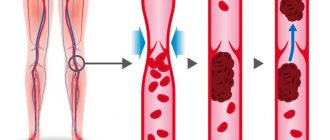
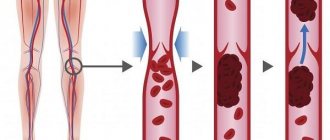
The pathogenesis of TCS is based on Virchow's triad:
- Damage to the walls of blood vessels.
- Slowing blood circulation.
- Increased blood viscosity.
This leads to local adhesion and clumping of platelets. In this way, a red or primary thrombus is formed. The large number of trabeculae in the cavernous sinus contributes to its growth and spread through the veins inside the skull.
Morphological changes are caused by blockage of regional veins and increased intracranial pressure. Intracranial blood flow is disrupted. Hydrostatic pressure increases. This leads to swelling of the brain. Due to stagnation of venous blood in the sinuses, the physiological absorption of cerebrospinal fluid begins to stop. Such circumstances increase the risk of hemorrhage or cerebral infarction.
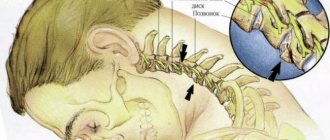
Neurological symptoms are determined by the topography and structure of the cavernous sinus. A group of cranial nerves, the sympathetic carotid plexus, and the carotid artery pass through the cavernous sinus.
Causes of development of thrombophlebitis and thrombosis of the sigmoid sinus and sepsis
The causative agents of thrombophlebitis and thrombosis of the sigmoid sinus are streptococcus, staphylococcus, pneumococcus and other bacteria.
Mixed bacterial flora predominates. Thrombophlebitis of the sigmoid sinus occurs most often through contact (due to an inflammatory process in the adjacent bone or perisinous abscess), much less often through the blood or lymph flow (hematogenous and lymphogenous through boils on the face).
The outer wall of the sigmoid sinus thickens and changes color. From blue, the wall of the sigmoid sinus becomes white or yellow-gray. Subsequently, granulation or necrosis occurs. If surgery is not performed in a timely manner, the inflammatory process spreads to the inner endothelial layer of the wall of the sigmoid sinus.
Damage to the endothelium and changes in the biochemical composition of the blood caused by invading microbes or their toxins in combination with a slowdown in blood flow lead to the formation of first a parietal and then an occlusive (clogging) thrombus (sigmoid sinus thrombosis).
Diagnosis: Magnetic resonance angiography of cerebral vessels is performed if thrombophlebitis of the sigmoid sinus is suspected.
Thrombosis of the sigmoid sinus is often limited, but it can sometimes spread retrogradely to the transverse sinus up to the confluence of the venous sinuses or even to the sinuses of the opposite side, and down to the bulb of the jugular vein and the jugular vein up to the innominate vein. The process of thrombophlebitis and thrombosis may spread to the upper and lower petrosal and cavernous sinuses.
The formation of a blood clot is a protective reaction to infection, but at the same time it is a dangerous complication of thrombophlebitis. With a low-virulent infection and good immunobiological reactions of the body, the blood clot can remain sterile (there are cases of an old blood clot being unexpectedly found in the sigmoid sinus on MRI of the brain (angiography) and in people who died from diseases not related to the ear). However, in the vast majority of cases, the blood clot becomes infected, often festeres and itself becomes a source of infection. With the blood flow, infected emboli or bacteria enter the pulmonary or systemic circulation.
In chronic otitis media, metastases of blood clots in the lungs predominate. Possible retrograde spread of the thrombus to the veins of the meninges flowing into the transverse sinus with the formation of an abscess in the cerebellum or occipital lobe of the brain. An abscess of the cerebellum or brain can also occur with a suppurating blood clot by destroying the inner wall of the sinus and spreading the process to the subarachnoid space and brain tissue.
Sepsis (“blood poisoning”) can develop as a result of the entry of a microbe through the sinus wall and without the formation of a blood clot (more often in acute otitis media). Finally, a form of sepsis that is caused by the entry of infection into the general circulation from multiple thrombosed small bone veins of the mastoid process (osteophlebitic pyaemia) is also very rare.
Anatomy of the ventricles of the brain with the designation of veins important during surgical interventions.
Clinical picture
Symptoms are variable. It depends on the rate of progression, the age of the patients and etiofactors. Includes:
- Headache without specific characteristics. If the root cause is infection, cephalalgia intensifies in a horizontal position.
- Nausea and vomiting.
- In some cases, hyperthermia and fever.
- Ophthalmological manifestations include pain when pressing on the periorbital areas, swelling, and tenderness of the eyeball. Possible bilateral or unilateral exophthalmos, chemosis, and sudden loss of vision.
- Swelling of the temporo-frontal region and cheeks, its redness or pallor.
- Violation of general condition. It can range from stunning to coma.
- Focal neurological symptoms include sensory aphasia, monoparesis, paralysis, generalized or focal epileptic seizures.
- Drooping of the upper eyelid.
- Restriction of eyeball movements.
- Loss of sensitivity in the area where the cranial nerves are innervated.
- Smoothness of the nasolabial fold.
- Various forms of strabismus.
Diagnostic methods
There are no pathogenetic symptoms of cavernous sinus thrombosis. This makes diagnosis difficult. It is necessary to distinguish the disease from sepsis, damage to the sigmoid sinus, retrobulbar hemorrhage, sarcoma and glioma of orbital tissue. To make a diagnosis, the following procedures are necessary:
- Examination and history taking.
- Checking neurological status. In this case, depression of the cranial and pupillary reflex, exophthalmos, hypoesthesia, and bulbar disorders are noted. Central paresis, strabismus, and positive meningeal signs are possible.
- A consultation with an ophthalmologist is indicated. The specialist can detect loss of visual fields, chemosis, blurred boundaries of the optic nerve head, and dilation of the venous vessels of the fundus.
- A blood test shows neutrophilic leukocytosis, anemia and increased ESR, thrombocytopenia.
- When collecting a lumbar puncture, an increased level of protein, leukocytes and red blood cells in the cerebrospinal fluid is detected. In a third of patients, this examination reveals nothing.
- CT scan reveals narrowing of the cerebral ventricles and cisterns, areas of increased density. The thrombus can be visualized using contrast.
- MRI is the most informative examination.
You can find out the addresses of diagnostic centers in the capital through the website “Unified CT/MRI/Ultrasound Recording Center in Moscow”. Here is the price list for diagnostics and patient reviews.
Diagnosis and treatment of thrombosis in Medical
Specialists from the Paracelsus Medical Center will help in diagnosing and eliminating this pathology, provide support during the rehabilitation period, and give recommendations for further prevention.
Our center uses expert-class equipment from leading global manufacturers for diagnosis and treatment. The consultation is conducted by practicing phlebologist surgeons.
On the basis of "Operating Room No. 1" phlebological operations are performed for venous disease. The key advantage of the Paracelsus Medical Center network is highly qualified professional surgeons with extensive practical experience.
Drug treatment
The basis of drug therapy is anticoagulants (thin the blood, prevent the growth of a blood clot), fibrinolytics and thrombolytics (dissolve existing clots), antiatherosclerotic drugs (lower cholesterol levels). If necessary, analgesics, anti-inflammatory drugs, cardiotonic drugs, vitamins, minerals, etc. may be needed as symptomatic therapy.
Surgery
There are such methods of surgical treatment of the disease:
- thrombectomy ー removal of a blood clot;
- stenting (expansion using a frame) and shunting (creating a bypass path for blood flow) for atherosclerotic artery disease;
- arteriovenous shunting.
If the thrombus cannot be removed, a vena cava filter can be installed - the device is placed in the vein above the level of blockage to prevent it from moving and closing the lumen of the vessels of vital organs.
Therapy
The main goal is to prevent the increase in intracranial hypertension. It is necessary to restore blood flow and suppress inflammatory processes. We need to prevent a relapse. If the primary pathology is of bacterial origin, antibiotics are indicated. An integrated approach includes:
- Antithrombotic drugs with gradual withdrawal of anticoagulants. Dipyridamole and aspirin can be used on an ongoing basis.
- Antibacterial therapy includes long-term administration of submaximal and maximum doses of broad-spectrum antibiotics. If the etiofactor is rhinusogenic, therapy affecting the anaerobic microflora is necessary.
- Treatment and direction to relieve symptoms allows you to stop convulsive seizures and fight cerebral edema. For maximum effect, it is recommended to combine anticoagulants with NSAIDs.
- In case of breathing disorders, it is possible to transfer the patient to mechanical ventilation with hyperventilation.
Surgical intervention
There can be two types: sanitation of foci of infection and removal of a blood clot or elimination of primary surgical diseases. The decision to undergo surgery is made only after conservative therapy and antibiotics. In case of translocation of intracranial structures that can damage the brain stem, emergency decompressive hemicraniectomy is necessary.
Preventive measures
There is no specific prevention of the disease. The risk of disease can be reduced by early detection and treatment of pathologies – etiofactors and coagulopathies.
Literature:
- Dubovitskaya Yu. I., Maksimova M. Yu., Bryukhov V. V., Krotenkova M. V. / Diagnosis of thrombosis of the cerebral veins and venous sinuses // Breast Cancer - 2017 - No. 21.
- Kryukov A. T., Palchun V. T./ Otorhinolaryngology // 2001.
- Izaeva T. A., Feigin G. A./ On the classification and treatment of phlebitis and thrombosis of large veins of the face and cavernous sinus of rhinosinusogenic origin // Russian Rhinology - 1996 - No. 5.
Risk factors for thrombosis
The following factors increase the likelihood of developing the disease:
- age over 50 years;
- obesity;
- smoking, alcoholism, drug addiction;
- poor nutrition;
- sedentary lifestyle;
- injuries;
- the need for frequent intravenous injections and procedures associated with violation of the integrity of blood vessels (blood sampling, hemodialysis, installation of a venous catheter) increases the risk of developing phlebitis and inflammation of the venous wall.